Health
Vol.5 No.6A2(2013), Article ID:33172,8 pages DOI:10.4236/health.2013.56A2008
Patient-centered care through internal and external participation in medical rehabilitation
![]()
Department of Medical Psychology and Medical Sociology, University of Freiburg, Freiburg, Germany; mirjam.koerner@mps.uni-freiburg.de
Copyright © 2013 Mirjam Körner. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received 16 April 2013; revised 17 May 2013; accepted 4 June 2013
Keywords: Patient-Centeredness; Participation; Rehabilitation; Shared Decision-Making; Teamwork
ABSTRACT
Patient-centeredness is one of the most important quality and outcome criteria in health care. Health care organizations are continually searching for approaches that will enable them to establish sustainable patient-centeredness in their daily practice. Existing approaches frequently focus on interaction between patient and health care professional (external participation). However, this is often not sufficient; other elements, such as good teamwork among the health care professionals (internal participation), are also essential. The model of integrated patientcenteredness differentiates between these two participations forms, both of which are explored from a patient and health care professional perspective in our study. The aim of the study was to confirm the model from the viewpoint of staff and patients. To this end we conducted a multi-center cross-sectional study consisting of a patient and staff survey to assess internal and external participation and patient-centeredness. A total of 15 rehabilitation clinics were involved, with 272 staff members and 536 patients included in the final analysis. Although evaluation was positive (mainly slightly above the middle of the scale), there was potential for improvement for both types of participation. Internal and external rating differed between patients and health care staff, with the first group assessing internal significantly better and external lower than the second group. The low to middle correlation of both types, as well as the correlation and regression with patient-centeredness, confirmed the model of integrated patient-centeredness. The model underlines the importance of both participation forms for patient-centeredness, as well as their interdependence. Further studies are needed in order to verify the impact of internal and external participation, as well as that of further possible dimensions of patientcenteredness, on clinical and functional outcome criteria.
1. INTRODUCTION
Patient-centeredness is one of the most important quality and outcome criteria in health care. There are different concepts of the dimensions of patient centeredness [1-7]. Some focus only on the patient and physician and their interaction [5-7], while other broader concepts take into account structural and organizational aspects such as access to care, coordination and continuity, information technology, interprofessional teamwork etc. [2,4,8,9].
The model of integrated patient-centeredness [8] differentiates between internal and external patient-centeredness in order to consider patient-health care professional interaction as well as organizational aspects. External patient-centeredness can thereby be described as a patient relationship focused on patient needs and preferences and with the primary aim of enabling patient expectations. In contrast, internal patient-centeredness refers to in-house conditions, e.g. interprofessional teamwork or clinic culture, that enable delivery of a continuous strategy aimed at the expectations of patients (external clients) [9]. The key feature of both forms is participation (see Figure 1).
External participation is defined as patient participation in decision-making, e.g. treatment planning, goal setting in the patient-professional encounter. The “shared decision-making (SDM)” approach is promoted as the ideal interaction model for implementing external par-
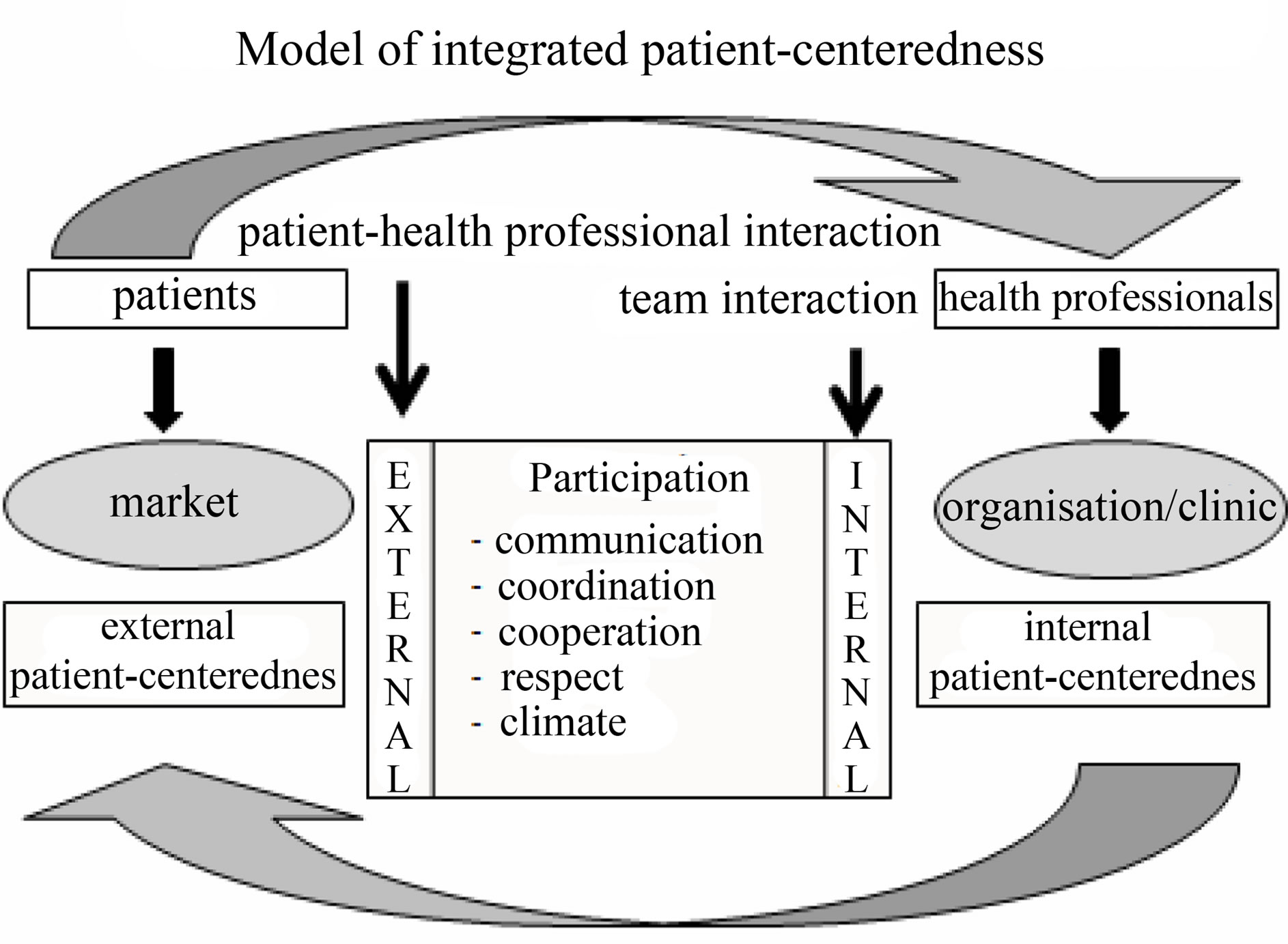
Figure 1. Model of integrated patient-centeredness [8,9].
ticipation in patient-professional interaction [10-12]. Shared decision-making can be defined as sharing medical and personal information in a reciprocal communication flow, discussing of wishes, options and preferences, and a mutual deliberation and decision-making process with the patient [13-16]. Expected effects of SDM are, for example, higher compliance, treatment acceptance and patient satisfaction, improved functional status, higher quality of life and improvement in medication adherence, as well as a reduction of decision conflicts, anxiety and medication costs [17-24]. Most patients who have to make a healthcare decision prefer SDM [25,26].
