World Journal of Cardiovascular Diseases
Vol.4 No.2(2014), Article ID:43219,6 pages DOI:10.4236/wjcd.2014.42013
Pulse palpation and limited joint mobility examination are better indicators than oscillometric measurement for diagnosing abnormal ankle-brachial index
Division of Medicine, Turku University Hospital, Turku, Finland
Email: laura.rantamaula@tyks.fi, *juha.varis@tyks.fi, Ilkka.kantola@tyks.fi
Copyright © 2014 Laura Rantamaula et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. In accordance of the Creative Commons Attribution License all Copyrights © 2014 are reserved for SCIRP and the owner of the intellectual property Laura Rantamaula et al. All Copyright © 2014 are guarded by law and by SCIRP as a guardian.
Received 18 October 2013; revised 25 November 2013; accepted 5 December 2013
KEYWORDS
Peripheral Artery Disease; Blood Pressure; Ankle-Brachial Index; Oscillometric ABI Measurement
ABSTRACT
Background: Peripheral artery disease (PAD) is the least recognized form of atherosclerosis and may even result in amputation if the diagnosis is delayed. Manual pulse palpation is the traditional way to diagnose PAD. Doppler ultrasonographic measurement of ankle-brachial index (ABI) is the gold standard diagnosing method but requires training and is not necessarily available as an outpatient procedure. Using automated oscillometric blood pressure devices has been suggested as an easier method for measuring the ABI. Methods: A single observer palpated the arterial dorsalis pedis, examined hand joints and measured the ABI of one hundred diabetic patients using both Doppler and oscillometric methods. The purpose of this study was to compare the oscillometric method and the manual diagnosing methods to the gold standard method of using a hand held Doppler device for measuring the ABI and detecting PAD. Results: ABI was abnormal in 24 patients (24%) (22 males, 2 females) when measured with the Doppler method. Of these 24 patients, the oscillometric method would have missed 12 giving 12 false negatives. We found that the sensitivity of the oscillometric method was 50.0% and specificity 90.8%. Clinical examination with palpation of ADP combined with limited joint mobility (LJM) scoring would have missed only four cases. Conclusions: Although the oscillometric method is easy and accessible, it is not sensitive enough to be used as the only method in measuring ABI. The simple and inexpensive ADP pulse palpation combined with testing for LMJ was able to find 20 of the 24 (83%) patients with an abnormal ABI measured by Doppler stethoscope.
1. INTRODUCTION
Peripheral artery disease (PAD) is the least recognized form of atherosclerosis compared to coronary and cerebrovascular disease [1]. Patients with PAD usually experience symptoms like claudication and ischemic pain in rest. However, PAD may be asymptomatic, especially in elderly patients with little exercise and in diabetic patients with peripheral neuropathy. The major risk factors for peripheral artery disease are diabetes mellitus, smoking and ageing [2,3]. Conservative diagnosis of PAD has been done by pulse palpation and testing the possible presence of limited joint mobility (LJM) syndrome. The treatment of PAD includes treatment of risk factors, smoking cessation and walking. Critical limb ischemia with ischemic rest pain or ischemic ulcerations requires revascularization to avoid amputation [4].
Ankle-brachial index (ABI) is a noninvasive screening test for peripheral artery disease. Both low and high values in ABI are markers for systemic atherosclerosis and increased risk of cardiovascular events [5]. An anklebrachial index of less than 0.9 is diagnostic for peripheral artery disease. A high (>1.3) ABI is a marker of arterial stiffness and media sclerosis [6].
The current gold standard for measuring of ABI is a hand-held Doppler stethoscope for auscultation of both the dorsal pedal (ADP) and posterior tibial (ATP) artery pulses while measuring the ordinary blood pressure in the arm. Its sensitivity is 79% and specificity 96% in detecting ≥ 50% reduction in vascular lumen [7]. This technique requires a trained performer and is not necessarily available as an outpatient procedure, which is the main reason for the lack of early diagnosis. In recent studies the usefulness of automated oscillometric blood pressure devices in measuring the ankle blood pressure, which would be an easier and less expensive method for measuring the ABI, has been clarified [8-16]. The aim of this study was to compare the oscillometric method and the traditional pulse palpation to the Doppler stethoscope in measuring ABI as a screening test in diabetic patients. As the presence of limited hand joint mobility syndrome (LJM) associates with vasculopathies, it was also examined in the study [17].
