World Journal of AIDS
Vol. 2 No. 4 (2012) , Article ID: 25336 , 11 pages DOI:10.4236/wja.2012.24043
Disclosing HIV to Infected Children in South Africa in the Era of HAART: A Grounded Theory Study on the Process, Reasons and Outcomes of Disclosure
![]()
School of Public Health, Faculty of Health Sciences, University of Limpopo, Medunsa Campus, Pretoria, South Africa.
Email: sphiwe_madiba@embanet.com
Received September 11th, 2012; revised October 13th, 2012; accepted October 23rd, 2012
Keywords: HIV Infected Children; Revealing the Diagnosis; Disclosure Outcomes; South Africa; Reaction to Disclosure; Disclosure Guidelines; Disclosure Process
ABSTRACT
South Africa has seen an increasing population of children and adolescents accessing antiretroviral treatment (ART) in the past seven years. Many of these children are at the age when they should know their HIV diagnosis. We used grounded theory to explore the process, reasons and outcomes of HIV disclosure to children accessing ART from a paediatric HIV clinic in South Africa. Twenty seven caregivers of children aged 6 - 13 years who were receiving ART participated in four focus group interviews. Four main themes, disclosure occurring as a process, asking HIV related questions, the right age to tell, and the child’s reaction to the diagnosis emerged. Biological caregivers approached disclosure as a process; they planned and prepared for the disclosure event for a long time. Full disclosure occurred when the caregivers had dealt with their own personal fears over the child’s diagnosis, resulting in disclosure being delayed to older age and adolescence. Non-biological caregivers disclosed impulsively to children and employed partial disclosure. Caregivers disclosed because of the child’s refusal to continue taking medication or the child repeatedly questioned the reasons for taking medication. Caregivers also disclosed because it was the right time to disclose, and the right time was often when the child reaches adolescence. After learning about their HIV diagnosis children became more adherent to medication, they also ensured that their HIV infected biological caregivers were adherent too. Children kept their diagnosis secret from people outside their immediate families. The increased survival of children on ART in South Africa calls for concerted efforts from researchers and health care providers to develop disclosure guidelines to assist caregivers to disclose to children in a manner that promotes the wellbeing of the child.
1. Introduction
Sub-Saharan Africa remains the region most heavily affected by HIV, of the estimated 3.4 million children under 15 years old living with HIV in 2010, 90% of them are in sub-Saharan Africa. About 350,000 children were newly infected with HIV in 2010 [1]. The Joint United Nations Programme on HIV/AID estimates that up to 280,000 children under 15 years were living with HIV in South Africa in 2009, making it the country with the highest number of children living with HIV in the world [2]. With a massive roll out of antiretroviral treatment (ART), South Africa has seen an increasing population of children and adolescents accessing ART in the past seven years [3]. Many of the children who started ART in South Africa are at the age when they should know their HIV diagnosis. Recent data from a South African study conducted with caregivers of HIV infected children show an increase in the number of older children accessing ART. The mean age of the children in this study was 8.2 years with a range of 4 - 17 years [4]. There is evidence from studies conducted in developed countries that issues regarding adherence to ART medication and the HIV diagnosis disclosure take on additional importance as children with HIV reach adolescence [5,6]. According to Domek [7] issues around adherence to ART medication, self-esteem and behavioural problems cannot be adequately addressed without HIV disclosure to infected children and adolescents. Furthermore, as HIV infected children reach adolescence, having information about their own disease becomes an essential part of HIV prevention within the larger population [6,8].
There is a great deal of evidence in support of the disclosure of the diagnosis to children infected with HIV. Blasini et al. [9] established that both the youth and their caregivers considered disclosure as a positive event for them and their families. Findings from developed countries show that children and adolescents who know their HIV diagnosis are more likely to accept HIV related medical care than those who are unaware of their diagnosis [8,10-12]. Disclosure positively influences adherence to ART for some HIV-positive children [13]. However, when children take their doses of ART medication they become asymptomatic, and they do not understand the visits to health care facilities for routine check-ups and the continuous taking of medication [10,14-16]. This often results in poor adherence to long term ART medication particularly among older children and adolescents [17-21]. Disclosure increases knowledge and understanding of HIV, helps to facilitate children’s adjustment to the illness and treatment regimens, boosts self-esteem, decreases risky behaviours, and builds stronger family ties to tackle more challenging issues in the future [10-12, 22]. In addition, Mellins et al. [23] observed less depression among children who knew their HIV diagnosis than in those who did not. Again, several studies maintain that HIV disclosure to children and adolescents has implications for the progression of the disease and the success of the treatment [11,14,20,24].
Current data from studies conducted in Sub Saharan Africa show that HIV disclosure rates to infected children remain low [25]. Moreover, data show that HIV disclosure to infected children is still delayed until older childhood and adolescence in many settings [9,16,23]. What complicates HIV disclosure to children in developing countries is the increasing prolonged survival among untreated vertically-infected HIV-positive children [26-28], who are now accessing HIV care services. In a study conducted in South Africa, a third (30.5%) of HIV infected children were diagnosed between 11 - 17 years [4]. Whereas in the beginning caregivers argued that the child was too young to know about their HIV diagnosis and delayed disclosure [7,20,29-31], children now live much longer without ART, and an increasing number is diagnosed in their early teens [4,26,28]. Delaying HIV disclosure to these children is likely to result in accidental disclosure with negative consequences. Accidental disclosure could lead to misinformation, confusion, bitterness and limited opportunities for processing the information in a supportive environment. Also, the possibility of children learning about their HIV diagnosis from sources other than their caregivers increases considerably with age because children are exposed to HIV and AIDS related information in their communities, schools, and through the media [23].
HIV disclosure to infected children is more complex than disclosure by adults because children have little control over when and how they are informed of their diagnosis. Caregivers usually hold the power to decide what is in the best interests of the child and may be reluctant to disclose for various reasons [30,32]. Consequently, most studies conducted on HIV disclosure to infected children report on the challenges experienced by caregivers to disclose HIV to their children. Previous studies maintained that caregivers in developing countries, often struggle with issues of how to talk to the child, what should be said and who should talk to the child [7, 33-35]. There are limited studies that examine the caregivers’ decision making process for HIV disclosure to infected children in developing countries. For South Africa, the country with the largest paediatric ART programme in the world [36]; it is imperative that health care providers and researchers understand why, when and how caregivers disclose HIV to their infected children to develop interventions to support caregivers in disclosure. This paper reports on the process, reasons and outcomes of HIV disclosure to children accessing ART from a paediatric HIV clinic in South Africa. The purpose of the study is to inform the development of interventions to manage HIV disclosure to children and adolescents enrolled in ART programs.
