Journal of Diabetes Mellitus
Vol.3 No.2(2013), Article ID:31495,4 pages DOI:10.4236/jdm.2013.32014
The “metabolic syndrome index”: A novel, comprehensive method for evaluating the efficacy of diabetes prevention programs
![]()
1Department of Epidemiology and Biostatistics, University of Nevada, Las Vegas, USA
2Department of Anthropology, University of Nevada, Las Vegas, USA; *Corresponding Author: daniel.benyshek@unlv.edu
Copyright © 2013 Hongbin Jin, Daniel C. Benyshek. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received 30 March 2013; revised 29 April 2013; accepted 7 May 2013
Keywords: Evaluation; Metabolic Syndrome; Type 2 Diabetes Prevention; T2D
ABSTRACT
A myriad of diabetes prevention programs are carried out worldwide to fight against the current type 2 diabetes (T2D) pandemic. The lack of a unified criterion for evaluating the efficacy of T2D prevention programs, however, makes the interpretation of prevention program results difficult, and hinders clear and direct comparisons of different prevention programs. Metabolic syndrome is a strong indicator for diabetes and its complications, holding great promise to become the basis of an intervention evaluation method. The Metabolic Syndrome Index (MSI), proposed here, quantifies the metabolic risk for developing T2D and its complications. The MSI is a novel scale for evaluating the efficacy of diabetes prevention programs because it is a systematic, comprehensive, and stable indicator that reflects the metabolic risk reduction for diabetes and its complications at multiple levels and dimensions.
1. INTRODUCTION
In epidemiology, population attributable risk is the common method to describe risk reduction for a disease or an unhealthy condition [1]. However, this method is not applicable for most type 2 diabetes (T2D) prevention programs that involve intensive lifestyle intervention because these programs usually do not include a control group due to the nature of their study designs and ethical concerns. Currently, percent weight loss is a widely used indicator to evaluate the efficacy of T2D prevention programs because of its clear relationship with diet modifycation and exercise—two common constructs in lifestyle intervention [2,3]. Yet, weight change alone may not fully reflect the efficacy of lifestyle intervention in terms of improving prediabetes conditions and reducing the risk of developing T2D and its complications. Recently, Feller and colleagues pointed out that waist circumference provides a better measure of diabetes risk than BMI because development of T2D is especially influenced by visceral fat, which is more metabolically active and produces more hormones and cytokines than other adipose tissues [4]. In addition, many research studies have confirmed that beneficial changes in T2D incidence can be achieved independently of weight loss [5-7].
Metabolic syndrome, which is associated with central obesity and insulin resistance, among several other cardiometabolic components (Table 1), has been demonstrated as a reliable predictor of T2D and cardiovascu lardiseases [7-12]. Since cardiovascular diseases such as heart disease and stroke are the major diabetes complications, metabolic syndrome holds great promise to become the basis for measuring risk reduction for diabetes and its complications resulting from lifestyle intervenetions. Many research studies have included the pre-post measurement of metabolic syndrome components in their reports and confirmed that symptoms of metabolic syndrome can be improved by lifestyle interventions [13-18]. However, analysis of each of these components separately may mask or distort the comprehensive change across symptoms because all metabolic syndrome components are mutually linked with strong interactions. Application of a Metabolic Syndrome Index (MSI) overcomes this disadvantage because it incorporatesall metabolic syndrome components into a single, stable, and comprehensive score, reflecting the metabolic risk

Table 1. Diagnostic criteria for metabolic syndrome.
for diabetes and its complications.
Because metabolic syndrome is a cluster of metabolic risk factors that contribute greatly to the development of T2D, these syndrome components can be thought of as constituting a network of symptoms that reflect the risk for type 2 diabetes and its complications. The MSI is a scaleof that network. The definition and clinical cutoff values of metabolic syndrome was adopted from the criteria proposed by the American Heart Association (AHA) and the National Heart, Lung, and Blood Institute (NHLBI) in 2005 [11].
2. METHODS
The MSI, proposed here, is a five-point scale that assigns one point to each of the five metabolic syndrome components—waist circumference, blood pressure, triglycerides, high-density lipoprotein (HDL) cholesterol, and fasting blood glucose (Table 1). The five components are assumed to be equally important for diabetes and its complications because each component is assigned one point only. The validity of index’s component equality is assured by the AHA/NHLBI criteria, which is defined as the presence of any three or more of the syndrome’s five components. In this way the proposed MSI accounts for the clinical significance of each of the syndrome’s risk factor cutoff values, and acknowledges the equal weight placed on each of the syndrome’s diagnostic components.
