Open Journal of Medical Microbiology
Vol.2 No.3(2012), Article ID:22824,6 pages DOI:10.4236/ojmm.2012.23014
Pattern of Acute Parasitic Diarrhea in Children under Five Years of Age in Kathmandu, Nepal
1Department of Microbiology, Institute of Medicine, Tribhuvan University Teaching Hospital (TUTH), Kathmandum, Nepal
2Public Health Research Laboratory, Institute of Medicine, Tribhuvan University Teaching Hospital (TUTH), Kathmandu, Nepal
Email: *shamshulansari483@yahoo.com
Received July 15, 2012; revised August 22, 2012; accepted August 29, 2012
Keywords: Parasitic Diarrhea; Protozoa; Helminthes; TUTH; Nepal
ABSTRACT
Diarrheal diseases are major problem of developing countries. Though precise data on childhood mortality associated with diarrheal diseases in Nepal is not available, it has been estimated that approximately 25% of child death are associated with diarrheal disease, particularly acute diarrhea. The purpose of this study was to assess the incidence of parasitic pathogens causing acute diarrhea in children under 5 years of age. A total of 525 children with acute diarrhea in a children’s hospital of Kathmandu, Nepal were enrolled between April 2011 and September 2011. The higher prevalence of diarrhea was in the age group of less than 2 years. Out of total 525 enrolled cases, protozoal parasites were found in 10.7% (56/525) of cases and helminthic parasites were found in 1.3% (7/525) of cases. Highest prevalence of 60.3% (38/63) of parasitic infection was found in the age group of 6 - 24 months followed by 7.9% (5/63) in the age group of less than 6 months. Of the total enrolled cases E. histolytica were 6.7% (35/525) followed by Giardial lamblia 3.4% (18/525) and the least frequency was due to A. lumbricoides constituting 0.6% (3/525). The aim of this study was to know the parasitic agents causing acute diarrhea in children.
1. Introduction
Diarrhea is the condition of having three or more loose or liquid bowel movement per day. Diarrhea is defined by World Health Organization (WHO) as having 3 or more loose or liquid stools per day or as having more stools than is normal for that person [1]. Acute diarrhea, defined as an increased frequency of defecation (three or more times/day or at least 200 g of stool/day) lasting less than 14 days, may be accompanied by nausea, vomiting, abdominal cramping, clinically significant systemic symptoms, or malnutrition [2]. In 2009 diarrhea was estimated to have caused 1.5 million deaths in children under the age of 5 years [3]. Nepal being a developing country, diarrheal diseases are major problem. Though precise data on childhood mortality associated with diarrheal diseases in Nepal is not available, it has been estimated that approximately 25% of child death are associated with diarrheal diseases, particularly acute diarrhea [4]. The WHO Child Health Epidemiology Reference Group estimates that 16% of deaths in African children younger than five years are directly attributable to diarrheal diseases [5].
The incidence of pathogens causing diarrhea varies between developed and developing world setting. In developed countries about 70% of diarrheal cases are of viral (40% rotavirus), 10% - 20% of bacterial and <10% of protozoal origin [6-9]. In developing countries 50% - 60% cases are of bacterial (Enteropathogenic Esherichia coli 25%, Campylobacter jejuni 10% - 18%, Salmonella spp. and Shigella spp. 5% each), 35% of viral (15% - 25% rotavirus) origin, and in many the cause is unidentified or mixed [6-10]. Diarrhea, including that of parasitic origin, remains one of the most common illnesses among children and, as reported by the World Health Organization, is one of the major causes of infant and childhood mortality in developing countries [11]. Intestinal opportunistic parasitic infections are important causes of diarrhea which is a serious health problem in tropical regions. Giardia spp. and Cryptosporidium spp. are common parasitic causes of human diarrhea with the prevalence rate of 1% - 3% in the industrialized world and 4% - 17% in developing countries [12].
Many species of protozoan parasites live in the gastrointestinal tract, infecting some 3.5 billion individuals worldwide. Three species are of particular importance: Entamoeba histolytica, Giardia lamblia, and Cryptosporidium parvum [13]. The coccidian parasite Cyclospora cayetanensis is a newly recognized enteric pathogen causing prolonged diarrhea in humans [14,15]. It has been implicated as an important cause of diarrheal illness in the context of Nepal [16-19].
2. Methodology
This study was conducted at Tribhuvan University Teaching Hospital, Department of Microbiology-Public Health Research Laboratory. A total of 525 stool samples were collected from the children under 5 years of age visiting Kanti Children’s Hospital, Kathmandu, Nepal with acute diarrhea in the periods between April 2011 and September 2011. Written informed consent was obtained from the children’s parents or guardian before enrollment. Ethical improvement was taken from the Institutional Review Board (IRB), Institute of Medicine, Tribhuvan University Teaching Hospital, Kathmandu, Nepal.