2. MATERIALS AND METHODS
One hundred patients with diabetes of varying duration were enrolled in the study in June-July 2010. Informed written consent was taken from each patient. A history of diabetes, hypertension, dyslipidemia, smoking and previously diagnosed PAD as well as current medication were recorded. Also the symptoms of intermittent claudication and pain in rest were recorded.
The pulses of ADP and ATP were palpated on both feet and the monofilament test performed. The patients were also tested for limited hand joint mobility (LJM) syndrome. LJM was assessed qualitatively by the same observer (L.R.) with the prayer maneuver; patients were asked to approximate the palmary surfaces of the fingers in a praying position with the fingers fanned and the wrists flexed. The possible LJM was classified using the Rosenbloom grading and then dichotomized, i.e. LJM score was either positive (including all Rosenbloom cases from II to IV) or negative [17]. The most recent values for GHbA1c and plasma cholesterol were recorded.
A single observer (LR) measured the ABI using both the Doppler and oscillometric methods. Doppler stethoscope was model 841-A (Parks Medical Electronics Inc, U.S.A.). The automated oscillometric device used was Omron M3 Intellisense (HEM-7051-E; Kyoto, Japan) with appropriate cuff size, and the Brachial pressure was measured in both arms using the oscillometric device and the higher average of three measurements was used in calculating the ABI. The ankle pressure was measured three times in both ankles with both methods, and the average of the three measurements was used in calculating the ABI. Before measurements the patients were at rest for at least 5 minutes and the measurements were taken with the patient in the supine position. The patients were asked not to exercise, smoke or have caffeinated drinks for three hours before the test. An ABI of less than 0.9 or greater than 1.3 was considered abnormal. A normal ABI result in the oscillometric method while the Doppler method gave an abnormal result, was considered a false negative (FN) and an abnormal oscillometric result while the Doppler ABI was normal, a false positive (FP).
3. ETHICAL APPROVAL
The study was approved by the ethical committee of Turku Hospital District and Turku University.
4. STATISTICAL ANALYSIS
The continuous variables are expressed as mean (SD). Database management and statistical analysis were performed using SPSS software, version 16.0. Group differences in continuous variables were assessed with unpaired Student’s t test or one way analysis of variance as appropriate. Chi-square test was used for the comparison of two proportions. The cut-off level for statistical significance was set at P-value < 0.05. The normal distribution of the continuous variables were confirmed using Shapiro-Wilks’ test of normality. The significance of correlation between variables was determined by Pearson’s correlation analysis. Multivariate stepwise linear regression analysis was applied to assess independent predictors of the variables of interest, performed where the univariate p value was <0.05.