Calculation of the MSI for an individual could not be simpler: a one point score is assigned to any risk factor that exceeds the metabolic syndrome cutoff value, and a score of zero is assigned to any risk factor value that falls below the cutoff value. The MSI value is simply the sum of the scores assigned each of the syndromes five components (Figure 1). A range from zero to five quantifies the metabolic risk for diabetes and its complications which can be reduced by lifestyle intervention. A MSI value should be calculated at least twice (before and after intervention) in order to calculate the percentage of the risk reduction potentially resulting from the intervene-
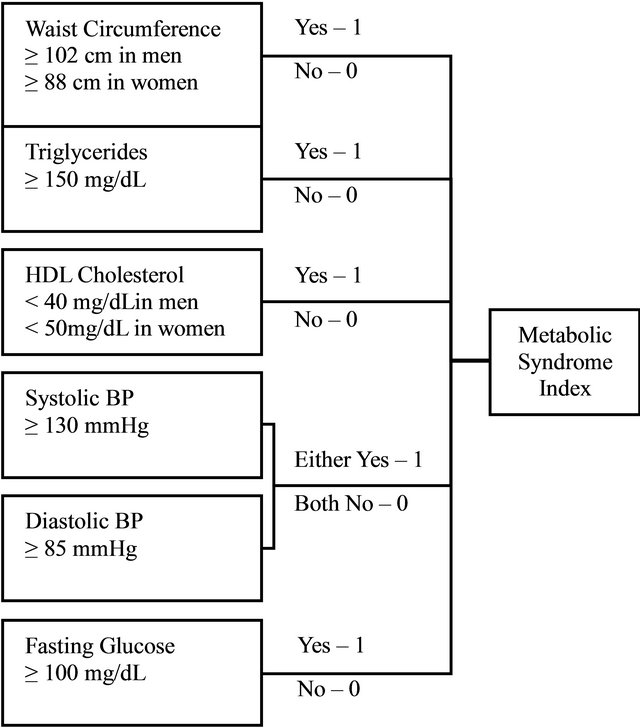
Figure 1. Metabolic syndrome index calculation flow chart.
tion. Extra measurements during the intervention will provide more information in understanding the responses of metabolic syndrome components to lifestyle interventions and the trend of the MSI.
The percentage of a MSI reduction quantifies the amount of risk for diabetes and its complications that has been avoided. In order to interpret the MSI better, we propose to use a new concept—metabolic risk—in describing the risk reduction caused by lifestyle intervenetion. Metabolic risk for diabetes and its complications is generally attributable to environmental and behavioral factors; in other words, risk that can be modified by lifestyle interventions. This risk reduction can be calculated and expressed as a single MSI value. Additionally, adoption of the MSI value will likely prove convenient for public health professionals because it is a direct reflection of the efficacy of T2D prevention interventions.
3. DISCUSSION
Lifestyle intervention for diabetes prevention programs is a multidimensional process with a series of health promotion strategies at multiple levels. The complexity of diabetes prevention programs necessitates a comprehensive and integrated method to evaluate their efficacy. Unlike weight loss, metabolic syndrome components provide multiple parameters that cover more aspects of risk reduction caused by lifestyle intervention and can provide a more comprehensive evaluation of the strengths and weaknesses of a given diabetes intervenetion. Utilization of a MSI incorporates and integrates diverse risk measures into one single parameter that can comprehensivelyquantify the efficacy of that program— both for individual participants, and for the intervention participant group as a whole.
Because the MSI being proposed here is derived from the sum of dichotomous (yes/no) variables reflecting established diagnostic cutoff values for the five risk factor components of metabolic syndrome, it might be argued that the MSI lacks sensitivity to improvements in component risk factors that do not reach these cutoff values. What the MSI may lack in sensitivity, however, it makes up in reliability. The fact that the metabolic syndrome identifies a suite of specific risk factors (present/ absent) that have been shown to accurately predict future risk of developing T2D, suggests that any reduction in the MSI constitutes a clear and significant reduction in the future risk for developing T2D. The same cannot be said with respect to improvements in the absolute values of metabolic syndrome risk factor components that do not meet diagnostic cutoff values. As a result, we would suggest that the reliability of the MSI to predict clear and meaningful reductions in the risk of developing T2D sets an appropriate standard for the evaluation of T2D prevention program efficacy.
Application of the MSI provides summarized information in addition to metabolic syndrome components in evaluating diabetes prevention programs. It also serves as a comparison for other evaluation tools used in T2D prevention programs by reporting the amount of metabolic risk reduction for diabetes and its complications that has been achieved. Furthermore, the changes in each of the MSI components provides a more comprehensive evaluation of diabetes prevention program efficacy, showing great potential for helping public health professionals individualize and optimize program curriculums for different target populations. Conventional usage of the MSI in T2D research will establish a unified criterion in evaluating T2D prevention programs and facilitate efficacy comparisons among disparate diabetes interventions.
REFERENCES
- Fleiss, J.L., Levin, B. and Cho Paik, M. (2003) Statistical methods for rates and proportions. 3rd Edition, WileyInterscience, Hoboken.