2.1. Sampling
From each participating children, clinical data were obtained and stool sample were collected in a Clean, leak proof screw capped plastic container. About 5 ml of fresh stool specimen was collected from babies’ diapers or clean bed pans with a clean plastic spatula in specimen containers. Specimens were transported to the laboratory within half an hour for investigation following the standard laboratory protocol (WHO protocol) in the Public Health Research laboratory, Institute of medicine, Tribhuvan University Teaching Hospital, Maharajganj, Kathmandu.
2.2. Macroscopic Examination
The colour, consistency, presence of blood and mucus and any other abnormalities were observed macroscopically. A direct wet mount of faecal material, particularly with liquid or unformed stool, is the fastest method for detection of motile trophozoites of E. histolytica, Giardia and other intestinal parasites.
2.3. Microscopic Examination
A direct wet mount of liquid stool specimen was prepared in a drop of normal saline for the observation of pus cells, ova, cyst and trophozoites of any parasites. The presence of pus cells is one factor suggestive of invasive infection in cases of community acquired gastroenteritis. Iodine preparations of liquid stools were prepared in 5 times diluted Lugol’s iodine. 1 - 2 ml fecal suspension was placed in 12 ml conical centrifuge tube. Then Sheather’s sugar solution was added until tube was three-quarters filled. It was stirred vigorously with applicator stick. Tube was filled with sugar solution to 1 or 2 cm from the top. Then it was centrifuged at 5000 rpm for 10 minutes. Surface material was transferred to microscopic slide by means of a wire loop. It was covered with coverslip and observed with high power. Smear was also prepared for the modified Kinyoun’s acid-fast staining [20].
2.4. Analysis
Differences in proportions were assessed by Chi-square test. P values < 0.05 were considered statistically significant.
3. Result
A total of 525 diarrheal stools of the children under five years of age visiting Kanti Children’s Hospital Kathmandu, from April 2011 to September 2011 were enrolled for the study. The samples were collected from the children with acute diarrhea with or without abdominal pain, nausea, vomiting, fever, and with or without mucus and/or blood in stools. Among total enrolled cases in the study, 64.2% (337/525) were male and 35.8% (188/525) were female. Out of total 525 enrolled cases, 61.5% (323/525) were from IPD and 38.5% (202/525) were from OPD.