2. Materials and Methods
Data described here were collected as part of doctoral grounded theory study conducted in partial fulfilment of the requirements for a doctoral degree from the School of Public Health, University of Limpopo Medunsa Campus, South Africa. Data were collected between November 2009 and March 2010.
2.1. Setting
Focus group (FG) interviews were conducted with caregivers of HIV infected children receiving ART in a paediatric clinic of an academic hospital. The clinic at the Dr George Mukhari academic hospital started with paediatric ART in 2004 and provides treatment and care to children from urban, peri-urban and informal settlements in a resource limited district of Gauteng province in South Africa. Caregivers were recruited as they waited for consultation and medication during the routine monthly visits for their children, and scheduled appointments were made with caregivers who met the inclusion criteria. The criteria for selection for FG interviews was being the caregiver of an HIV infected child aged 6 - 13 years and receiving ART. Caregiver’s biographic and demographic information such as their age, gender, level of education, employment status, relationship with child, and the age of the child were carefully considered to maximize variation. One other critical criterion was a caregiver’s report that the child knew his/her HIV diagnosis, which was used to assign caregivers to either the disclosed or the non-disclosed groups. For the purpose of this study, we defined a caregiver as the biological mother, biological father, grandmother, grandfather, foster parent, or other relative who performs primary caregiving functions for the child routinely or on a daily basis.
2.2. Data Collection
The FG interviews were conducted by the lead researcher who is experienced in facilitating focus groups. A trained research assistant assisted with recruitment and FG interviews. Two open ended FG guides, one for disclosed and one for non-disclosed caregivers was used for the FG interviews. The guides were developed in English and translated into Setswana, a local language spoken by most caregivers in the study site. The FG interviews were conducted in Setswana and were audio recorded with the participants’ permission. FG interviews lasted for about 60 to 90 minutes. Written informed consent was obtained from individual caregivers prior to the start of the FG interview. The caregivers received R50.00 (equivalent US $8) to cover their transport cost, and refreshments were provided at the end of the FG interviews. A total of nine FG interviews were conducted with disclosed and non-disclosed caregivers of children on ART. One FG interview was conducted with a mixed group of disclosed and non-disclosed caregivers, three with non-disclosed and disclosed caregivers, respectively. Each FG interview had an average of seven participants with a total of 52 caregivers. Two follow up FG interviews were conducted with 12 caregivers.
The socio-demographic information of the caregivers and children in their care was collected at the end of the FG interviews using a brief self-administered questionaire. The tool was also translated to Setswana, and caregivers who could not read or write were assisted to complete the tool by the research assistant.
The Medunsa Research Ethics Committee of the University of Limpopo granted ethical approval for the study, and permission to conduct the study was obtained from the hospital management of Dr. George Mukhari Academic hospital. Participation in the study was voluntary, and the researchers ensured confidentiality throughout data collection. Informed consent was obtained from participants prior to the FG interviews.
2.3. Data Analysis
The constant comparative data analysis as described by Straus and Corbin [37] guided the analysis of data for this study. FG interviews were transcribed verbatim in Setswana and translated to English by the lead researcher. Each transcribed FG interview was reviewed for accuracy by replaying each interview recorder whilst reading and translating the transcript. Transcripts were imported into NVivo version 8, a computer software package for qualitative analysis, which was used for coding all the FG interviews. Analysis began with the development of a code list from multiple readings of a number of transcripts. The code list was reviewed by the lead researcher and the research promoter for consensus on the definitions of the themes and sub themes. This was followed by open coding to identify major themes and categories that emerged from the data. The lead researcher and promoter met frequently to review themes, and new emergent themes identified, were integrated in the coding process. The transcripts were recoded if a new code emerged or an existing code was revised. Axial coding was used to draw tentative connections and relationships between the codes and categories that were generated through open coding [37]. The simultaneous processes of data collection and analysis permitted on going verification of codes and categories. Data triangulation, transcribing verbatim, peer debriefing, and analyzing data using computer software were employed to attain trustworthiness [38].
Because this paper is focused on the process, reasons and outcomes of disclosure, analyses are confined to FG interviews with non-disclosed caregivers.
Responses provided on the caregiver and child demographic data were analysed using Stata version 10.0 [39].
3. Findings
3.1. Sample Description
Demographic characteristics of the caregivers are presented in Table 1. A total of 27 caregivers of children on ART participated in three FG interviews and one follow up FG interview. Caregivers ranged in age from 20 - 70 years. Less than half 12 (44.4%) of the caregivers were the biological mothers of children. The caregiver employment status revealed that 19 (70.4%) were unemployed and that the majority 22 (81.5%) depended on child support grant. Half 14 (51.9%) of the caregivers were married while more than a third 10 (37%) were single. A third 8 (29.6%) had high school and tertiary education and 12 (44.4%) had a secondary education. About 12 (44.4%) of the caregivers did not know their HIV status while 3 (11.1%) were HIV negative.