Internal participation can be defined as patient-centered interprofessional teamwork within the clinic. It focuses on communication, coordination, cooperation, respect and climate within the interprofessional team in the patient treatment planning and process. Medical rehabilitation in Germany mostly takes place as in-patient measures in special rehabilitation clinics. This treatment is based on a holistic approach and requires different health care professionals working together in a team. The teamwork process brings these different professions, assessments and evaluations together to obtain a holistic view of the patients’ problems. Teamwork is therefore a key feature of the work in medical rehabilitation and a precondition for effective patient treatment [27-30]. Effective teamwork is accompanied by enhancement of treatment outcomes [31-33], reduction of morbidity [34], increase in patient [31,32] and employee [35] satisfaction and reduction of costs [32,33].
The model of integrated patient-centeredness is the first to combine both participation forms as the main dimensions. The aim of the study was to confirm this model by assessing staff and patient perception of internal and external participation, interdependence of these two elements, and whether there is an association with patient-centeredness.
2. METHODS
The study formed a part of the larger research project “Development and evaluation of a shared decisionmaking training program in medical rehabilitation”, funded as part of the German grant program “Chronic illness and patient orientation”, and was supported by the German Federal Ministry of Research and Education and the German Statutory Pension Insurance Scheme. The study was approved by the Ethics Committee of the University of Freiburg in Germany.
Twenty-two in-patient medical rehabilitation clinics in southwest Germany originally expressed interest in the study; of these, fifteen took part in the patient and staff survey. Each clinic determined a contact person (mostly senior physician or psychologist) responsible for the study process: all surveys were then sent to this contact person, who distributed them to the patients and health care professionals in the treatment team.
Inclusion criteria for patients were: chronic disease(s), treatment in inpatient rehabilitation, age > 18 years, sufficient German language abilities, no cognitive impairments and signed informed consent.
Physicians, nursing staff, therapists of the psychosocial department (such as psychotherapists, social workers, art, occupational and music therapists), and therapists of the physiological department (such as physiotherapists, masseurs, sport, exercise and nutrition therapists, dieticians) constitute the medical rehabilitation teams and were included in the staff survey.
All surveys were anonymous and participation was optional for patients as well as for staff members. After completing the survey the patients put it and the signed letter of consent in the envelope provided and returned it to the study coordinator, who collected the envelopes and sent them back to us. The staff sent the questionnaire direct to our research team in a pre-paid addressed envelope.
2.1. Instruments
The questionnaire pack for the patients and for the staff contained standardized questionnaires. Table 1 provides an overview of assessment required for this study.
The 9-item Shared Decision-Making Questionnaire (SDM-Q-9) [36] is a standardized brief patient-report instrument for assessing shared decision-making. It is psychometrically tested and can be used for the measurement of external participation from the patient’s perspective. The questionnaire contains nine five-step items, relating to the nine steps of the SDM model [36]. The authors of the instruments recommend compiling a standardized total value over the nine items, which is calculated by multiplying the mean of all items by 20/9, giving a range of 0 (no participation) to 100 (maximal par-
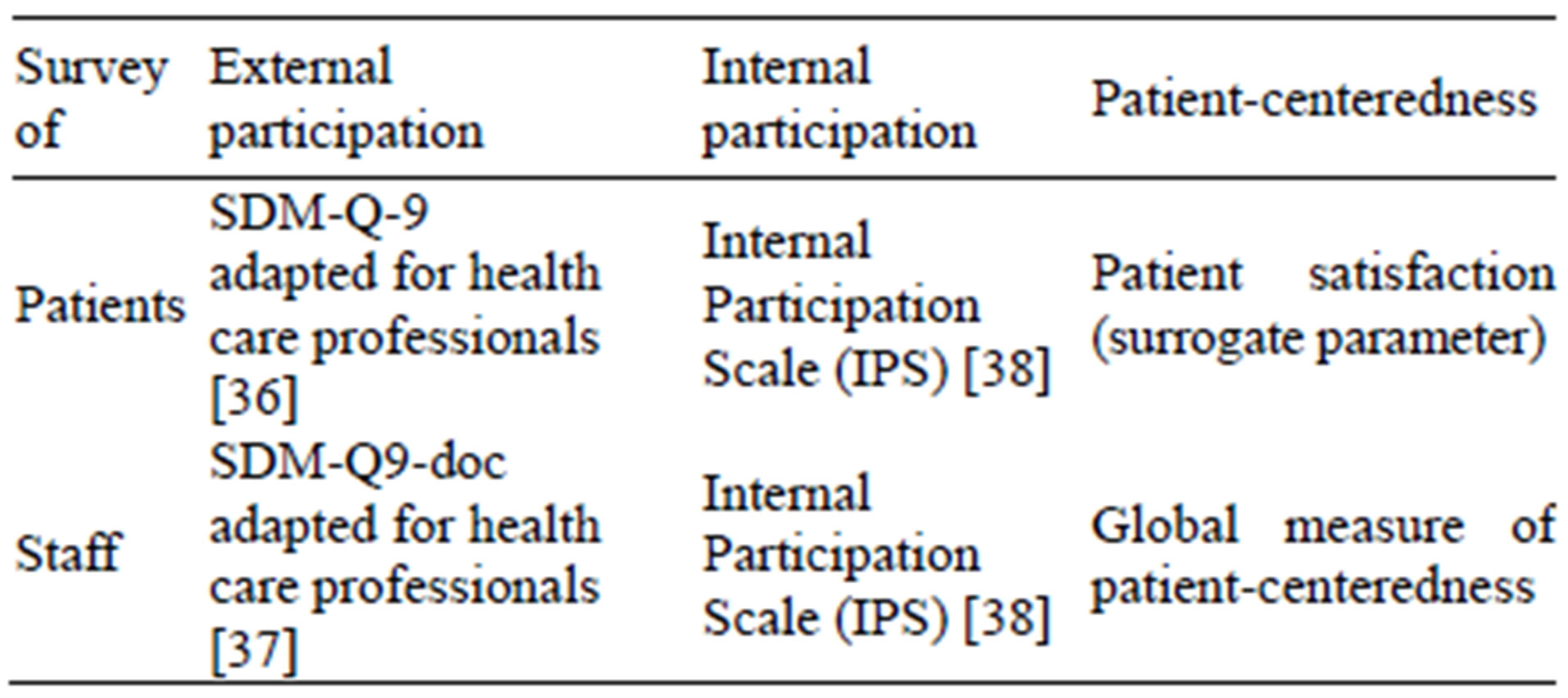
Table 1. Assessment of internal and external participation as well as patient-centeredness.