- Hamman, R.F., Wing, R.R., Edelstein, S.L., Lachin, J.M., Bray, G.A., Delahanty, L.D. and Hoskin, A.M. (2006) Effect of weight loss with lifestyle intervention on risk of diabetes. Diabetes Care, 42, 2102-2107. doi:10.2337/dc06-0560
- Ali, M.K., Echouffo-Tcheugui, J. and Williamson, D.F. (2012) How effective were lifestyle interventions in realworld settings that were modeled on the Diabetes Prevention Program? Health Affairs, 31, 67-75. doi:10.1377/hlthaff.2011.1009
- Feller, S., Boeing, H. and Pischon, T. (2010) Body mass index, waist circumference, and the risk of type 2 diabetes mellitus: Implications for routine clinical practice. DeutschesÄrzteblatt International, 107, 470-476. doi:10.3238/arztebl.2010.0470
- Pan, X.R., Li, G.W., Hu, Y.H., Wang, J.X., Yang, W.Y., An, Z.X. and Hu, Z.X. (1997) Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance: The Da Qing IGT and Diabetes Study. Diabetes Care, 20, 537-544. doi:10.2337/diacare.20.4.537
- Tuomilehto, J., Lindström, J., Eriksson, J.G., Valle, T.T., Hämäläinen, H., Ilanne-Parikka, P. and Keinänen-Kiukaanniemi, S. (2001) Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. The New England Journal of Medicine, 344, 1343-1350. doi:10.1056/NEJM200105033441801
- Ramachandran, A., Snehalatha, C., Mary, S., Mukesh, B., Bhaskar, A.D. and Vijay, V. (2006) The Indian Diabetes Prevention Programme shows that lifestyle modification and metformin prevent type 2 diabetes in Asian Indian subjects with impaired glucose tolerance (IDPP-1). Diabetologia, 49, 289-297. doi:10.1007/s00125-005-0097-z
- Lorenzo, C., Okoloise, M., Williams, K., Stern, M.P. and Haffner, S.M. (2003) The metabolic syndrome as predictor of type 2 diabetes. Diabetes Care, 26, 3153-3159. doi:10.2337/diacare.26.11.3153
- Grundy, S.M., Brewer, B.H., Cleeman, J.I., Smith, S.C. and Lenfant, C. (2004) Definition of metabolic syndrome, report of the National Heart, Lung, and Blood Institute/ American Heart Association Conference on Scientific Issues Related to Definition. Circulation, 109, 433-438. doi:10.1161/01.CIR.0000111245.75752.C6
- Alberti, K.G. and Zimmet, P.Z. (1998) Definition, diagnosis and classification ofdiabetes mellitus and its complications, part 1: Diagnosis and classificationof diabetes mellitus provisional report of a WHO consultation. Diabetic Medicine, 15, 539-553. doi:10.1002/(SICI)1096-9136(199807)15:7<539::AID-DIA668>3.0.CO;2-S
- Grundy, S.M., Cleeman, J.I., Daniels, S.R., Donato, K.A., Eckel, R.H., Franklin, B.A. and Gordon, D.J. (2005) Diagnosis and management of the metabolic syndrome, an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Critical Pathways in Cardiology, 4, 198-203.
- Wilson, P.W.F., D’Agostino, R.B., Parise, H., Sullivan, L. and Meigs, J.B. (2005) Metabolic syndrome as a precursor of cardiovascular disease and type 2 diabetes. Circulation, 112, 3066-3072.
- Christ, M., Iannello, C., Iannello, P.G. and Grimm, W. (2004) Effects of a weight reduction program with and without aerobic exercise in the metabolic syndrome. International Journal of Cardiology, 97, 115-122.
- Orchard, T.J., Temprosa, M., Goldberg, R., Haffner, S., Ratner, R., Marcovina, S. and Fowler, S. (2005) The effect of metformin and intensive lifestyle intervention on the metabolic syndrome: The diabetes prevention program randomized trial. Annuals of Internal Medicine, 142, 611-619. doi:10.7326/0003-4819-142-8-200504190-00009
- Okura, T., Nakata, Y., Ohkawara, K., Numao, S., Katayama, Y., Matsuo, T. and Tanaka, K. (2007) Effects of aerobic exercise on metabolic syndrome improvement in response to weight reduction. Obesity, 15, 2478-2484. doi:10.1038/oby.2007.294
- Muzio, F., Mondazzi, L., Harris, W.S., Sommariva, D. andBranchi, A. (2007) Effects of moderate variations in the macronutrient content of the diet on cardiovascular disease risk factors in obese patients with the metabolic syndrome. The American Journal of Clinical Nutrition, 86, 946-951.
- Meckling, K.A. and Sherfey, R. (2007) A randomized trial of a hypocaloric high-protein diet, with and without exercise, on weight loss, fitness, and markers of the metabolic syndrome in overweight and obese women. Applied Physiology, Nutrition, and Metabolism, 32, 743- 752. doi:10.1139/H07-059
- Rector, R.S., Warner, S.O., Liu, Y., Hinton, P.S., Sun, G.Y., Cox, R.H. and Stump, C.S. (2007) Exercise and diet induced weight loss improves measures of oxidative stress and insulin sensitivity in adults with characteristics of the metabolic syndrome. American Journal of Physiology, Endocrinal Metabolism, 293, E500-E506. doi:10.1152/ajpendo.00116.2007