Demographic information on children was collected from the caregivers and is presented in Table 2. The children ranged in age from 6 - 13 years, and the mean age was 11 years. More than half 14 (51.8%) were diagnosed between 10 - 13 years, and the mean age of diagnosis was 8.3 years. More than two thirds 16 (61.1%) of the children were disclosed to between 10 - 13 years, and
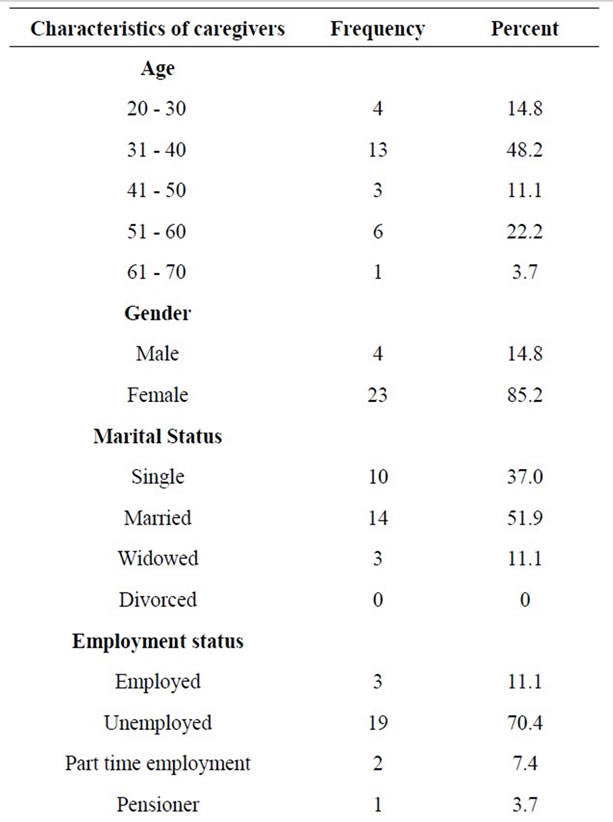
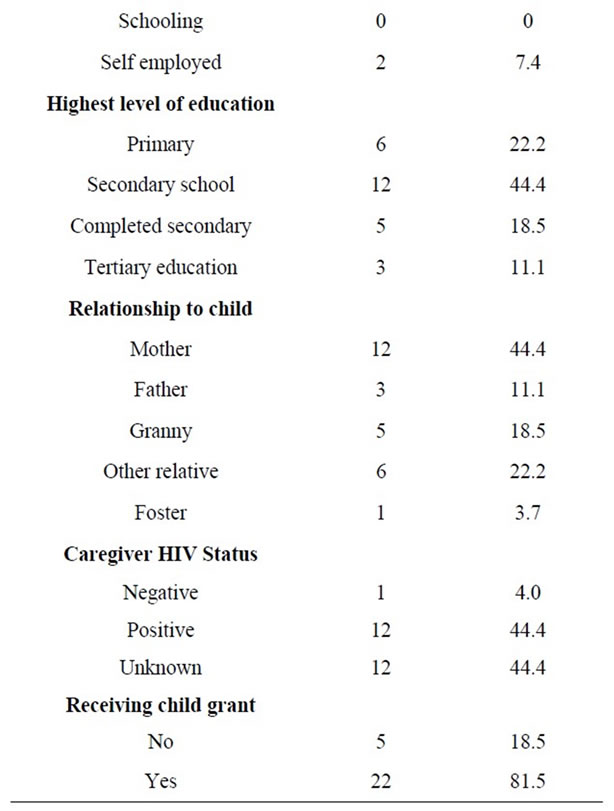
Table 1. Caregiver demographic information (n = 27).
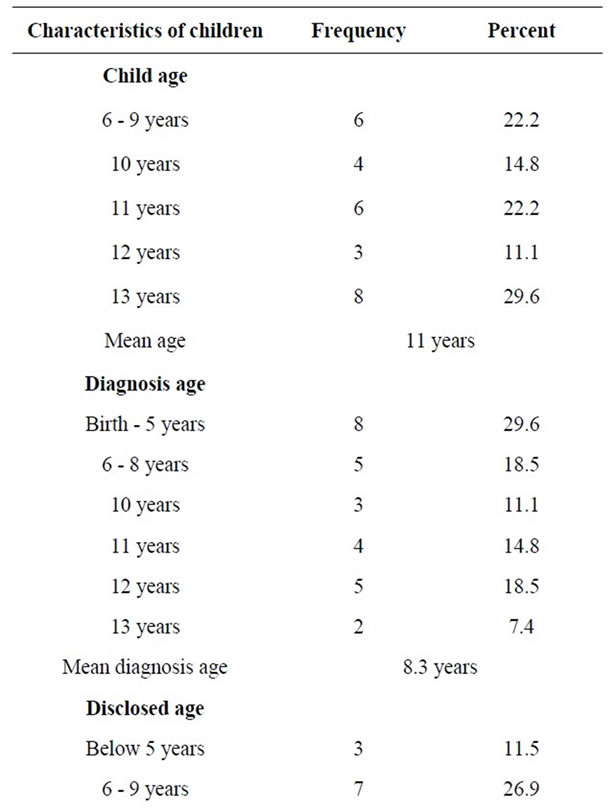
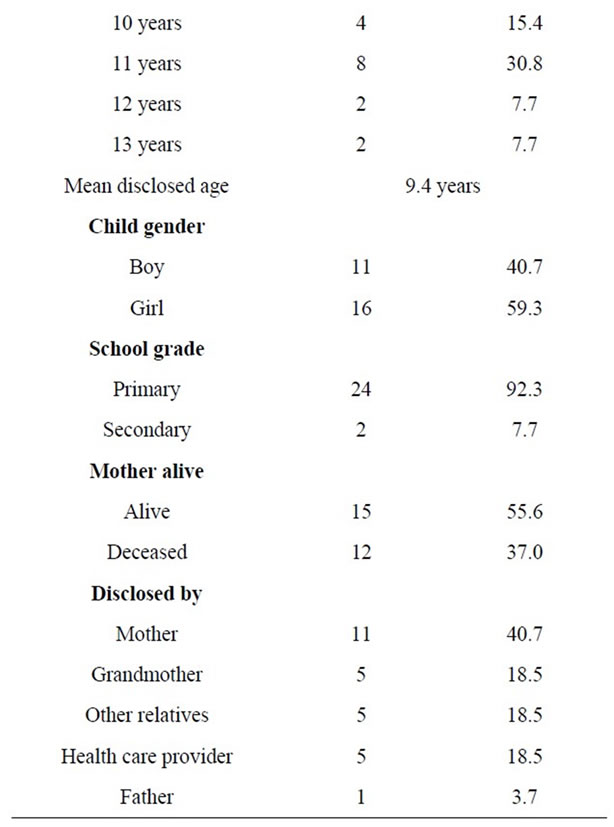
Table 2. Demographic information on children (n = 27).
the mean age of disclosure was 9.4 years. All of the children were on ART, and the mean duration on ART was 3.2 years. Twelve (37%) children were maternal orphans. Almost all (92.3%) of the children were in primary school.
3.1.1. Disclosure Occurring as a Process
Disclosure in this sample was approached as a process and not as once only occurrence. Caregivers talk about a process of providing children with information appropriate for their ages and ability to understand.
I think it is important that she gets used to the disease at an early age and that you keep reminding the child at an early age and not when she is 11 or 12 years. I do not think it can be a problem if she is told at 5 years so that she grows up knowing about her illness and you continue building her understanding, and you tell the child information that she can understand. By the time she is 12 years she will understand because you would have given her a foundation (biological mother of a 12 years old).
If you tell him when he is much older he will be hurt, but if you tell him at an early age he grows up knowing about this thing (HIV) and he will understand it (aunt of a 13 years old).