ticipation) [36]. The total score should not be calculated if two or more items are missing. We used a slightly modified version, replacing “physician” in the nine questions with “health care professional” and not asking for a specific decision-making situation, and therefore captured involvement in decision-making in a more general manner. The psychometrical criteria in our study were checked and were comparable with those in the original version.
The 9-item Shared Decision-Making Questionnaire doctor version (SDM-Q-9 doc) [37] was also modified to assess external participation, or rather the implementation of SDM from the health care professional perspective. Calculation of the standardized total value is identical to the SDM-Q-9 (see above). Psychometric properties of the adapted instrument were tested with the sample and were also comparable with the original SDM-Q9 doc [37].
The Internal Participation Scale (IPS) [38] was developed in this study in order to measure interprofessional patient-centered participation from a patient and staff perspective. The scale can be used for both groups, and consists of six items on climate, communication, coordination of treatment, coordination of professionals, cooperation and respect. The item scales have four steps and range from 1 (does not apply at all) to 4 (fully applies). The raw scores were also transformed to a standardized value range from 0 (minimal participation) to 100 (maximal participation) in order to compare internal and external participation. The main psychometric criteria were tested and are acceptable to excellent [38].
The global item of patient-centeredness (“In my point of view the clinic is patient-centered”) is assessed on a five-point Likert scale (1 = fully applies, 2 = generally applies, 3 = undecided, 4 = does not generally apply, 5 = does not apply at all), or the professionals can also tick “I can’t judge this”.
In the patient survey, “patient satisfaction” was used as a surrogate parameter to measure patient-centeredness, applying the established and validated “Questionnaire on Patient Satisfaction” [39,40]. This instrument is a selfrating instrument for inpatient settings designed on the basis of the American “Client Satisfaction Questionnaire CSQ-8” [41]. Based on eight 4-point Likert-scaled items (e.g., “Did you receive the type of treatment that you wished?”), the questionnaire assessed general patient satisfaction [41]. High scale values mark high patient satisfaction.
2.2. Data Analysis
Prior to data entry, quality was tested by verification of random samples, the items were further checked for plausibility, and missing data analysis was performed. Questionnaires with more than 30% of items unanswered (missing data) were excluded.
The survey data were evaluated with the IBM Statistical Package for Social Science (SPSS Version 21). Descriptive statistics, t-Test for paired samples (comparing internal and external participation within the staff or patient survey) and univariate analysis of variance with the factor “group” (patient or staff) and dependent variable “participation” (internal or external) were used for data analysis. Bivariate correlation coefficient between internal and external participation and patient-centeredness were calculated to judge interdependence and association with patient-centeredness in general. Additionally, a linear regression analysis checked the impact of internal and external participation on patient-centeredness.
3. RESULTS
3.1. Samples
A total of N = 1419 questionnaires were distributed to patients, with N = 662 completed and returned (response rate = 46.6%). After missing data analysis, a total of 536 complete data sets were included. Table 2 provides a description of the patient sample.
The average age of the patient sample was 52.7 years (range 18 - 90, SD = 13.7), with more men (62.3%) than women (36.9%) participating, and mostly Germans (93%). While 43.5% registered a low educational level, 33% had reached a medium and 19.8% a high level. Almost half of the patients were employed, 24.6% were retired and 17.2% were unemployed. Nearly two thirds of the patients were treated in somatic rehabilitation clinics (64.6%) and slightly more than one third in psychosomatic rehabilitation clinics (34%).
Of 661 questionnaires allotted to health care professionals in the rehabilitation teams, 275 came back (rate of return: 41.6%). Three questionnaires were excluded as a result of missing data analysis (more than 30% in the whole questionnaire), giving a total of 272 staff surveys for the analysis.
Table 3 displays the sample characteristics of the staff survey. In contrast to the patient sample, more females (60.3%) than males (34.6%) participated here. About two

Table 2. Description of patient sample (N = 536).
thirds (62.5%) of the staff were aged between 36 and 55. All health care professionals were represented in the sample: 18% physicians, 187.6% nurses, 24.6% psychosocial therapists, 18.4% physical and sports therapists and 13.6% other professional groups. Approximately 70% of the employees had worked more than five years in the clinic.