The positive predictive value was calculated as the number of true positive (TP) results divided by the number of all positive results [TP/(TP + FP)] and the negative predictive value as the number of true negative (TN) results divided by the number of all negative results [TN/(TN + FN)]. The sensitivity was calculated as the number of true positives divided by the number of true positives and false negatives [TP/(TP + FN)] and the specificity as the number of true negatives divided by the number of false positives and true negatives [TN/(FP + TN)].
5. RESULTS
One hundred patients (24 females and 76 males) were recruited from the out-patient clinics and the wards of the Department of Medicine in Turku University Hospital. The demographics of the patients are presented in Table 1. The duration of diabetes was less than 5 years in 23 patients, 5 - 10 years in 24 patients and over 10 years in 53 patients. The age of the patients varied between 18 and 81 years. Seventeen patients were current smokers with an average of 26.2 pack-years. The mean GHbA1c was 7.8 (1.5) %. Fifteen patients had experienced intermittent claudication. Right ADP pulse was palpable in 72 patients and left in 73 patients. Right ATP pulse was palpable in 64 patients and left in 60 patients. Seventeen
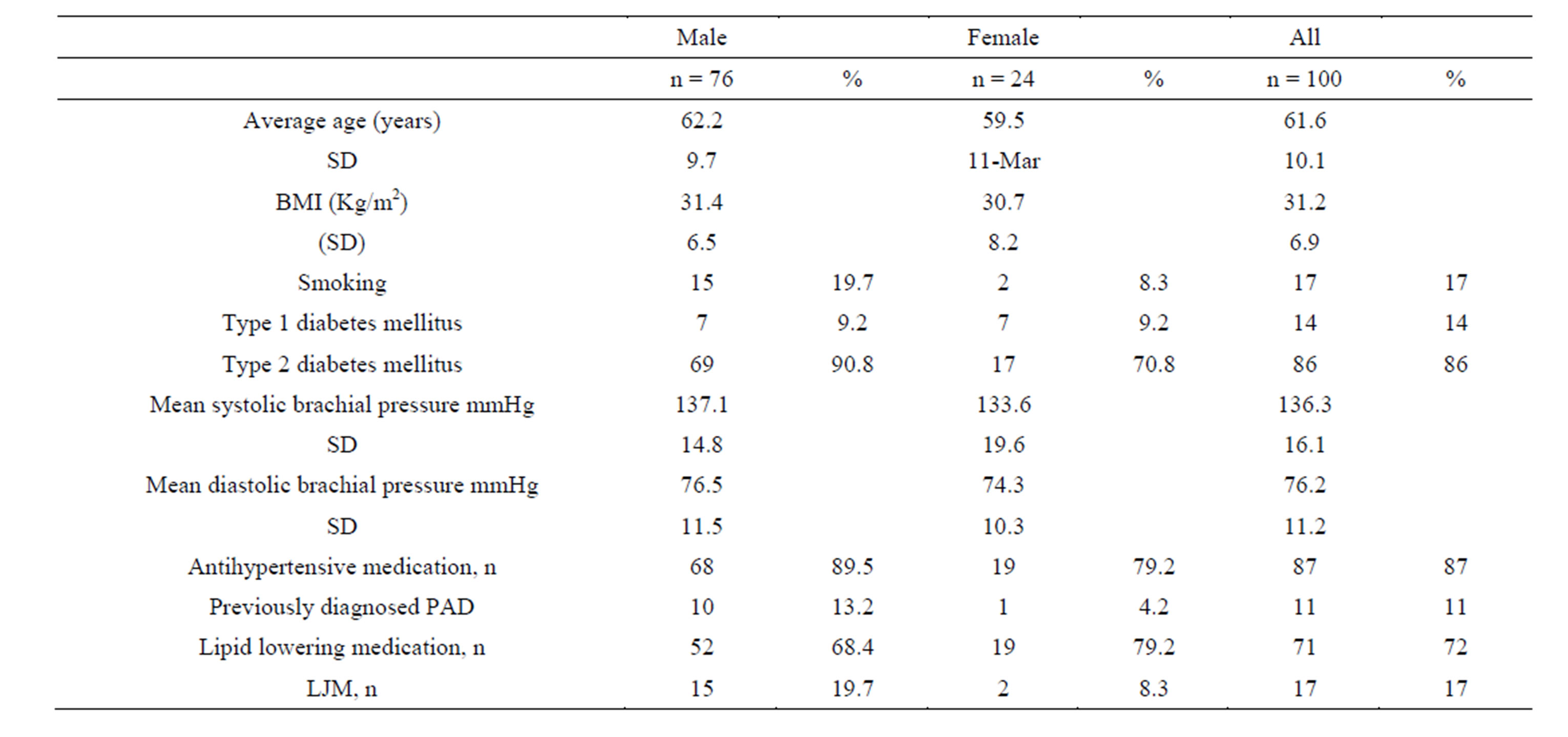
Table 1. Demographics of the patients.
patients showed limited joint mobility.
ABI was abnormal (less than 0.9 or greater than 1.3) in 24 patients (24.0%) (2 females) with the Doppler method and in 20 patients (20.0%) (3 females) with the oscillometric method. For ABI details please refer to Table 2. ABI was less than 0.9 in 20 (10.0%) ankles (13 patients) when measured with the Doppler method and in 14 (7.0%) ankles (10 patients) with the oscillometric method. It was greater than 1.3 in 17 (8.5%) ankles (11 patients) and 11 (5.5%) ankles (10 patients) with the Doppler and oscillometric methods, respectively. There was no value of ABI below which the oscillometric method would have found all abnormal values. The lowest ABI recorded with the Doppler method was 0.55. Mean ABI in the right side was 1.10 (0.17) and 1.13 (0.20) in the left side with the Doppler method. The oscillometric method gave a mean ABI of 1.13 (0.15) in the right and 1.13 (0.12) in the left side.
The ankle systolic pressure was over 300 mmHg in 3 ankles with the Doppler method and hence ABI could not be calculated but was considered abnormal, while the oscillometric method gave a low ABI of less than 0.9 in the same ankles. In one patient the ankle pressure with the Doppler method was 220 mmHg giving an ABI of 1.44, while the oscillometric systolic pressure was 134 mmHg and the ABI 0.88. No significant correlation was seen between ABI and sex, age, BMI, smoking or claudication symptoms.