The data show that the decision to disclose the HIV diagnosis to children was difficult, stressful and emotional for most of the caregivers prior to disclosure.
Eish! …, I was afraid…, I did not know how she was going to react…, I know the pain of knowing. I was hurt when I found that she is sick (biological mother of a 6 years old).
For caregivers who were not the biological mothers of the children, disclosure was easy, and they often disclosed immediately after the child came into their care or after diagnosis.
The reason I decided to tell him…, his mother died, and a few months later he got sick and was admitted in hospital. When we got home from the hospital, I sat him down and told him (grandmother of an 11 years old).
Besides the fact that caregivers experienced disclosure as emotional, they also reported that there was a time before disclosure when they did not know what to tell and how to tell their children about the HIV diagnosis.
Eish! …, In the beginning, it is very difficult to tell the child, it is difficult when the child is still small, you do not know where to begin. But one day I decided to tell him (grandmother of a 10 years old).
Planning and preparing for the disclosure event took different forms, and was depended on the emotional status and readiness of the caregiver to disclose.
It was scary…, whenever I wanted to tell him, I would take him to the McDonald’s because I was not sure how he was going to react, whether he will be angry at me. So I always postponed telling him, and I did it often. If the clinic prepare us, it will be helpful because it is difficult (biological mother of an 11 years old).
Although caregivers believed that disclosure should be planned, in reality, some of the disclosure events were accidental, unplanned and impulsive.
I was in the kitchen about to take my medication when she said mama drink your medication otherwise you are going to die. I said do you think I will die? And she said, “don’t you see that you are sick?” I said what is wrong with me? She said you have HIV, on TV they say people are dying from HIV. I was confused for a few minutes and I said it is better that I tell her and I said that is true, mama is HIV positive and so are you. She said “I am not sick” and you could see that she said that with all her heart, but I already said it and I could not take it back (biological mother of a 6 years old).
3.1.2. Asking HIV Related Questions
Caregivers reported that the disclosure event was influenced by their children’s asking questions about why they had to continuously take medication.
The child was asking why she was taking medication all the time and why other children were not taking medication. She was complaining that she is always being called to take medication while other children are playing. I had to explain that the treatment is for her life (grandmother of an 8 years old).
Some of the caregivers disclosed the HIV diagnosis to the child because of the child’s refusal to continue taking medication:
The reason I told him is because he did not want to take the medication, he takes his medication at six in the morning and evenings, and sometimes he comes around six thirty from playing. So, I decided that it is better that I tell him because it looks like he does not know (aunt of a 13 years old).
The reason I decided to tell her is because she would cry when I call her for treatment and say she is tired of taking medication (biological mother of a 13 years old).
Close to half (12 out of 27) of the children in this sample were maternal orphans and were cared for by relatives and foster parents. One of the reason caregivers disclose was in response to children’s questions about their biological parents.
He asked, and we told him that his mother and father died from AIDS, the other thing he also wanted to know the reason for taking medication (aunt of a 12 years old).
She was asking me about her mother and I explained that this is the reason you also have this disease (HIV), the disease that you suffer from is the same disease that killed your mother (aunt of a 12 years old).
3.1.3. Right Age to Tell
Caregivers perceived the age when the child is told about the diagnosis as important for the child to be able to manage the disclosure. Some of the caregivers disclosed because they believed that it was the right age for the child to know.
I think we helped him to know so that he grows up knowing his condition. I am also grateful that if I die XXX will not suffer because he will know his condition (grandmother of a 10 years old).
When the child knows about his illness he can deal with that better and does not think about it all the time (biological father of a 14 years old).
Fear that the child will infect other children was a great concern for caregivers in this study sample. Protecting other children from being infected was the reason why children should know their HIV diagnosis.
The reason I told her is because I wanted her to know what is wrong with her so that if she is playing with other children and something happens to her, and there is blood she should not allow people to touch her (aunt of a 12 years old).
3.1.4. The Child’s Reaction to the Diagnosis
Prior to disclosure most caregivers were fearful of the children’s reaction to the disclosure. Responding to the question of how their children reacted to learning about their HIV diagnosis, some caregivers reported that children were mostly saddened by the disclosure.
He went to the disclosure camp, and when he came back he was angry with me and was unhappy and moody, when I tried to find out what was wrong I realized that I was hurting him more. When he got back from the camp he did not want to come close to me, and he was crying all the time and did not want to discuss that topic (biological mother of a 9 years old).
She was not angry but was sad…, after being told, she isolated herself from us, and when I asked her what she was thinking of she said I am not thinking about anything mama. But I could see that what I told her was making her sad (biological mother of a 13 years old).
In contrast, some caregivers experienced the disclosure occurrence differently and reported that their children were able to easily accept the disclosure.
She wanted to know if the medication she was taking was for HIV, and I said yes, she said “if I do not drink the medication, will I die”, I said yes you will die. She wanted to know how long will she be taking this medication, and I told her that she will take medication for the rest of her life. She reacted well to this, and she was not upset or hurt (foster mother of a 10 years old).
One of the challenges for the caregivers before disclosure was fear that the child was going to ask about the source of the infection. Data show that indeed children asked about the source of the disease after learning about their HIV diagnosis.
My child asked why she is positive and she wanted to know if I was also positive, I told her that I am positive but not yet taking medication (biological mother of a 12 years old).
He asked why he was taking medication and what the medication was for; he also asked me how he got the disease (grandmother of a 10 years old).
Most of the disclosure in this sample was prompted by issues around medication. Reports from caregivers show that following disclosure children became adherent to the medication.
Now when it is time for treatment, she comes running even if she was playing outside. Now she is able to take her medication on her own (foster mother of a 10 years old).
Since then…, around six in the evenings she comes, even if she has been playing she will go to the bedroom and take her medication. She does not have problems anymore (biological mother of a 11 years old).
Reports from caregivers also show that adhering to their medication for most children in the sample also meant ensuring that their biological HIV infected caregivers were adherent to their medication too.
She knows and reminds me of the times for my treatment. She is happy these days. She has no problems; she knows her times for her medication (biological mother of an 11 years old).
Even if I am not there he knows that we both take medication. Sometimes I leave the house early in the morning, when I get back he would ask if I have taken my medication (biological mother of a 9 years old).
Often caregivers instructed children to keep their HIV diagnosis secret for fear of negative consequences should the child tell others about their disease. However, even in the absence of instructions the children still kept their HIV diagnosis secret.