3.2. Internal and External Participation
Patient perception of internal and external participation differed significantly (T = 18.839, df = 456, p < 0.001), while professional perception (T = −0.0590, df = 261, p = 0.556) did not. Staff perception of internal and external participation was nearly identical and a little higher than the middle of the scale. Patients also rated external participation in the middle of the scale, but internal participation much higher (see Table 4). Patient perception of external participation was significantly lower than that of staff (F = 17.903, p < 0.001, partial Eta-square: 0.022). In contrast, staff evaluated internal
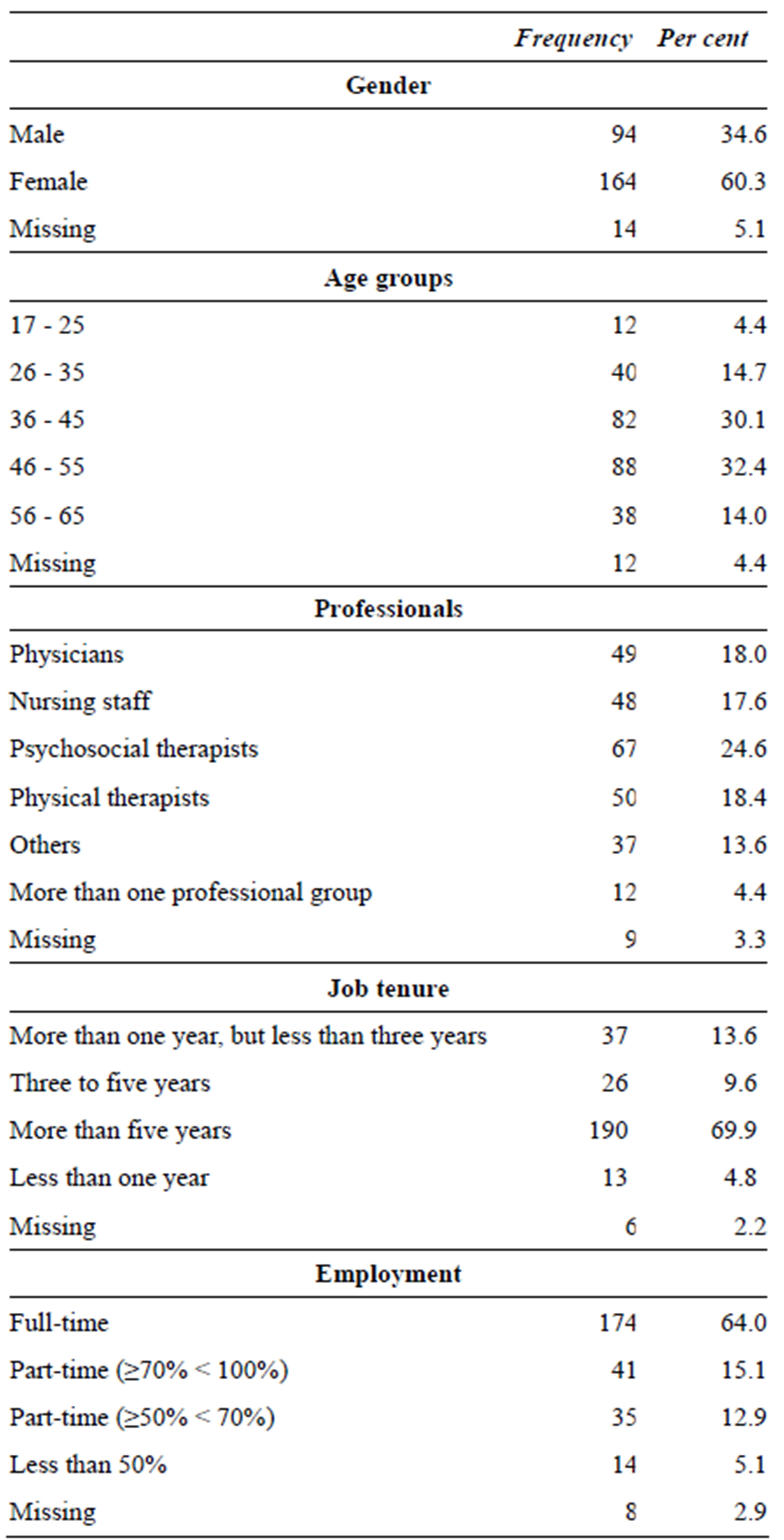
Table 3. Description of staff sample (N = 272).
participation considerably less favorably than the patients did (F = 139.128, p < 0.001, partial Eta-square = 0.155).
The participation forms correlated low to middle with each other. Correlation with patient-centeredness is higher for internal participation than for external participation (see Table 5). Correlation of internal and external participation with patient-centeredness in the staff survey is negative because the global item for patient-centeredness here is scaled inversely, with low values corresponding with high patient-centeredness.
A regression analysis of both participation forms showed that for both perspectives (staff and patients), internal participation is a more important predictor for

Table 4. Participation forms (Mean and Standard deviation).
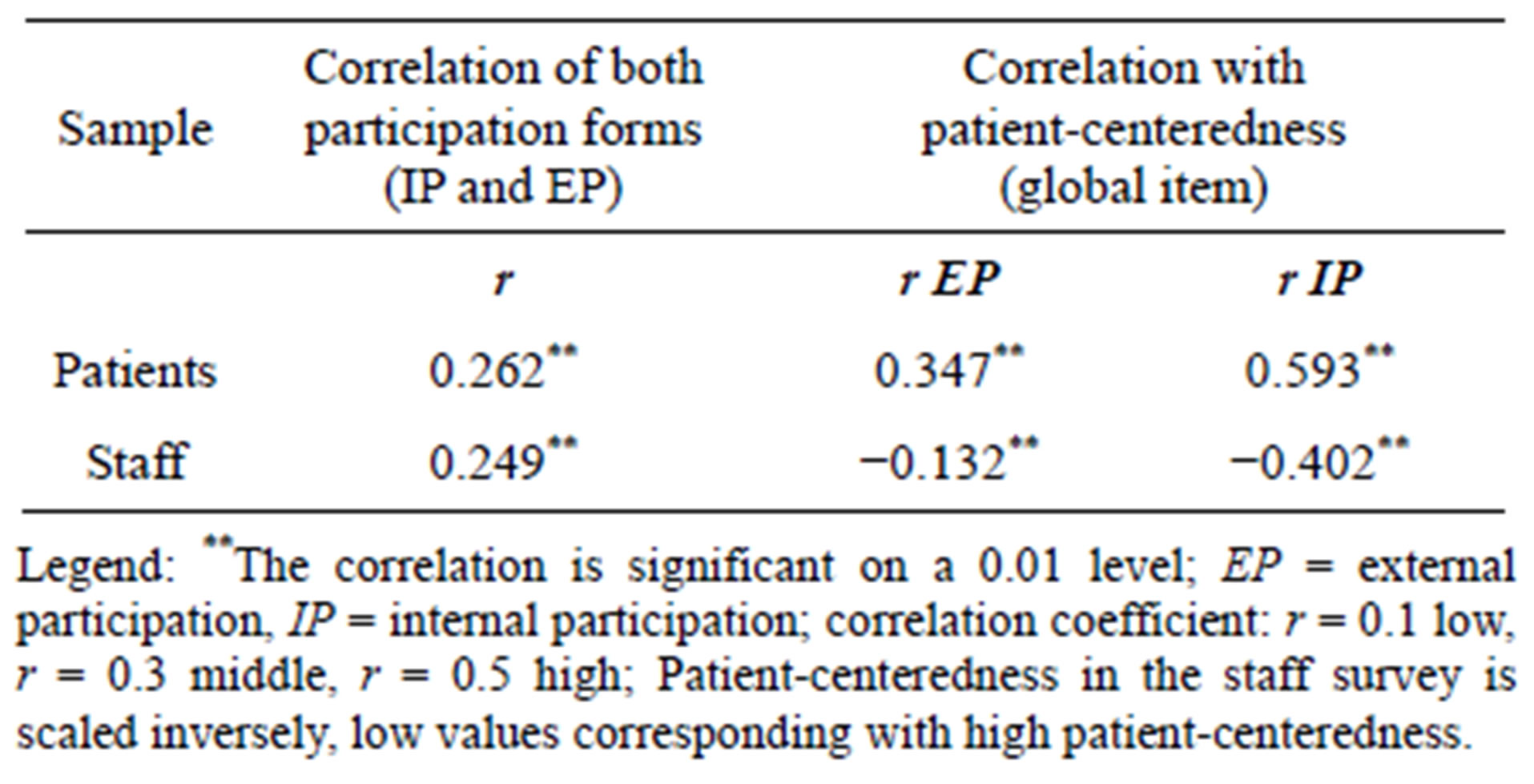
Table 5. Correlation coefficients for internal and external participation and patient-centeredness.