The higher prevalence of diarrhea was in the age group of less than 2 years among which the prevalence was highest 69.9% (367/525) in the age group of 6 - 24 months, 19.2% (101/525) in the age group of less than 6 months and the least prevalence of 2.7% (14/525) was found in the age group of 49 - 60 months (Table 1). The prevalence of diarrhea in less than 2 years of age was found to be statistically significant (P < 0.01).
Out of total 525 enrolled cases, protozoal parasites were found in 10.7% (56/525) of cases and helminthic parasites were found in 1.3% (7/525) of cases while 88% (462/525) of cases were due to other than parasites (Figure 1). Parasites infected cases were 77.8% (49/63) among male while 22.2% (14/63) were among female.
Highest prevalence of 60.3% (38/63) of parasitic infection was found in the age group of 6 - 24 months followed by 7.9% (5/63) in the age group of less than 6
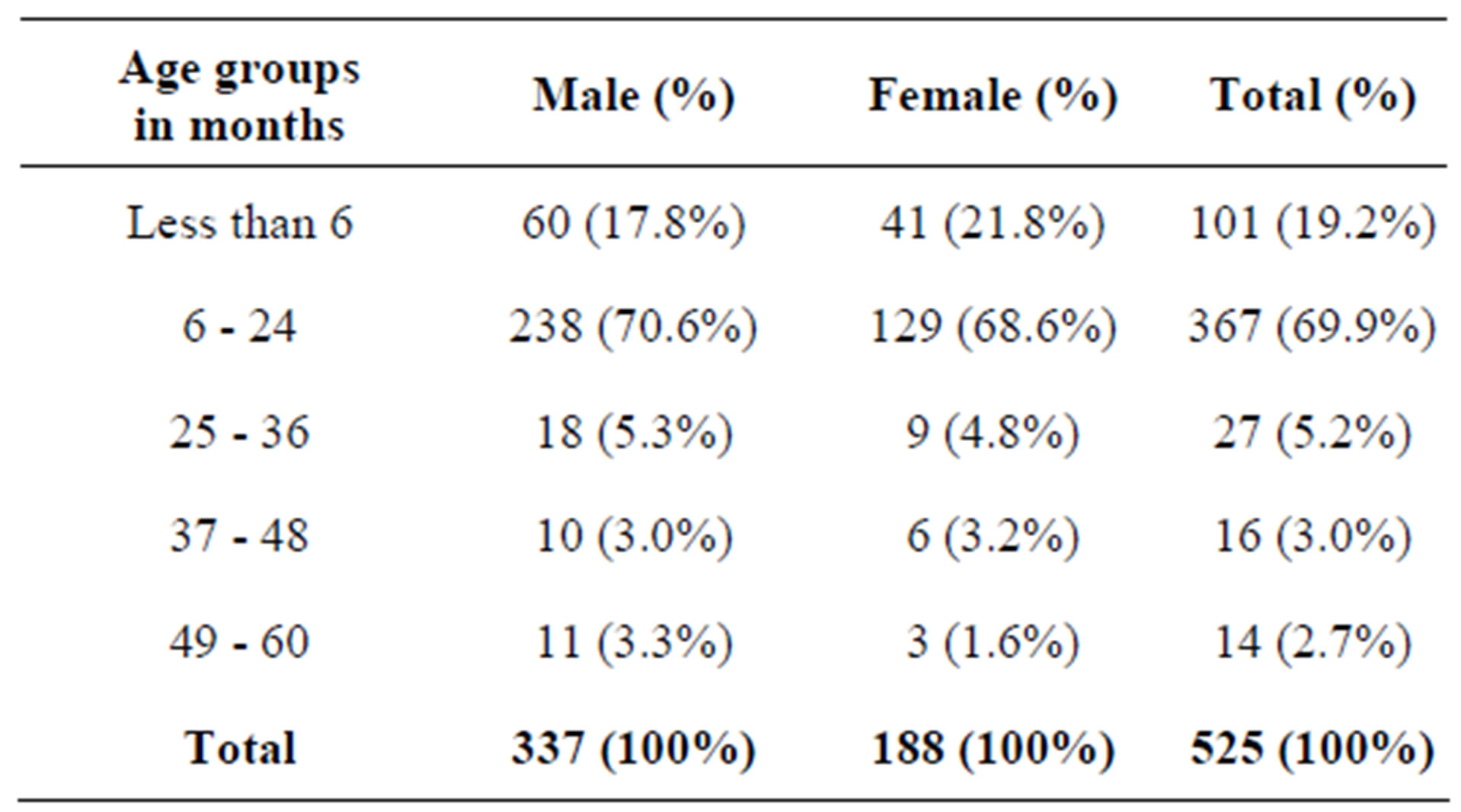
Table 1. Age and gender wise distribution of diarrheal cases.
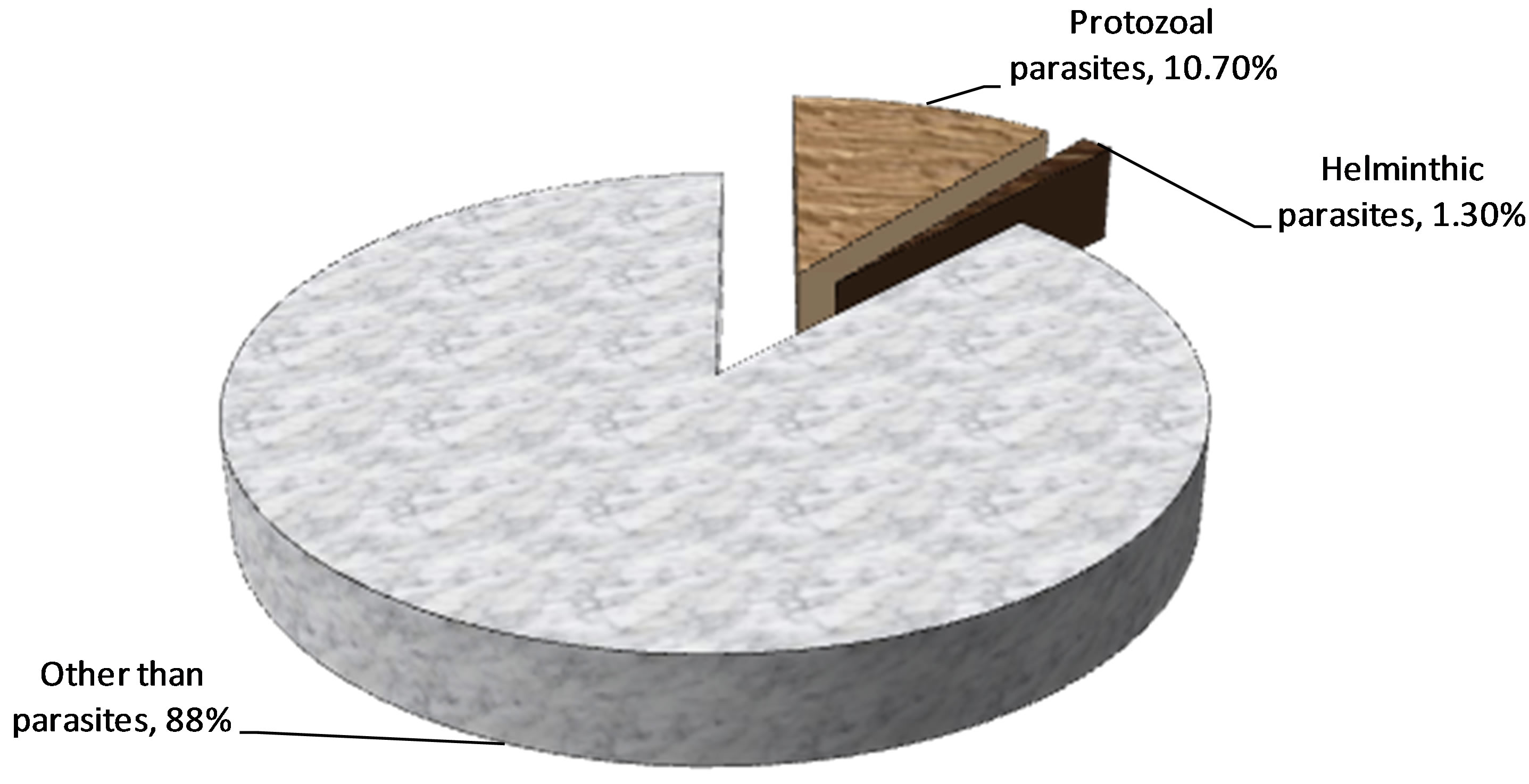
Figure 1. Distribution of parasitic positive cases.
months and the least prevalence of 6.3% (4/63) were in the age group of 49 - 60 months as shown in Figure 2. Occurrence of entero-parasites in children below 2 years of age was statistically significant than in those above 2 years of age (P < 0.01).
Of the total enrolled cases E. histolytica were 6.7% (35/525) followed by Giardial lamblia 3.4% (18/525), H. nana 0.7% (4/525) and Cyclospora cayetanensis and A. lumbricoides each constituting 0.6% (3/525) as depicted in Figure 3. The protozoal infected cases over helminthic infected cases was found to be statistically significant (P < 0.01).
4. Discussion
Diarrheal disease remains one of the largest health problems in many parts of the world. The disease is often mild and self-limiting but, particularly in the elderly and young children, the symptoms may be very severe. Studies in developing countries have shown that children in the first 2 years of the life may have up to 10 episodes of diarrheal disease, often with significant mortality [21]. Diarrheal disease occupied the second place among the top ten diseases in Nepal [22]. This study was conducted to find out the current trend of entero-parasites causing acute diarrhea in children under 5 years of age. In this study, 525 cases with acute diarrhea were processed for this study who visited Kanti Children’s Hospital between April 2011 and September 2011. 