We did not tell him to talk or not to talk, but the way I see it, he does not talk, I would not like him to talk (brother of an 8 years old).
We did not say anything she just kept quiet, and she is quiet about that (aunt of a 14 years old).
4. Discussion
The decision to disclose the diagnosis to HIV infected children was difficult for most caregivers in this study. Similar to other studies, caregivers found disclosure to be an emotionally traumatic event [40,41]. Caregivers delayed disclosure because they were fearful that their children would ask about the source of the infection, which they perceived as a difficult question to answer. Consequently, only 12 of the 27 children were told about their diagnosis by biological mothers, the rest were disclosed to by nonbiological caregivers. This study and others, argue that nonbiological caregivers do not have to deal with most of the fears that biological parents have first to deal with, like passing the infection on to the children. For biological caregivers disclosing the HIV diagnosis to children is comparable to disclosure of the parent’s HIV status [16,22,23,41]. When nonbiological caregivers disclose there is less blame and guilt than when biological caregivers disclose [41]. As a result, nonbiological caregivers often disclosed shortly after the child came into their care or after the HIV diagnosis.
Literature on HIV disclosure to children conceptualises disclosure as a once-off event or a process when information about the diagnosis is provided to the child [16]. Ledlie [22] discusses three main patterns of disclosure and maintains that disclosure to children is a process that caregivers pass through with a continuum of conditions from total secrecy to partial disclosure to full disclosure. The same patterns of disclosure were observed in this study, most biological caregivers employed full disclosure in telling their children about the diagnosis, while nonbiological caregivers were inclined to use partial disclosure. Partial disclosure refers to the strategy whereby caregivers provide children with information about their illness without naming the disease as HIV/ AIDS [12]. Caregivers in this study often told children that they have a disease similar to what their mothers had. Given that only 12 of the 27 children were told their HIV diagnosis by their biological mothers, the data suggest that most children in the study received partially disclosure.
Similar to other studies, some of the caregivers in this study approached disclosure as a process; planning and preparing for the disclosure event [16,23,32,33,41,42]. Prior to disclosure, caregivers planned the disclosure event over a long period. Planning involved specific activities including buying toys, cell phones, or taking the child out for lunch to prepare for the disclosure event. Similar planning activities were reported [16]. In addition, caregivers exposed the children to HIV related programs on TV to provide them with HIV-related information in preparation for disclosure. While other caregivers read HIV and AIDS booklets with their children. The reading sessions were used to provide children with explanations about HIV. These activities influenced caregivers and their children positively, and made disclosure easy.
However, data from this study and others show that not every disclosure event was well planned and prepared for [16,42]. Some of the caregivers disclosed during moments of frustration in response to the child’s refusal to take ART medication. Caregivers also disclosed impulsively because the child persistently asked questions about the nature of their illness. Similar findings were reported in other studies [16,42,43]. Disclosure was also a once off impulsive event when nonbiological caregivers disclosed soon after the child was diagnosed with HIV or came under their care. The impulsive nature of HIV disclosure to children could be attributed to caregiver lack of disclosure skills as well as the lack of disclosure guidelines reported in many studies [7,20,44, 45].
The child’s reluctance to adhere to ART medication prompted disclosure in some cases. Some caregivers disclosed because of the child’s refusal to continue taking ART medication. While others disclosed because the child was persistent in asking questions about taking medication continuously. These findings should be viewed in the context where most of the children were healthy and asymptomatic during field work, and they could not understand why they had to take ART medication. The data generally agree with findings from previous studies [14- 16,23,30,46,47]. In line with previous findings, children became adherent to their ART medication on learning about their diagnosis [48]. Adhering to medication for most children also meant ensuring that their biological caregivers were adherent to their medication too. A variety of aids like watches with timers, reminder notices and mobile phone alarms were used to remind them to take their medication. Similar findings were reported in previous studies [46,49].
One other reason for disclosure was the persistent questioning from symptomatic children about the nature of their disease. Other studies also reported similar findings [46,50]. Persistent illness-related questioning was not one of the main reasons why caregivers disclosed to children. Most children were on ART medication for three years and were asymptomatic and healthy. Caregivers also disclosed because children were asking questions about the death of their biological parents; 12 of the 27 children were maternal orphans. According to Vaz et al. [16] caregivers view disease-related questions as a motivation to tell children of their HIV diagnosis. Contrary to that, in this study, disclosure prompted by persistent illness related questioning was often unplanned, impulsive and partial.
The right age to tell, also determined disclosure of HIV to children, the right age is contextualized as the time when the child is perceived to have the ability to understand the diagnosis. Caregivers disclosed because they believed that once children learn about their HIV diagnosis they will be able to manage the disease better. In line with this view, Bhattacharya [51] reported better self-care as the most frequently cited advantage of disclosure among children who were told about their HIV diagnosis. The right time to disclose for many caregivers was the time when the child reaches adolescence. Similar findings were reported previously [8,16,30,40]. Furthermore, caregivers in this study and others, disclosed to the adolescent primarily to protect their children, and also to protect others from becoming infected [12,16,30].
The children’s initial reaction to disclosure was crying, shock, disbelief, and anger. Children were saddened by the disclosure; they isolated themselves, were often moody, tearful and withdrawn. Some caregivers reported that their children reacted well to the disclosure and were able to accept the diagnosis. Mellins et al. [23] argue that, caregivers tended to underestimate the level of shock to children and overestimate the percentage of neutral reactions of children at the time of the disclosure. This study argues that given the process of disclosure employed by most caregivers, it is likely that the same phenomenon could have happened to caregivers’ estimation of the reactions of their children. For some caregivers, disclosure was a once-off impulsive occurrence and not a process that required multiple conversations as suggested by Mellins [23].
Recent findings from Vaz et al. [16] show that upon learning about their diagnosis, most children did not ask questions or verbalize their concerns to anyone. Although children in this study asked questions following disclosure, caregivers did not associate the questioning to concerns that the children have about their diagnosis. Children asked questions about how long they were expected to take their ART medication, whether their biological caregiver was also infected with HIV, whether their siblings were infected, they wanted to know if they were going to die, as well as the source of their infection. Similar findings were reported [16].