patient-centeredness than external participation (see Tables 6 and 7). The explained variance of patient-centeredness is 16.3% for the staff data and 39.1% for patients. The standardized beta regression coefficient is negative in the staff perspective (see Table 6) because the global item for measuring patient-centeredness is scaled inversely in comparison with the scales for internal and external participation.
4. DISCUSSION
The results for internal and external participation are positive, but there is still potential for improvement for both forms. The health care professionals judged them almost identically in contrast to the patients, who evaluated internal participation significantly better than external. The low to middle correlation of the participation forms confirmed the interdependence between them. This interdependence is also underlined in the model of integrated patient-centeredness. The association of internal and external participation to patient-centeredness can be seen as a further confirmation of the model. Internal participation is perceived to be the more important predictor for patient-centeredness by both patients and staff, although the patients rate both forms significantly.
Since the data (correlation and regression analysis) confirms the model, it seems to make sense to integrate both participation forms into one model. References found in the literature also corroborate this. Patienthealth care professional interaction and the proactive team are the key features of the chronic care model and
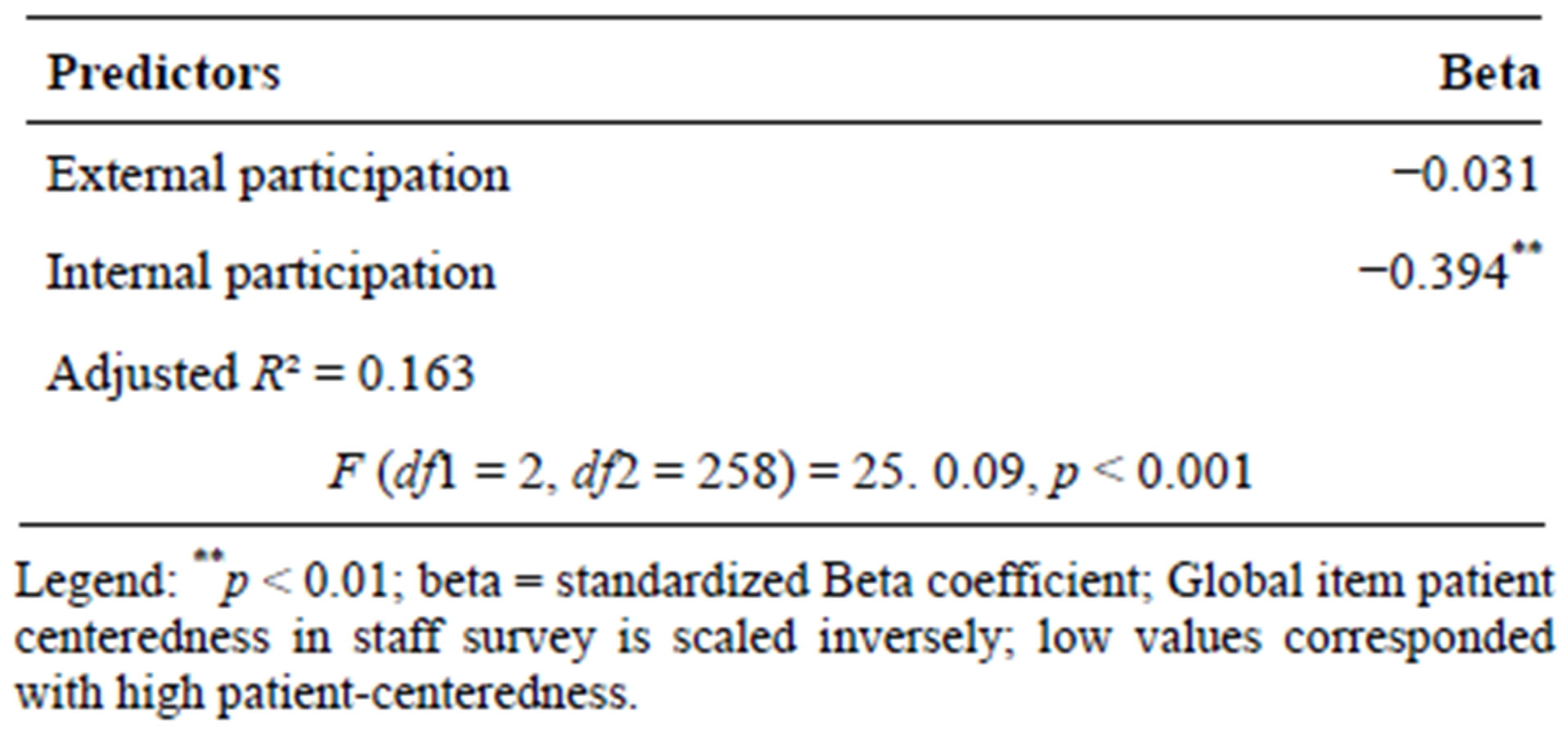
Table 6. Impact of internal and external participation on patient-centeredness—staff perspective (regression analysis).