337 cases were male and 188 were female with male to female ratio being 1.79:1. Children below 5 years of age were enrolled in this study. In present study, among the total cases of 525, 61.5% (323/525) were from IPD and 38.5% (202/525) were from OPD.
The maximum number of samples were from the age group of less than 2 years in which the age group of 6 - 24 months constitutes maximum number (69.9%) followed by the age group of less than 6 months (19.2%). This indicates that the prevalence of diarrhea is higher in children below 2 years of age. Among the total cases enrolled, the prevalence of protozoal parasite was 10.7% (56/525) and helminthic parasite was 1.3% (7/525) and 88% (280/525) of cases were due to other than parasitic causes in this study.
Higher frequency of diarrhea was seen in male which was 64.2% (337/525) than female 35.8% (188/525). Similarly Shariff et al. in 2003 in children under 5 years of age in eastern Nepal found the prevalence of 67.5% of diarrhea in males [23]. Higher prevalence of diarrhea in male was also reported to be 56.4% by J. B. Sherchand et al. in Nepal [24], 57% by Eileen J. Klein et al. in Missouri [25] and 61.4% by Sabrina J. Moyo et al. in Tanzania [26]. Similarly the frequency of diarrhea was more in the age group less than 2 years of age among which the age group of 6 - 24 months was highest 69.9% (367/525) than the age group of less than 6 months 19.2% (101/ 525). The frequency of diarrhea in age less than 2 years was found to be statistically significant (P < 0.01). Similar study by M. Shariff et al. (2003) in children under 5 years of age in eastern Nepal showed the majority of diarrheal cases (70.9%) were observed in patients between 6 months and 2 years of age [23].
Higher frequency of parasites infected cases were male (77.8%) and 22.2% were female. Ogunlesi Tinuade et al. (2006) from Nigeria also found the higher prevalence of 57.1% in male whereas 42.9% of parasite positive cases were in female [27], which is consistent with our findings.