In response to learning about their diagnosis, children developed strategies to manage their reception of the HIV disclosure. Secrecy was used as a strategy to manage HIV disclosure by the children. Caregivers reported that after disclosure, some of the children were instructed to keep the diagnosis secret, due to the stigma associated with HIV and AIDS. However, even when children were not instructed to keep the diagnosis secret, they still kept the diagnosis secret. This phenomenon was also identified by Hejoaka [52] who argues that children keep the diagnosis secret because of their awareness of the secret nature of the disease. In an endeavor to keep the diagnosis secret, children in this study developed strategies to conceal their ART medications and the disease. They used diverse strategies in the presence of other persons to notify the caregiver discreetly that it is time for their medication. These findings are similar to other studies [32,52].
5. Conclusions
We found that HIV disclosure to children was influenced by the caregiver and child related factors as well as the social context of HIV infection and disclosure. The interplay of these factors resulted in HIV disclosure being delayed sometimes to older age and adolescence. Biological mothers, as compared to nonbiological caregivers experienced disclosure as traumatic, and feared that they would be blamed for the HIV infection. Consequently, biological mothers often approached disclosure as a process and planned and prepared for the disclosure event. Full disclosure often occurred when the biological caregivers believed that they had dealt with their own personal fears over the child’s diagnosis. However, planning and preparing for the disclosure often resulted in disclosure being delayed to late adolescence. When disclosure is delayed till late adolescence, adherence to ART medication becomes a problem; hence most caregivers disclosed because the child was not adherent to medication or repeatedly questioned the reasons for taking medication. Taking into consideration that an increasing number of children are diagnosed in their early teens, early disclosure of HIV to these children should take priority to ensure adherence to ART medication. The role of the health care providers in facilitating HIV disclosure to children becomes crucial.
In contrast, nonbiological caregivers often disclosed impulsively to children soon after the child was diagnosed with HIV or came under their care. These findings have implications for HIV disclosure to infected children. When disclosure was a once of event and partial, HIV infected children lose the opportunity to ask questions and to be taught about their disease and ART medication. Caregivers often delay disclosure because they lack disclosure skills; an impulsive disclosure is also an indication of the lack of disclosure skills as well as the lack of the comprehension of the impact of a HIV diagnosis disclosure to a child. When disclosure is once off, caregivers also downplay the reactions of the child to the HIV disclosure, hence the report that most children reacted well to the disclosure. The development of disclosure guidelines to assist caregivers to disclose HIV to infected children has been the subject of debates for a more than a decade. The increased survival of children on ART in developing countries like South Africa calls for a concerted effort from researchers and health care providers to develop disclosure guidelines to assist caregivers to disclose to children in a manner that would promote the wellbeing of the child.
The outcome of disclosure was positive for most children, after learning about their HIV diagnosis, children became adherent to ART medication they also ensured that their HIV infected biological caregivers were adherent too. In spite of this, children kept their diagnosis secret; they used secrecy as a strategy to conceal their ART medication as well as the disease from people outside their immediate families. Keeping a secret is an additional burden for children who have to cope with their HIV diagnosis, adhere to ART medication, and monitor their caregivers’ adherence to their ART medication. Disclosure guidelines should take into consideration the secret nature of HIV and educate caregivers about the negative impact of secrets on the child.
6. Acknowledgements
This research was partially funded by AAU Grants for Graduate Research and Scholarship. We thank Mr. Abram Maubane the research assistant as well as Ms Chidi Matlala an MPH intern for their role in data collection. We also thank health care providers from the paediatric clinics of Doctor George Mukhari hospital for their guidance and assistance during data collection.
REFERENCES
- WHO, UNAIDS, and UNICEF, “Global HIV/AIDS Response: Epidemic Update and Health Sector Progress Towards Universal Access, Progress Report,” WHO, Geneva, 2011. http://www.who.int/hiv/pub/progress_report2011/en/index.html
- UNAIDS, “Report on the Global AIDS Epidemic,” UNAIDS, Geneva, 2009. http://data.unaids.org/pub/report/2009/jc1700_epi_update_2009_en.pdf
- O. Shisana, T. Rehle, L. C. Simbayi, K. Zuma, J. Jooste, et al., “South African National HIV Prevalence, Incidence, Behaviour and Communication Survey 2008: A Turning Tide among Teenagers?” HSRC Press, Cape Town, 2009. http://www.hsrc.ac.za/Document-3239.phtml
- J. M. Mahloko and S. Madiba, “Disclosing HIV Diagnosis to Children in Odi District, South Africa: Reasons for Disclosure and Non-Disclosure,” African Journal of Primary Health Care and Family Medicine, Vol. 4, No.1, 2012. http://www.phcfm.org/index.php/phcfm/article/view/345
- R. G. Steele, T. D. Nelson and B. P. Cole, “Psychosocial Functioning of Children with AIDS and HIV Infection: Review of the Literature from a Socio-Ecological Framework,” Journal of Developmental & Behavioral Pediatrics, Vol. 28, No. 1, 2007, pp. 58-69. doi:10.1097/DBP.0b013e31803084c6
- C. Thorne, M. L. Newell, F. A. Botet, A. B. Bohlin, A. Ferrazin, et al., “Older Children and Adolescents Surviving with Vertically Acquired HIV Infection,” Journal of Acquired Immune Deficiency Syndromes, Vol. 29, No. 4, 2002, pp. 396-401.
- G. J. Domek, “Debunking Common Barriers to Pediatric HIV Disclosure,” Journal of Tropical Pediatrics, Vol. 56, No. 6, 2010, pp. 440-442. doi:10.1093/tropej/fmq013
- P. Lester, M. Chesney, M. Cooke, R. Weiss, P. Whalley, et al., “When the Time Comes to Talk about HIV: Factors Associated with Diagnostic Disclosure and Emotional Distress in HIV-Infected Children,” Journal of Acquired Immune Deficiency Syndromes, Vol. 31, No. 3, 2002, pp. 309-317. doi:10.1097/00126334-200211010-00006
- I. Blasini, C. Chantry, C. Cruz, L. Ortiz, I. Salabarría, et al., “Disclosure Model for Pediatric Patients Living with HIV in Puerto Rico: Design, Implementation, and Evaluation,” Journal of Developmental & Behavioral Pediatrics, Vol. 25, No. 3, 2004, pp. 181-189. doi:10.1097/00004703-200406000-00007
- C. E. Abadía-Barrero and M. D. LaRusso, “The Disclosure Model versus a Developmental Illness Experience Model for Children and Adolescents Living with HIV/ AIDS in São Paulo, Brazil,” AIDS Patient Care and STDs, Vol. 20, No. 1, 2006, pp. 36-43.