The efficacy of pulse palpation, LJM testing and oscillometric method to detect abnormal ABI measured using the gold-standard Doppler method is described in detail in Table 3. Compared to Doppler method, the positive predictive value of the oscillometric method was 64% and the negative predictive value 88%. The sensitivity and specificity data is presented in Table 4. Sensitivity of the oscillometric method vs Doppler method as the gold standard was 50.0%, (43.2% in ankles) and the specificity 90.8%, (95.6% in ankles), respectively. Five patients had a true positive ABI in one ankle and a false negative in the other so they would have been classified as having abnormal ABI. Palpation of the pulses and testing of LJM yields a positive predictive value of 46.5% and a negative predictive value of 93.0% and the sensitivity of 83.3% and the specificity of 69.7%. The palpation of the ankle pulses as such yields the sensitivity of 73.9% and 64.9% (patients, ankles) and the specificity 81.8%, 82.8%, respectively. Testing of only LJM yields the sensitivity of 29.2% and the specificity of 86.8%. Both LJM and non-palpable pulses give the sensitivity of 21.7% and the specificity of 97.4%. Palpation of the ADP pulses, testing for LJM and measuring the oscillometric ABI yielded the sensitivity of 91.6% and the specificity of 63.2% (for details, see Table 4).
In linear regression analysis, a positive correlation between both the Doppler and oscillometric ABI of the right ankle and the ADP pulse palpability (Doppler: r = 0.325, p = 0.039, oscillometric: r = 0.479, p = 0.000) was seen. Also a positive correlation between the oscillometric ABI of the left ankle and the ADP pulse palpability (r = 0.296, p = 0.028) was seen. There was, however, no significant correlation between the left Doppler ABI and the ADP pulse palpability (r = 0.050, p = 0.664). The ADP pulse was not palpable in 10 of the 11 patients (90.9%) who had a low ABI in the right ankle, and in 7 of the 9 patients (77.8%) who had a low ABI in the left ankle.

Table 2. Pulse palpation status and ABI of the patients.
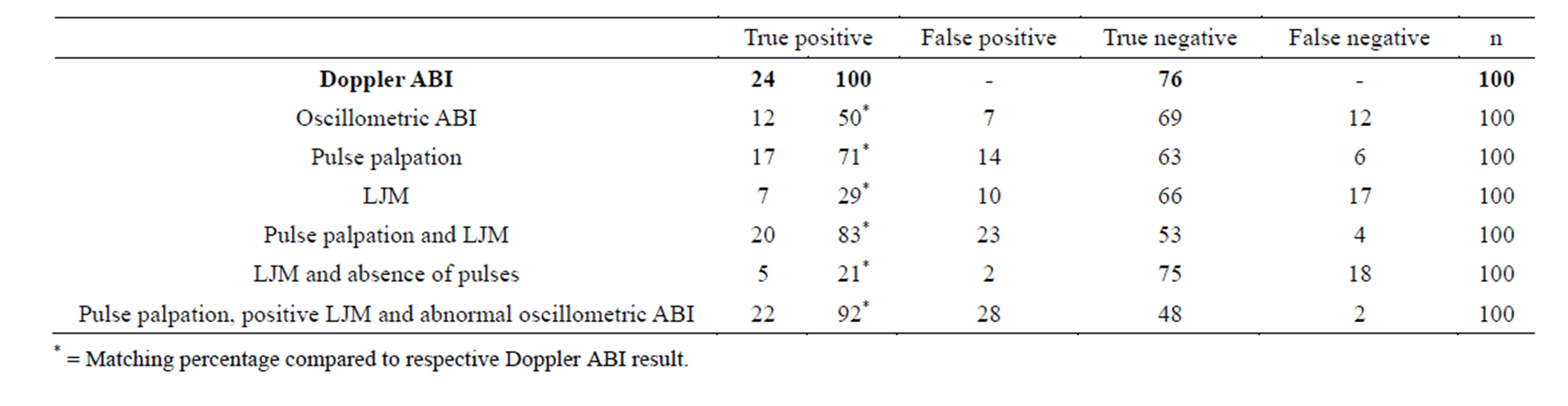
Table 3. Oscillometric ankle-brachial index (ABI), pulse palpation and limited joint mobility (LJM) results compared to gold-standard ABI results measured by Doppler method in one hundred patients.