In this study the children less than 2 years were more infected than other age group among which the age between 6 - 24 months were the most infected age group followed by less than 6 months of age. The incidence of high entero-parasites among the age less than 2 years was found to be statistically significant (P < 0.01). It appeared
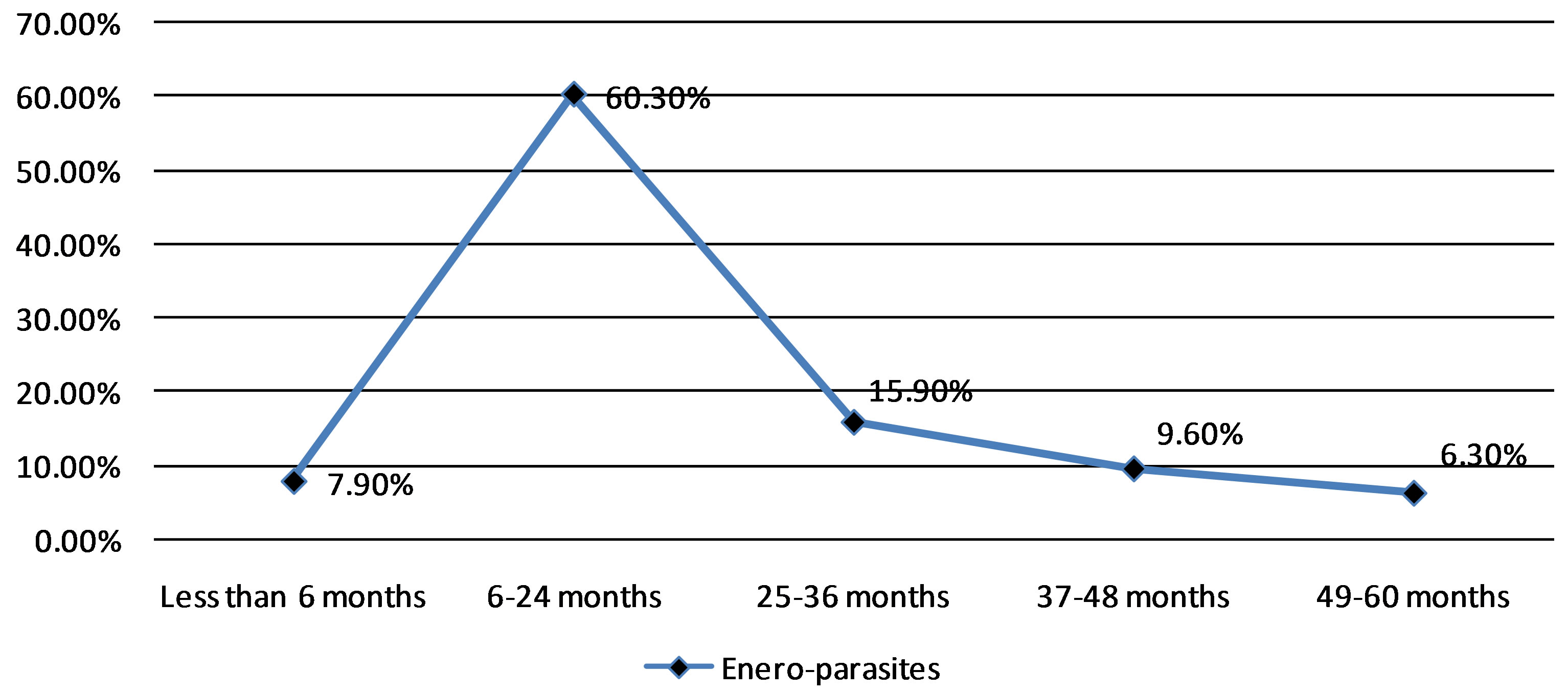
Figure 2. Distribution of entero-parasite positive cases in different age groups.