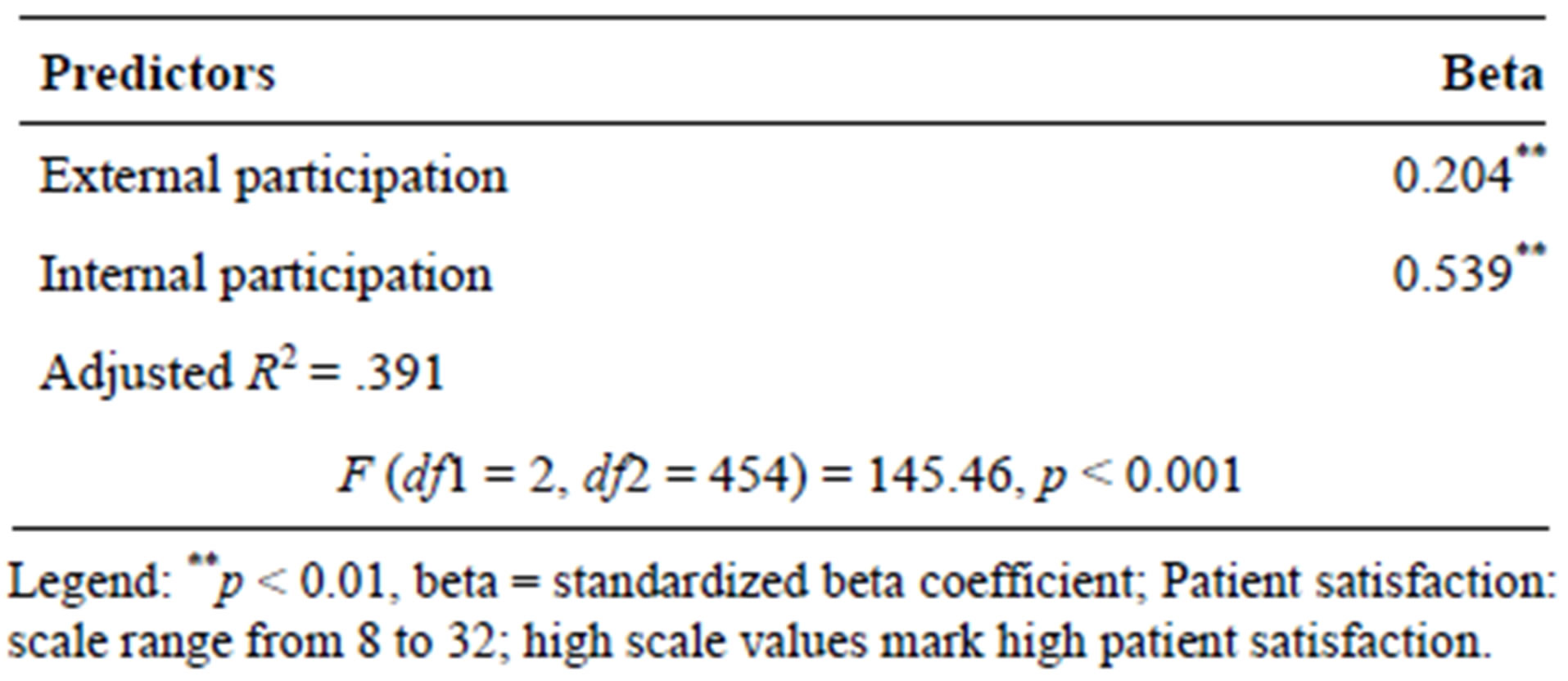
Table 7. Impact of internal and external participation on patient-centeredness—patient perspective (regression analysis).
predict clinical outcome [42-44]. An interprofessional approach to shared decision-making developed by a Canadian research group combined interprofessionalism and shared decision-making [45-48], while Green et al. [4] mentioned the importance of the team as one interpersonal dimension besides communication and knowing the patient.
Surprisingly, internal participation correlated higher with patient-centeredness than external and was the more important predictor in the regression analysis. A structural equation model using the data of the larger research project likewise showed that internal participation is the strongest predictor for treatment acceptance and patient satisfaction [49]. Further studies also underpin the importance of considering the interprofessional team and their collaboration for a patient-centered approach [35, 50-52].
Meanwhile it is known from studies on inter-rater agreement that there is a difference between self-rating and rating by others e.g. [53], therefore it seems important to consider the patient and health care professional perspective. The reason for the better patient evaluation of internal participation compared to staff rating could be that the quality of interaction in the team is not visible for them, as they are not part of the team. This is supported by the remarkable number of patients who ticked the box “I can’t judge this” for the Internal Participation Scale (IPS) items relating to communication (15%) and respect (12.3%) [38]. Overall, it appears that the evaluation is influenced when someone is directly affected. For example, the patients are directly affected by external participation, which they rated lower, indicating a need for improvement. Health care professionals are directly affected by internal participation, and expressed a higher potential for improvement there. The training program which was developed in the context of the larger research project mentioned above considers both participation forms in two independent modules [10,54], and with the benefit that it can be tailored to the needs of each clinic.
Some methodical limitations of the study should be considered. The study sample may suffer from selection bias caused by representatives possibly not reaching all patients in the clinics, or not all staff, which might explain the low to middle average rate of return for the surveys. Since surveys were voluntary, we mainly reached motivated patients and staff. This led to restrictions regarding the generalizability of the results. There was also a lack of external criteria for patient-centeredness; a global item was therefore applied to assess patient-centeredness in the staff survey and a surrogate parameter used to measure patient satisfaction in the patient survey. This fact limited the validity of the study.
However, the study has confirmed the model of integrated patient-centeredness as well as the importance of considering both participation forms for assessing it. The low to middle correlation of internal and external participation showed the interdependence of them, as well as their independence.
The regression analysis demonstrated the importance of both participation forms as predictors of patient-centeredness. There is a potential for more explanation of variance of patient-centeredness, indicating that more dimensions exist and need to be taken into account. Recent studies on the dimensions of patient-centeredness mention structural dimensions such as information technology or access to care, clinical dimensions, e.g. types of encounter, and interpersonal dimensions such as communication, knowing the patient [4], or starting from the patient situation, legitimizing the illness experience, acknowledging the patient’s expertise, offering realistic hope, developing an ongoing partnership and providing advocacy for the patient in the health care system [5]. Further studies should explore the additional dimensions of patient-centeredness and the impact of these on clinical and functional outcome parameters.
5. ACKNOWLEDGEMENTS
The study was a part of a research consortium on patient-centeredness and chronic diseases funded by the German Ministry of Education and Research and the German statutory pension insurance scheme (project number: 01GX720).
We would like to thank all patients and health care professionals in the rehabilitation clinics who supported the study (AOK-Klinik Korbmattfelsenhof, AOK-Klinik Stoeckenhoefe, Askepios Triberg, DAKHaus Schwaben, Klinik Bad Herrenalb GmbH, Kliniken Dr. Voetisch, Kurpark-Klinik, Neurologisches Rehabilitationszentrum Quellenhof, Rehabilitationsklinik Birkenbuck, Rehabilitationsklinik Gloecklehof, Rehabilitationsklinik St. Landelin, Reha-Zentrum Todtmoos, Rheintalklinik, Rehabilitationsklinik Hoehenblick, Therapiezentrum Muenzesheim). The authors also acknowledge the research assistance of AnneKathrin Steger und Heike Ehrhardt.