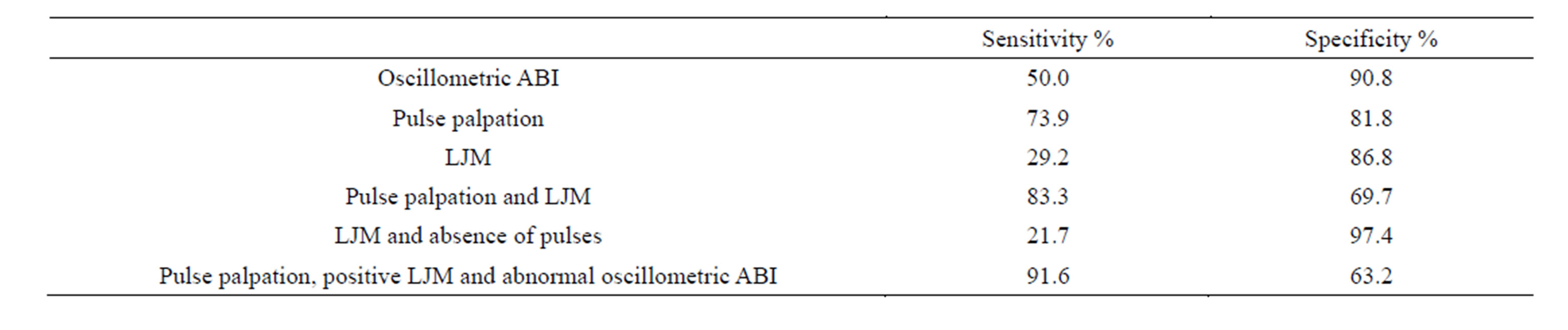
Table 4. The sensitivity and specificity of oscillometric ankle brachial index (ABI), pulse palpation and limited joint mobility (LJM) methods compared to gold-standard ABI testing by Doppler method in one hundred patients.
A negative correlation between the oscillometric ABI of both ankles and the presence of limited joint mobility of the hand was seen (r = −0.272, p = 0.002 in the right and r = −0.187, p = 0.048 in the left side). The ABI was abnormal (with the Doppler method) in 7 (41.0%) of the patients with LJM. A positive correlation in the linear regression analysis between limited joint mobility and both GHbA1c (r = 0.366, p = 0.000) and previously diagnosed PAD (r = 0.350, p = 0.000) was seen.
The overall incidence of an abnormal ABI was 24% in these 100 diabetic patients. The incidence was 41% among those who had LJM and 20.5% among those with no LJM.
6. DISCUSSION
We clarified the value of the ordinary oscillometric blood pressure monitor in evaluating ankle brachial index in diabetic patients. Its specificity was very good but sensitivity not high enough to be used as the only screening method of significant atherosclerotic lower limb changes in diabetic patients. Our results are in good agreement with recent paper by Nelson et al in which oscillometric ABI was not recommended for routine diagnosis of peripheral arterial disease [18]. Instead palpation of the distal pedal and posterior tibial arterial pulses and testing of limited joint mobility was more sensitive but not as specific as oscillometric blood pressure monitoring.
Some former studies have found the oscillometric method useful as a screening test. Diehm et al (2009) found it useful in oligo-symptomatic non-diabetic patients with PAD but not in diabetic patients alike with our study [8]. Premanath and Raghunath found a sensitivity of 70% and a specificity of 75% using another Omron blood pressure device (HEM-7051-C) with diabetic patients [9]. In our study the sensitivity of the oscillometric method was significantly lower compared to their study. Clairotte et al also studied diabetic patients and concluded that the oscillometric method was useful in detecting PAD when the normal range for the ABI was 1.0 - 1.1 in contrast to the more often used 0.9 - 1.3 as in our study [10].
Kornø et al used a different blood pressure device (CASMED 740) and found that it systematically overestimated the ankle pressure in low blood pressures [11]. They also found the oscillometric method too inaccurate, as 29% of patients would have been incorrectly classified as normal. Aboyans et al and Vinyoles et al also found the oscillometric method unreliable and MacDougall et al underlined that although the oscillometric method was feasible and operator-independent, it could not detect low ABI efficiently [12-14].