- P. J. Bachanas, K. A. Kullgren, K. S. Schwartz, B. Lanier, J. S. McDaniel, et al., “Predictors of Psychological Adjustment in School-Age Children Infected with HIV,” Journal of Pediatric Psychology, Vol. 26, No. 6, 2001, pp. 343-352. doi:10.1093/jpepsy/26.6.343
- I. Funck-Brentano, D. Costagliola, N. Seibel, E. Straub, M. Tardieu, et al., “Patterns of Disclosure and Perceptions of the Human Immunodeficiency Virus in Infected Elementary School-Age Children,” Archives of Pediatric Adolescence Medicine, Vol. 151, No. 10, 1997, pp. 978- 985. doi:10.1001/archpedi.1997.02170470012002
- S. Biadgilign, A. Deribew, A. Amberbir and K. Deribe, “Barriers and Facilitators to Antiretroviral Medication Adherence among HIV-Infected Paediatric Patients in Ethiopia: A Qualitative Study,” SAHARA J, Vol. 6, No. 4, 2009, pp. 148-154.
- S. Kallem, L. Renner, M. Ghebremichael and E. Paintsil, “Prevalence and Pattern of Disclosure of HIV Status in HIV-Infected Children in Ghana,” AIDS and Behavior, Vol. 15, No. 6, 2010, pp. 1121-1127.
- C. Merzel, N. Van Devanter and M. Irvine, “Adherence to Antiretroviral Therapy among Older Children and Adolescents with HIV: A Qualitative Study of Psychosocial Contexts,” AIDS Patient Care and STDs, Vol. 22, No. 12, 2008, pp. 977-987. doi:10.1089/apc.2008.0048
- L. M. E. Vaz, E. Eng, S. Maman, T. Tshikandu and F. Behets, “Telling Children They Have HIV: Lessons Learned from Findings of a Qualitative Study in SubSaharan Africa,” AIDS Patient Care and STDs, Vol. 24, No. 4, 2010, pp. 247-256. doi:10.1089/apc.2009.0217
- S. L. Marhefka, L. J. Koenig, S. Allison, P. Bachanas, M. Bulterys, et al., “Family Experiences with Pediatric Antiretroviral Therapy: Responsibilities, Barriers, and Strategies for Remembering Medications,” AIDS Patient Care and STDs, Vol. 22, No. 8, 2008, pp. 637-647. doi:10.1089/apc.2007.0110
- C. A. Mellins, E. Brackis-Cott, C. Dolezal and E. J. Abrams, “The Role of Psychosocial and Family Factors in Adherence to Antiretroviral Treatment in Human Immunodeficiency Virus-Infected Children,” The Pediatric Infectious Disease Journal, Vol. 23, No. 11, 2004, pp. 1035-1041. doi:10.1097/01.inf.0000143646.15240.ac
- D. A. Murphy, C. M. Wilson, S. J. Durako, L. R. Muenz and M. Belzer, “Antiretroviral Medication Adherence among the REACH HIV-Infected Adolescent Cohort in the USA,” AIDS Care: Psychological and Socio-Medical Aspects of AIDS/HIV, Vol. 13, No. 1, 2001, pp. 27-40.
- P. Oberdorfer, T. Puthanakit, O. Louthrenoo, C. Charnsil, V. Sirisanthana, et al., “Disclosure of HIVAIDS Diagnosis to HIV-Infected Children in Thailand,” Journal of Paediatrics and Child Health, Vol. 42, No. 5, 2006, pp. 283-288. doi:10.1111/j.1440-1754.2006.00855.x
- P. L. Williams, D. Storm, G. Montepiedra, S. Nichols, B. Kammerer, et al., “Predictors of Adherence to Antiretroviral Medications in Children and Adolescents with HIV Infection,” Pediatrics, Vol. 118, No. 6, 2006, pp. e1745- e1757.
- S. W. Ledlie, “Diagnosis Disclosure by Family Caregivers to Children Who Have Perinatally Acquired HIV Disease: When the Time Comes,” Nursing Research, Vol. 48, No. 3, 1999, pp. 141-149. doi:10.1097/00006199-199905000-00004
- C. A. Mellins, E. Brackis-Cott, C. Dolezal, A. Richards, S. W. Nicholas, et al., “Patterns of HIV Status Disclosure to Perinatally HIV-Infected Children and Subsequent Mental Health Outcomes,” Clinical Child Psychology and Psychiatry, Vol. 7, No. 1, 2002, pp. 101-114. doi:10.1177/1359104502007001008
- M. Ferris, K. Burau, A. M. Schweitzer, S. Mihale, N. Murray, et al., “The Influence of Disclosure of HIV Diagnosis on Time to Disease Progression in a Cohort of Romanian Children and Teens,” AIDS Care: Psychological and Socio-Medical Aspects of AIDS/HIV, Vol. 19, No. 9, 2007, pp. 1088-1094.
- S. Biadgilign, A. Deribew and A. E. H. K. D. Amberbir, “Factors Associated with HIV/AIDS Diagnostic Disclosure to HIV Infected Children Receiving HAART: A Multi-Center Study in Addis Ababa, Ethiopia,” PLoS One, Vol. 6, No. 3, 2011, Article ID: e17572. doi:10.1371/journal.pone.0017572
- R. A. Ferrand, E. L. Corbett, R. Wood, J. Hargrove, C. E. Ndhlovu, et al., “AIDS among Older Children and Adolescents in Southern Africa: Projecting the Time Course and Magnitude of the Epidemic,” AIDS, Vol. 23, No. 15, 2009, pp. 2039-2046.
- O. Shisana, S. Mehtar, T. Mosala, M. Zungu-Dirwayi, T. Rehle, et al., “HIV Risk Exposure in Children: A Study of 2 - 9-Year-Olds Served by Public Health Facilities in the Free State, South Africa,” HSRC Press, Cape Town, 2005.
- S. A. Walker, V. Mulenga, F. Sinyinza, K. Lishimpi, A. Nunn, et al., “Determinants of Survival without Antiretroviral Therapy after Infancy in HIV-1-Infected Zambian Children in the CHAP Trial,” JAIDS Journal of Acquired Immune Deficiency Syndromes, Vol. 42, No. 5, 2006, pp. 637-645. doi:10.1097/01.qai.0000226334.34717.dc
- F. G. Kouyoumdjian, T. Meyers and S. Mtshizana, “Barriers to Disclosure to Children with HIV,” Journal of Tropical Pediatrics, Vol. 51, No. 5, 2005, pp. 285-287. doi:10.1093/tropej/fmi014
- A. Lesch, L. Swartz, A. Kagee, K. Moodley, Z. Kafaar, et al., “Paediatric HIV/AIDS Disclosure: Towards a Developmental and Process-Oriented Approach,” AIDS Care: Psychological and Socio-Medical Aspects of AIDS/HIV, Vol. 19, No. 6, 2007, pp. 811-816.