REFERENCES
- Bertarkis, K.D. and Azari, R. (2011) Determinants and outcomes of patient-centered care. Patient Education and Counseling, 85, 46-52. doi:10.1016/j.pec.2010.08.001
- Bleses, H. (2005) Patient-centeredness as a quality feature. Medizinische Fakultät der Charité, Berlin. http://edoc.huberlin.de/dissertationen/bleses-helma-2005-01-24/HTML
- Cott, C.A., Teare, G., McGilton, K.S. and Lineker, S. (2006) Reliability and construct validity of the clientcentred rehabilitation questionnaire. Disability and Rehabilitation, 28, 1387-1397. doi:10.1080/09638280600638398
- Green, S.M., Tuzzio, L. and Cherkin, D. (2012) A framework for making patient-centered care front and center. The Permanente Journal, 16, 49-53.
- Hudon, C., Fortin, M., Haggerty, J., Loignon, C., Lambert, M. and Poitras, M.-E. (2012) Patient-centered care in chronic disease management: A thematic analysis of the literature in family medicine. Patient Education and Counseling, 88, 170-176. doi:10.1016/j.pec.2012.01.009
- Leplege, A., Gzil, F., Cammelli, M., Lefeve, C., Pachoud, B. and Ville, I. (2007) Person-centredness: Conceptual and historical perspectives. Disability and Rehabilitation, 29, 1555-1565. doi:10.1080/09638280701618661
- Mead, N. and Bower, P. (2000) Patient-centredness: A conceptual framework and review of the empirical literature. Social Science and Medicine, 51, 1087-1110. doi:10.1016/S0277-9536(00)00098-8
- Körner, M. (2009) A model of shared decision-making in medical rehabilitation. Die Rehabilitation, 48, 160-165. doi:10.1055/s-0029-1220748
- Körner, M., Steger, A.-K. and Ehrhardt, H. (2013) Designing an interprofessional training program for shared decision-making. Journal of Interprofessional Care, 27, 146-154. doi:10.3109/13561820.2012.711786
- Bieber, C., Nicolai, J., Hartmann, M., Blumenstiel, K., Ringel, N., Schneider, A., Härter, M., Eich, W. and Loh, A. (2009) Training physicians in shared decision-making— Who can be reached and what is achieved? Patient Education and Counseling, 77, 48-54. doi:10.1016/j.pec.2009.03.019
- Di Blasi, Z., Harkness, E., Ernst, E., Georgiou, A. and Kleijnen, J. (2001) Influence of context effects on health outcomes: A systematic review. Lancet, 357, 757-762. doi:10.1016/S0140-6736(00)04169-6
- Faller, H. (2003) Shared decision-making: An approach to strengthening patient participation in rehabilitation. Die Rehabilitation, 42, 129-135. doi:10.1055/s-2003-40097
- Charles, C., Gafni, A. and Whelan, T. (1997) Shared decision-making in the medical encounter: What does it mean? (or it takes at least two to tango). Social Science and Medicine, 44, 681-692. doi:10.1016/S0277-9536(96)00221-3
- Charles, C., Gafni, A. and Whelan, T. (1999) Decisionmaking in physician-patient encounter: Revisting the shared treatment decision-making model. Social Science and Medicine, 49, 651-661. doi:10.1016/S0277-9536(99)00145-8
- Charles, C., Whelan, T. and Gafni, A. (1999) What do we mean by partnership in making decisions about treatment? British Medical Journal, 319, 780-782. doi:10.1136/bmj.319.7212.780
- Makoul, G. and Clayman, M.L. (2006) An integrative model of shared decision-making in medical encounters. Patient Education and Counseling, 60, 301-312. doi:10.1016/j.pec.2005.06.010
- Scheibler, F., Schwantes, U., Kampmann, M. and Pfaff, H. (2005) Shared decision-making. GGW—Das Wissenschaftsforum in Gesundheit und Gesellschaft, 1, 23-31.
- Farin, E. (2010) Patient-provider communication in chronic illness: Current state of research in selectet areas. Rehabilitation, 49, 277-291. doi:10.1055/s-0030-1263160
- Scheibler, F., Janssen, C. and Pfaff, H. (2003) Shared decision-making: An overview of international research literature. Sozialund Präventivmedizin, 48, 11-23. doi:10.1007/s000380300002
- Simon, D., Loh, A. and Härter, M. (2008) Development and evaluation of interventions to support shared decision-making—Framework and measuring instruments. Zeitschrift für Medizinische Psychologie, 17, 149-159.
- Stewart, M.A. (1995) Effective physician-patient communication and health outcomes: A review. Canadian Medical Association Journal, 152, 1423-1433.
- Mackey, K., Parchman, M.P., Leykum, L.K., Lanham, H.J., Noel, P.H. and Zeber, J.E. (2012) Impact of the chronic care model on medication adherence when patients perceive cost as a barrier. Primary Care Diabetes, 6, 137-142. doi:10.1016/j.pcd.2011.12.004
- Thompson, L. and McCabe, R. (2012) The effect of clinician-patient alliance and communication on treatment adherence in mental health care: A systematic review. BMC Psychiatry, 12, 87. doi:10.1186/1471-244X-12-87
- Zeber, J.E., Copeland, L.A., Good, C.B., Fine, M.J., Bauer, M.S. and Kilbourne, A.M. (2008) Therapeutic alliance perceptions and medication adherence in patients with bipolar disorder. Journal of Affective Disorders, 107, 53-62. doi:10.1016/j.jad.2007.07.026
- Coulter, A. and Magee, H. (2003) The European patient of the future—state of health. Open University Press, Maidenhead.
- Murray, E., Pollack, L., White, M. and Lo, B. (2007) Clinical decision-making: Patients’ preferences and experiences. Patient Education and Counseling, 65, 189-196. doi:10.1016/j.pec.2006.07.007
- King, J.C., Nelson, T.R., Heye, M.L., Turturro, T.C. and Titus, M.N.D. (1998) Prescriptions, referrals, order writing, and the rehabilitation team function. In: DeLisa, J.A. and Gans, B.M. Eds., Rehabilitation Medicine: Principles and Practice, Lippincott-Raven, Philadelphia, 269-285.