Our study suggests that palpating the ADP pulses and testing for LJM is a better method for screening of peripheral artery disease compared to the oscillometric measurement. Its sensitivity was nearly double but it was not as specific as the oscillometric monitor which means that Doppler ultrasound has to be performed on more patients with normal blood flow. Pulse palpation alone is not as sensitive, but more specific and measurement of LJM, although fast if prayers sign is recorded, alone is specific but not at all sensitive. Pulse palpation and LJM together correctly found 20 of the 24 patients (83.3%) with an abnormal ABI, as the oscillometric ankle pressure measurement only found 12 (50%). The ADP pulse might be palpable in high values of ABI and this accounted for three of the 4 false negatives. Pulse palpation and LJM had a quite high rate of false positives (23 patients compared to 7 - 9 by oscillometric monitor). Many of the false positives were cases where the ADP pulse was not palpable because of swelling or previous injuries in the foot.
If the oscillometric measurement of the ABI is added to the screening PAD, the sensitivity is higher (91.6%) than with only pulse palpation and testing for LJM (83.3%). One or more of these tests (pulse palpation, LJM and oscillometric ABI) was abnormal in 50 patients out of 100 patients. 22 of these 50 were true positives, which mean that if the oscillometric measurement of the ABI is added to the screening methods along with pulse palpation and measurement of LJM, 2 more patients with an abnormal ABI measured with the Doppler method, can be found. It also yields 28 false positives and a sensitivity of 63.2%, which is lower than with pulse palpation and LJM (69.7%). If the oscillometric ABI is measured, the Doppler ABI needs to be performed on even more patients with normal blood flow. This adds to the costs as only 2 more patients were found (22/24) compared to pulse palpation and measuring the LJM (20/24).
Our study is limited to the one oscillometric blood pressure device used (Omron M3 Intellisense). The sex distribution of our study was not even (76% male vs. 24% female). In our study Doppler ultrasound is taken as a golden standard, not angiography. However, it would have been unethical to perform angiography to the patients without any sign of peripheral arterial disease. Doppler ultrasound has been earlier compared to angiography and achieved its role as a gold standard [7]. The practical strength of the study was that all measurements were performed by one person and the ordinary oscillometric blood pressure monitor was used, not oscillometric device specifically constructed for ABI measurement. Most general practices cannot afford special devices, but ordinary monitors can be found in every general practice.
7. CONCLUSION
PAD is an underdiagnosed condition, often diagnosed in its later stages when symptoms already occur. PAD is a risk factor for chronic leg and foot ulcerations accounting for 9% - 22% of these cases, 2% - 25% of these patients are diabetics [19]. That is why there is a need for an easy and inexpensive way of screening for PAD in general practice. In our study using an automated and ordinary oscillometric blood pressure device in measuring the ankle pressure was not sensitive enough as a screening method. Therefore we cannot recommend using the Omron M3 Intellisense oscillometric blood pressure device as an only screening method for PAD in diabetic patients. On the other hand ADP pulse palpation and testing for LJM was able to find 83% patients with an abnormal ABI measured by Doppler stethoscope. This economical and handy method is unlikely to miss abnormal ABI, although it has a quite high rate of false positives.
REFERENCES
- Olin, J.W. and Sealove, B.A. (2010) Peripheral artery disease: Current insight into the disease and its diagnosis and management. Mayo Clinic Proceedings, 85, 678-692. http://dx.doi.org/10.4065/mcp.2010.0133
- Willigendael, E.M., Teijink, J.A., Bartelink, M.L., Peters, R.J., Büller, H.R. and Prins, M.H. (2004) Influence of smoking on incidence and prevalence of peripheral arterial disease. Journal of Vascular Surgery, 40, 1158-1165. http://dx.doi.org/10.1016/j.jvs.2004.08.049
- Dormandy, J., Heeck, L. and Vig, S. (1999) Predictors of early disease in the lower limbs. Seminars in Vascular Surgery, 12, 109-117.
- (2010) Finnish Current Care Guidelines: Peripheral arterial disease. Duodecim, 126, 1433-1434.
- Paraskevas, K.I., Kotsikoris, I., Koupidis, S.A., Giannoukas, A.D. and Mikhailidis, D.P. (2010) Ankle-brachial index: A marker of both peripheral arterial disease and systemic atherosclerosis as well as a predictor of vascular events. Angiology, 61, 521-523. http://dx.doi.org/10.1177/0003319710371620
- Zhang, H., Li, X.Y., Si, Y.J., Lu, X.L., Luo, X.S. and Liu, Z.Y. (2010) Manifestation of lower extremity atherosclerosis in diabetic patients with high ankle-brachial index. Chinese Medical Journal, 123, 890-894.