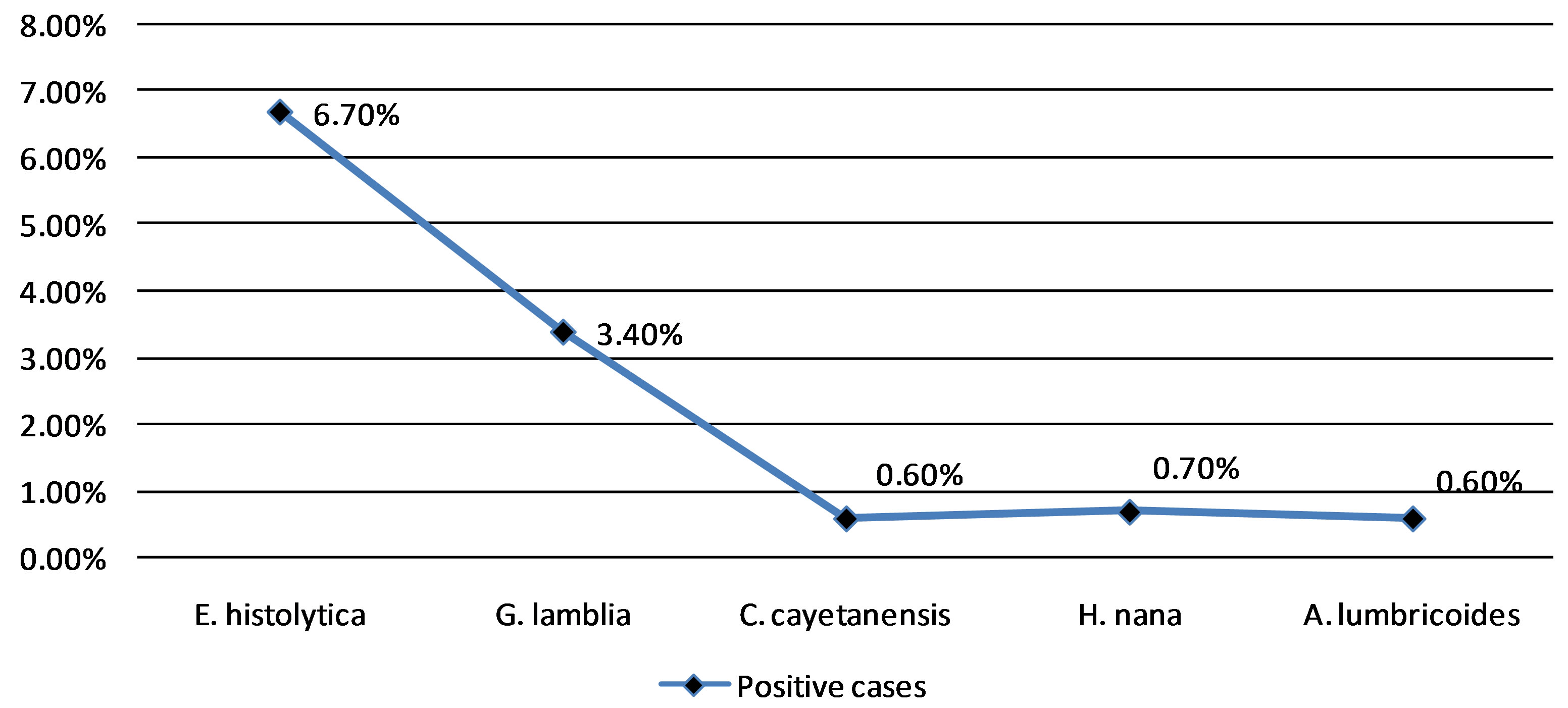
Figure 3. Distribution of different positive parasites cases.
that infants below 6 months of age were initially protected to some extent by maternal antibodies against severe diarrhea, and they seem to have acquired adequate immunity between 12 and 16 months of age. The greater risk of infants and young children in the period between 6 - 12 months with declined levels of maternal antibodies to infection have been documented [24].
Despite the government policy for anti-helminthic program and health education program launched at community level, the intestinal parasite infestation still remains the major cause of diarrheal diseases in children [24]. In present study too the parasitic infestation was the major etiologic agent that causes diarrhea in children. The protozoa accounted for 10.7% whereas helminthes accounted for 1.3%. The most constituted parasite causing acute diarrhea was E. histolytica constituting 6.7% (35/525) followed by Giardial lamblia 3.4% (18/525), H. nana 0.7% (4/525) and Cyclospora cayetanensis and A. lumbricoides each constituting 0.6% (3/525). Ogbonnaya Ogbu et al. in 2006 [28], found E. histolytica from 3.3% cases and G. lamblia from 2.7% of cases which concurs with our study. Similarly Mohammad Youssef et al.
(1994) reported E. histolytica from 4.9% of cases [29] and Nazek Al-Gallas et al. detected 2.6% of G. lamblia [30]. Inacio M. Mandomando et al. found 9.3% A. lumbricoídes and 2.5% G. lamblia [31] and S. Das et al. found 4.8% E. hystolytica, 6.3% G. intestinalis, 3.6% hookworm and 4.3% roundworm as the major agents of gastrointestinal disturbance especially seen in school age children [32].
The low positivity with helminthic parasites in our study may be due to the government policy for antihelminthic program launched at community level. Apart from this, primary school children in selected districts are being provided with deworming tablets twice yearly by World Food Program, Plan Nepal and Save the Children, US [33].