- Mickan, S. and Rodger, S. (2000) The organisational context for teamwork: Comparing health care and business literature. Australian Health Review, 23, 179-192. doi:10.1071/AH000179
- Norrefalk, J.R. (2003) How do we define multidisciplinary rehabilitation? Journal of Rehabilitation Medicine, 35, 100-102. doi:10.1080/16501970306118
- Wade, D.T. (2001) Research into rehabilitation. What is the priority? Clinical Rehabilitation, 15, 229-232. doi:10.1191/026921501677354949
- Wagner, E.H. (2000) The role of patient care teams in chronic disease management. British Medical Journal, 320, 569-572. doi:10.1136/bmj.320.7234.569
- Grumbach, K. and Bodenheimer, T. (2004) Can health care teams improve primary care practice? Journal of the American Medical Association, 291, 1246-1251. doi:10.1001/jama.291.10.1246
- Valentine, M.A., Nemhard, I.M. and Edmondson, A.C. (2011) Measuring teamwork in health care settings: A review of survey instruments. http://www.hbs.edu/research/pdf/11-116.pdf
- Davenport, D.L., Henderson, W.G., Mosca, C.L., Khuri, S.F. and Mentzer, R.M. (2007) Risk-adjusted morbidity in teaching hospitals correlates with reported levels of communication and collaboration on surgical teams but not with scale measures of teamwork climate, safety climate, or working conditions. Journal of the American College of Surgeons, 205, 778-784. doi:10.1016/j.jamcollsurg.2007.07.039
- Lemieux-Charles, L. and McGuire, W.L. (2006) What do we know about health care team effectiveness? A review of the literature. Medical Care Research and Review, 63, 263-300. doi:10.1177/1077558706287003
- Kriston, L., Scholl, I., Hölzel, L., Simon, D., Loh, A. and Härter, M. (2010) The 9-item Shared Decision-making Questionnaire (SDM-Q-9). Development and psychometric properties in a primary care sample. Patient Education and Counseling, 80, 94-99. doi:10.1016/j.pec.2009.09.034
- Scholl, I., Kriston, L., Dirmaier, J., Buchholz, A. and Härter, M. (2012) Development and psychometric properties of the Shared Decision-Making Questionnaire—Physician version (SDM-Q-Doc). Patient Education and Counseling, 88, 284-290. doi:10.1016/j.pec.2012.03.005
- Körner, M. and Wirtz, M. Development and psychometric properties of the team-scale for measuring interprofessional collaboration from a patient and health care professional perspective. BMC Health Services Research.
- Schmidt, J., Lamprecht, F. and Wittmann W.W. (1989) Satisfaction with inpatient management. Development of a questionnaire and initial validity studies. Psychotherapie Psychosomatik Medizinische Psychologie, 39, 248-255.
- GfQG (2012) Questionnaire on patient satisfaction. http://www.gfqg.de/assessment_zuf8.htm
- Attkisson, C.C. and Zwick, R. (1982) The client satisfaction questionnaire. Psychometric properties and correlations with service utilization and psychotherapy outcome. Evaluation and Program Planning, 5, 233-237. doi:10.1016/0149-7189(82)90074-X
- Schaefer, J. and Davis, C. (2004) Case Management and the chronic care model. A multidisciplinary role. Lippincott’s Case Management, 9, 96-103. doi:10.1097/00129234-200403000-00007
- Stock, R.D., Reece, D. and Cesario, L. (2004) Developing a comprehensive interdisciplinary senior healthcare practice. Journal of the American Geriatrics Society, 52, 2128- 2133. doi:10.1111/j.1532-5415.2004.52576.x
- Wagner, E. (1998) Chronic disease management: What will it take to improve care for chronic illness? Effective Clinical Practice, 1, 2-4.
- Légaré, F., Stacey, D., Pouliot, S., Gauvin, F.P., Desroches, S. and Kryworuchko, J. (2011) Interprofessionalism and shared decision-making in primary care: A stepwise approach towards a new model. Journal of Interprofessional Care, 25, 18-25. doi:10.3109/13561820.2010.490502
- Légaré, F., Stacey, D., Brière, N., Desroches, S., Dumont, S., Fraser, K., Murray, M.-A., Sales, A. and Aubé, D. (2011) A conceptual framework for interprofessional shared decision-making in home care: Protocol for a feasibility study. BMC Health Services Research, 11, 23. doi:10.1186/1472-6963-11-23
- Légaré, F., Stacey, D., Gagnon, S., Dunn, S., Pluye, P., Frosch, D., Kryworuchko, J., Elwyn, G., Gagnon, M.-P. and Graham, I.D. (2011) Validating a conceptual model for an inter-professional approach to shared decisionmaking: A mixed methods study. Journal of Evaluation in Clinical Practice, 17, 554-564. doi:10.1111/j.1365-2753.2010.01515.x
- Légaré, F., Stacey, D., Brière, N., Fraser, K., Desroches, S., Dumont, S., Sales, A., Puma, C. and Aubé, D. (2013) Healthcare provider’s intentions to engage in an interprofessional approach to shared decision-making in home care programs: A mixed methods study. Journal of Interprofessional Care, 27, 214-222.
- Quaschning, K., Körner, M. and Wirtz, M. (2013) Analyzing the effects of shared decision-making, empathy and team interaction on patient satisfaction and treatment acceptance in medical rehabilitation using a structural equation modeling approach. Patient Education and Counseling, 91, 167-175. doi:10.1016/j.pec.2012.12.007
- O’Leary, K.J., Sehgal, N.L., Terrell, G. and Williams, M.V. (2012) Interdisciplinary Teamwork in Hospitals: A review and practical recommendations for improvement. Journal of Hospital Medicine, 7, 48-54. doi:10.1002/jhm.970
- Sevin, C., Moore, G., Shepherd, J., Jacobs, T. and Hupke, C. (2009) Transforming care teams to provide the best possible patient-centered, collaborative care. Journal of Ambulatory Care Management, 32, 24-31.
- Sinclair, L.B., Lingard, L.A. and Mohabeer, R.N. (2009) What’s so great about rehabilitation teams? An ethnographic study of interprofessional collaboration in rehabilitation unit. Archives of Physical Medicine and Rehabilitation, 90, 1196-1201. doi:10.1016/j.apmr.2009.01.021
- Mann, S.L., Budworth, M.H. and Ismaila, A.S. (2012) Ratings of counterproductive performance: The effect of source and rater behavior. International Journal of Productivity and Performance Management, 61, 142-156. doi:10.1108/17410401211194653
- Körner, M., Ehrhardt, H. and Steger, A.-K. (2011) Development of an interprofessional train-the-trainer program to implement shared decision-making in medical rehabilitation centers. Die Rehabilitation, 50, 331-339. doi:10.1055/s-0031-1285891