- S. Waugh, “Parental Views on Disclosure of Diagnosis to Their HIV-Positive Children,” AIDS Care: Psychological and Socio-Medical Aspects of AIDS/HIV, Vol. 15, No. 2, 2003, pp. 169-176.
- L. P. Wiener, C. A. P. Mellins, S. P. Marhefka and H. B. P. Battles, “Disclosure of an HIV Diagnosis to Children: History, Current Research, and Future Directions,” Journal of Developmental & Behavioral Pediatrics, Vol. 28, No. 2, 2007, pp. 155-166.
- D. Dematteo, C. Harrison, C. Arneson, R. S. Goldie, A. Lefebvre, et al., “Disclosing HIV/AIDS to Children: The Paths Families Take to Truth Telling,” Psychology, Health & Medicine, Vol. 7, No. 3, 2002, pp. 339-356. doi:10.1080/13548500220139395
- T. P. Nelms and V. L. Zeigler, “A Study to Develop a Disclosure to Children Intervention for HIV-Infected Women,” Journal of the Association of Nurses in AIDS Care, Vol. 19, No. 6, 2008, pp. 461-469. doi:10.1016/j.jana.2008.05.005
- G. A. Heeren, “Changing Methods of Disclosure. Literature Review of Disclosure to Children with Terminal Illnesses, including HIV,” The European Journal of Social Science Research, Vol. 24, No. 1-2, 2011, pp. 199-208. doi:10.1080/13511610.2011.553506
- UNGASS, “South Africa UNGASS Country Progress Report,” 2010. http://data.unaids.org/pub/report/2010/southafrica_2010_country_progress_report_en.pdf
- A. Strauss and J. Corbin, “Basics of Qualitative Research. Techniques and Procedures for Developing Grounded Theory,” 2nd Edition, Sage, Newbury Park, 1998.
- J. W. Creswell, “Qualitative Inquiry and Research Method: Choosing among Five Approaches,” 2nd Edition, Sage, Thousand Oaks, 2007.
- StataCorp, “Stata Statistical Software. Release 10,” StataCorp LP, 2007.
- S. Instone, “Perceptions of Children with HIV Infection When Not Told for So Long: Implications for Diagnosis Disclosure,” Journal of Pediatric Health Care: Official Publication of National Association of Pediatric Nurse Associates & Practitioners, Vol. 14, No. 5, 2000, pp. 235-243.
- L. Chi-Ling and R. Johann-Liang, “Disclosure of the Diagnosis of HIV/AIDS to Children Born of HIV-Infected Mothers,” AIDS Patient Care and STDs, Vol. 13, No. 1, 1999, pp. 41-45. doi:10.1089/apc.1999.13.41
- P. Lester, M. Chesney, M. Cooke, P. Whalley, B. Perez, et al., “Diagnostic Disclosure to HIV-Infected Children: How Parents Decide When and What to Tell,” Clinical Child Psychology and Psychiatry, Vol. 7, No. 1, 2002, pp. 85-99. doi:10.1177/1359104502007001007
- D. Kennedy, B. Cowgill, L. Bogart, R. Corona, G. Ryan et al., “Parents’ Disclosure of Their HIV Infection to Their Children in the Context of the Family,” AIDS and Behavior, Vol. 14, No. 5, 2010, pp. 1095-1105.
- J. Rujumba, C. Mbasaalaki-Mwaka and G. Ndeezi, “Challenges Faced by Health Workers in Providing Counselling Services to HIV-Positive Children in Uganda: A Descriptive Study,” Journal of the International AIDS Society, Vol. 13, No. 1, 2010, p. 9. doi:10.1186/1758-2652-13-9
- J. Rwemisisi, B. Wolff, A. Coutinho, H. Grosskurth and J. Whitworth, “‘What If They Ask How I Got It?’ Dilemmas of Disclosing Parental HIV Status and Testing Children for HIV in Uganda,” Health Policy Plan, Vol. 23, No. 1, 2008, pp. 36-42. doi:10.1093/heapol/czm040
- A. C. Gerson, M. Joyner, P. Fosarelli, A. Butz, L. Wissow, et al., “Disclosure of HIV Diagnosis to Children: When, Where, Why, and How,” Journal of Pediatric Health Care: Official Publication of National Association of Pediatric Nurse Associates & Practitioners, Vol. 15, No. 4, 2001, pp. 161-167.
- L. Vaz, A. Corneli, J. Dulyx, S. Rennie, S. Omba, et al., “The Process of HIV Status Disclosure to HIV-Positive Youth in Kinshasa, Democratic Republic of the Congo,” AIDS Care: Psychological and Socio-Medical Aspects of AIDS/HIV, Vol. 20, No. 7, 2008, pp. 842-852.
- N. Hammami, C. Nostlinger, T. Hoeree, P. Lefevre, T. Jonckheer, et al., “Integrating Adherence to Highly Active Antiretroviral Therapy into Children’s Daily Lives: A Qualitative Study,” Pediatrics, Vol. 114, No. 5, 2004, pp. 591-597. doi:10.1542/peds.2004-0085
- F. Hejoaka, “Care and Secrecy: Being a Mother of Children Living with HIV in Burkina Faso,” Social Science & Medicine, Vol. 69, No. 6, 2009, pp. 869-876. doi:10.1016/j.socscimed.2009.05.041
- W. M. Nehring, F. R. Lashley and K. Malm, “Disclosing the Diagnosis of Pediatric HIV Infection: Mothers’ Views,” Journal for Specialists in Pediatric Nursing, Vol. 5, No. 1, 2000, pp. 5-14. doi:10.1111/j.1744-6155.2000.tb00081.x
- M. Bhattacharya, A. P. Dubey and M. Sharma, “Patterns of Diagnosis Disclosure and Its Correlates in HIV-Infected North Indian Children,” Journal of Tropical Pediatrics, Vol. 57, No. 6, 2010, pp. 405-411.
- F. Hejoaka, “HIV Disclosure to Children in Low-Resource Countries: A Forgotten Issue on the International AIDS Policy Agenda,” AIDS 2008-XVIII International AIDS Conferences, Mexico, 2008.