5. Conclusion
The frequency of parasitic diarrhea was higher in male children compared to female children. The study showed that the age group 6 - 24 months were found to be the most infected group among children. The frequency of E. histolytica infected cases were highest among the parasite infected cases.
6. Acknowledgements
We are deeply grateful to Prof. Dr. Basista Prasad Rijal, Professor of Department of Microbiology, Insitute of Medicine, Tribhuvan University, for his continuous guidance.
We are also grateful to all the working staffs, doctors and Nursing In-charge of oral rehydration therapy ward and the subjects of this study of Kanti Children’s Hospital, Kathmandu, Nepal.
REFERENCES
- World Health Organization, “Diarrhea,” 2007.
- N. M. Thielman and R. L. Guerrant, “Acute Infectious Diarrhea,” The New England Journal of Medicine, Vol. 350, No. 1, 2004, pp. 38-47. doi:10.1056/NEJMcp031534
- World Health Organization, “Diarrheal Disease,” 2009. http/whqlibdoc.who,int(pdf)
- R. Maharjan, B. Lekhak, C. D. Shrestha and J. Shrestha, “Detection of Enteric Bacterial Pathogens (Vibrio cholerae and Escherichia coli O157) in Childhood Diarrhoeal Cases,” Scientific World, Vol. 5, No. 5, 2007, pp. 23-26.
- K. Reither, R. Ignatius, T. Weitzel, et al., “Acute Childhood Diarrhoea in Northern Ghana: Epidemiological, Clinical and Microbiological Characteristics,” BMC Infectious Diseases, Vol. 7, 2007, pp. 104-111.
- A. C. Cheng, J. R. McDonald and N. M. Thielman, “Infectious Diarrhea in Developed and Developing Countries,” Journal of Clinical Gastroenterology, Vol. 39, No. 9, 2005, pp. 757-773.
- E. J. Elliott, “Acute Gastroenteritis in Children,” British Medical Journal (BMJ), Vol. 334, No. 7583, 2007, pp. 35-40. doi:10.1136/bmj.39036.406169.80
- M. E. Wilson, “Diarrhea in Nontravelers: Risk and Etiology,” Clinical Infectious Diseases, Vol. 41, No. 8, 2005, pp. S541-S560. doi:10.1086/432949
- N. A. Cunliffe, P. E. Kilgore, J. S. Breasee, et al., “Epidemiology of Rotavirus Diarrhea in Africa: A Review to Assess the Need for Rotavirus Immunization,” Bulletin of the World Health Organization, Vol. 76, No. 5, 1998, pp. 525-537.
- M. Naghipour, T. Nakgomi and O. Nakagomi, “Issues with Reducing the Rotavirus Associated Mortality by Vaccination in Developing Countries,” Vaccine, Vol. 26, No. 26, 2008, pp. 3236-3241. doi:10.1016/j.vaccine.2008.04.004
- C. Boschi-Pinto, L. Velebit and K. Shibuya, “Estimating Child Mortality Due to Diarrhoea in Developing Countries,” Bulletin of the World Health Organization, Vol. 86, No. 9, 2008, pp. 710-717.
- A. Hörman, H. Korpela, J. Sutinen, et al., “ Meta-Analysis in Assessment of the Prevalence and Annual Incidence of Giardia spp. and Cryptosporidium spp. Infections in Humans in the Nordic Countries,” International Journal for Parasitology, Vol. 34, No. 12, 2004, pp. 1337-1346. doi:10.1016/j.ijpara.2004.08.009
- A. Al-Bwardy, S. Ramia, R. Al-Frayh, et al., “Bacterial, Parasitic and Viral Enteropathogens Associated with Diarrhoea in Saudi Children,” Annals of Tropical Paediatrics, Vol. 8, No. 1, 1988, pp. 26-30.
- D. R. Shlim, M. T. Cohen, M. Eaton, et al., “An AlgaeLike Organism Associated with an Outbreak of Prolonged Diarrhea among Foreigners in Nepal,” The American Journal of Tropical Medicine and Hygiene, Vol. 45, No. 3, 1991, pp. 383-389.
- Y. R. Ortega, C. R. Sterling, et al., “Cyclospora Species— A New Protozoan Pathogen of Humans,” The New England Journal of Medicine, Vol. 328, No. 18, 1993, pp. 1308-1312. doi:10.1056/NEJM199305063281804
- C. W. Hoge, P. Echeverria, R. Rajah, et al., “Prevalence of Cyclospora Species and Other Enteric Pathogens among Children Less than 5 Years of Age in Nepal,” Journal of Clinical Microbiology, Vol. 33, No. 11, 1995, pp. 3058- 3060.