- Lijmer, J.G., Hunink, M.G., van den Dungen, J.J., Loonstra, J. and Smith, A.J. (1996) ROC analysis of noninvasive tests for peripheral arterial disease. Ultrasound in Medicine & Biology, 22, 391-398. http://dx.doi.org/10.1016/0301-5629(96)00036-1
- Diehm, N., Dick, F., Czuprin, C., Lawall, H., Baumgartner, L. and Diehm, C. (2009) Oscillometric measurement of ankle-brachial index in patients with suspected peripheral disease: Comparison with Doppler method. Swiss Medical Weekly, 139, 357-363.
- Premanath, M. and Raghunath, M. (2010) Ankle-Brachial index by oscillometry: A very useful method to assess peripheral arterial disease in diabetes. International Journal of Diabetes in Developing Countries, 30, 97-101. http://dx.doi.org/10.4103/0973-3930.62600
- Clairotte, C., Retout, S., Potier, L., Roussel, R. and Escoubet, B. (2009) Automated ankle-brachial pressure index measurement by clinical staff for peripheral arterial disease diagnosis in nondiabetic and diabetic patients. Diabetes Care, 32, 1231-1236. http://dx.doi.org/10.2337/dc08-2230
- Kornø, M., Eldrup, N. and Sillesen, H. (2009) Comparison of ankle-brachial index measured by an automated oscillometric apparatus with that by standard Doppler technique in vascular patients. European Journal of Vascular and Endovascular Surgery, 3, 610-615. http://dx.doi.org/10.1016/j.ejvs.2009.07.004
- Aboyans, V., Lacroix, P., Doucet, S., Preux, P.M., Criqui, M.H. and Laskar, M. (2008) Diagnosis of peripheral arterial disease in general practice: Can the ankle-brachial index be measured either by pulse palpation or an automatic blood pressure device? International Journal of Clinical Practice, 62, 1001-1007. http://dx.doi.org/10.1111/j.1742-1241.2008.01784.x
- Vinyoles, E., Pujol, E., Casermeiro, J., de Prado, C., Jabalera, S. and Salido, V. (2007) Ankle-brachial index to detect peripheral arterial disease: Concordance and validation study between Doppler and an oscillometric device [Article in Spanish]. Medicina Clínica (Barc), 128, 92-94. http://dx.doi.org/10.1016/S0025-7753(07)72499-5
- MacDougall, A.M., Tandon, V., Wilson, M.P. and Wilson, T.W. (2008) Oscillometric measurement of anklebrachial index. Canadian Journal of Cardiology, 24, 49- 51. http://dx.doi.org/10.1016/S0828-282X(08)70548-8
- Richart, T., Kuznetsova, T., Wizner, B., Struijker-Boudier, H.A. and Staessen, J.A. (2009) Validation of automated oscillometric versus manual measurement of the ankle-brachial index. Hypertension Research, 32, 884- 888. http://dx.doi.org/10.1038/hr.2009.125
- Kawamura, T. (2008) Assessing Ankle-Brachial Index (ABI) by using automated oscillometric devices. Arq Bras Cardiol, 90, 294-298.
- Rosenbloom, A.L., Silverstein, J.H., Legotte, D., Richardson, K. and McCallum, M. (1981) Limited joint mobility in childhood diabetes indicates increased risk for microvascular disease. The New England Journal of Medicine, 305, 191-194. http://dx.doi.org/10.1056/NEJM198107233050403
- Nelson, M., Quinn, S., Winzenberg, T., Howes, F., Shiel, L. and Reid, C.M. (2012) Ankle-Brachial index determination and peripheral arterial disease diagnosis by an oscillometric blood pressure device in primary care: Validation and diagnostic accuracy study. BMJ Open, 2.
- Briggs, M. and Closs, S.J. (2003) The prevalence of leg ulceration: A review of the literature. EWMA Journal, 3, 14-20.
- KEY MESSAGE
- Although oscillometric method is easy and accessible it is not sensitive enough to be recommended as the only method in measuring ABI
- Simple ADP pulse palpation and testing for limited joint mobility (LJM) found 20 of the 24 patients with an abnormal ABI measured by Doppler stethoscope
- This handy and economical approach is unlikely to miss abnormal ABI, although the problem of quite high rate of false positives remains.
NOTES
*Corresponding author.