- D. R. Shlim, C. W. Hoge, R. Rajah, et al., “Persistent High Risk of Diarrhea among Foreigners in Nepal during the First 2 Years of Residence,” Clinical Infectious Diseases, Vol. 29, No. 3, 1999, pp. 613-616. doi:10.1086/598642
- J. B. Sherchand and J. H. Cross, “Emerging Pathogen Cyclospora cayetanensis Infection in Nepal,” Southeast Asian Journal of Tropical Medicine and Public Health, Vol. 32, Suppl. 2, 2001, pp. 143-150.
- J. B. Sherchand and J. H. Cross, “Parasitic Epidemiological Studies of Cyclospora cayetanesis in Nepal,” Southeast Asian Journal of Tropical Medicine and Public Health, Vol. 35, Suppl. 1, 2004, pp. 12-19.
- D. T. John and W. A. Petri, “Markell and Voge’s Medical Parasitology,” 9th Edition, Saunders Elsevier, St. Louis, 2006.
- R. E. Black, “Persistent Diarrhea in Children in Developing Countries,” The Pediatric Infectious Disease Journal, Vol. 12, No. 9, 1993, pp. 751-761. doi:10.1097/00006454-199309000-00010
- Population Division, Ministry of Health and Population, Government of Nepal, “Nepal Population Report,” Kathmandu, 2007, pp. 77-100.
- M. Shariff, M. Deb and R. Singh, “A Study of Diarrhoea among Children in Eastern Nepal with Special Reference to Rotavirus,” Indian Journal of Medical Microbiology, Vol. 21, No. 2, 2003, pp. 87-90.
- J. B. Sherchand, M. Yokoo, O. Sherchand, A. R. Pant and O. Nakagomi, “Burden of Enteropathogens Associated Diarrheal Diseases in Children Hospital, Nepal,” Scientific World, Vol. 7, No. 7, 2009, pp. 71-75.
- E. J. Klein, D. R. Boster, J. R. Stapp, et al., “Diarrhea Etiology in a Children’s Hospital Emergency Department: A Prospective Cohort Study,” Clinical Infectious Diseases, Vol. 43, No. 7, 2006, pp. 807-813. doi:10.1086/507335
- S. J. Moyo, N. Gro, M. I. Matee1, J. Kitundu, et al., “Age Specific Aetiological Agents of Diarrhoea in Hospitalized Children Aged Less than Five Years in Dar es Salaam, Tanzania,” BMC Pediatrics, Vol. 11, 2011, pp. 19-24. doi:10.1186/1471-2431-11-19
- O. Tinuade, O. John, O. Saheed, et al., “Parasitic Etiology of Childhood Diarrhea,” Indian Journal of Pediatrics, Vol. 73, No. 12, 2006, pp. 1081-1084. doi:10.1007/BF02763049
- O. Ogbu, N. Agumadu, C. J. Uneke and E. S. Amadi, “Aetiology of Acute Infantile Diarrhoea in the SouthEastern Nigeria: An Assessment of Microbiological and Antibiotic Sensitivity Profile,” The Internet Journal of Third World Medicine, Vol. 7, No. 1, 2008, p. 2.
- M. Youssef, A. Shurman, et al., “Bacterial, Viral and Parasitic Enteric Pathogens Associated with Acute Diarrhea in Hospitalized Children from Northern Jordan,” FEMS Immunology and Medical Microbiology, Vol. 28, No. 3, 2000, pp. 257-263. doi:10.1111/j.1574-695X.2000.tb01485.x
- N. Al-Gallas, O. Bahri, A. Bouratbeen, A. B. Haasen and R. B. Aissa, “Etiology of Acute Diarrhea in Children and Adults in Tunis, Tunisia, with Emphasis on Diarrheagenic Escherichia coli: Prevalence, Phenotyping and Molecular Epidemiology,” The American Journal of Tropical Medicine and Hygiene, Vol. 77, No. 3, 2007, pp. 571-582.
- I. M. Mandomando, E. V. Macete, J. Ruiz, S. Sanz, et al., “Etiology of Diarrhea in Children Younger than 5 Years of Age Admitted in a Rural Hospital of Southern Mozambique,” The American Journal of Tropical Medicine and Hygiene, Vol. 76, No. 3, 2007, pp. 522-527.
- S. Das, R. Saha and S. Singhal, “Enteric Pathogens in north Indian Patients with Diarrhea,” Indian Journal of Community Medicine, Vol. 32, No. 1, 2007, pp. 27-31. doi:10.4103/0970-0218.53389
- Save the Children, “School Health and Nutrition Newsletter,” 2004. http://www.schoolsandhealth.org/Documents/Save%20the%20Childrens%20Schools%20and%20Health%20Newsletter%20November%202006.pdf
NOTES
*Corresponding author.

