World Journal of Cardiovascular Diseases
Vol.2 No.3(2012), Article ID:21230,4 pages DOI:10.4236/wjcd.2012.23025
Successful mitral valve replacement in a young pregnant patient
![]()
1Department of Cardiovascular Surgery, Adana Numune Education and Training Hospital, Adana, Turkey
2Department of Cardiovascular Surgery, Corlu Sifa Hospital, Istanbul, Turkey
3Department of Cardiovascular Surgery, Karadeniz Ereğli Devlet Hastanesi, Karadeniz, Turkey
Email: ofdogan@hacettepe.edu.tr
Received 29 March 2012; revised 30 April 2012; accepted 7 May 2012
Keywords: Pregnancy; Mitral Valve Prosthesis; Thrombosis
ABSTRACT
Pregnancy in women with mechanical prosthetic heart valves is associated with an increased risk of maternal and fetal complications. Managing of the anticoagulation of these patients is very important for life saving of mother and fetus. Unfortunately, thromboembolic complications in some pregnant women with mechanical mitral valve can be seen. Herein, we present urgent mechanical mitral valve replacement in a 27 year old pregnant woman due to stuck mechanical valve.
1. INTRODUCTION
Pregnancy increases the risk of mechanical prosthetic heart valve (MPHV) thrombosis. Warfarin or low molecular weight heparin (LMWH) is protective but implies risks to the fetus. As we know that MPHV have the advantage of longevity but require long-life anticoagulation. Biological or tissue valves do not require anticoagulation, however unlike mechanical heart valves, they wear out over time often necessitating replacement. The risk of valve thrombosis is quoted as being between 0.7% and 6% per patient per year (up to 1.3% for thrombosis). This risk may rise to 25% in the absence of adequate anticoagulation [1]. Herein, we present a young pregnant patient with stuck mitral valve due to valve thrombosis while receiving LMWH and who required re-replacement of mechanical prosthetic mitral valve.
2. CASE REPORT
A 27 year old patient who was 38 weeks pregnant, presented with complaints of dyspnea and palpitations to our emergency unit. Her history revealed that she underwent mitral prosthetic valve replacement (25 no. Bjork-Shiley) for severe mitral valve stenosis. The patient reported that warfarin treatment was stopped with pregnancy, and that she was started on a 20.000 unit dose of low molecular weight heparin twice a daily. The physical examination revealed that the patient was dispneic. The heart rate was 106/min, and blood pressure was 85/50 mmHg; the prosthetic valve click sound was not found. Her transthoracic echocardiography demonstrated an echogenicity consistent with thrombus formation on the left ventricular side and on the mechanical mitral valve (Figure 1). In her Doppler evaluation a pressure difference of a maximum of 15 mmHg, and an average of 10 mmHg, was identified caused by thrombus on the valve which inhibited the valve to open. The patient’s activated partial thromboplastin time (aPTT) was measured as 35.6 sec, whereas the prothrombin time (PTT)- INR valve was measured as 1.32 sec. Fetal and maternal ultrasonography have showed that the normal development of the fetus. The ultrasonographic examination have showed that the the development of the fetus was normal. Thus, we planned urgent caesarean and mitral valve replacement. We offered the choise of heart valve, mechanical and bioprosthesis, to our patient, preoperatively. Because the patient do not decide pregnancy in the future she choised the mechanical mitral valve replacement.
A spinal anaesthesia was performed for the delivery. The fetus was healthy and an Apgar score was normal. 15 min. after, general anaesthesia was induced followed by rapid caesarean section delivery of the baby by the obstetric team.
A median sternotomy incision was performed and mediastinal adhesion was released carefully. Aortic and bicaval cannulation was performed, and cardiopulmonary bypass (CPB) was instituted. The left atriotomy was done. There was a large thrombus formation on the left ventricular side and on the mechanical mitral prosthesis.
The Bjork-Shiley mitral mechanical valve was nearly stuck. Organised and fresh thrombus was carefully
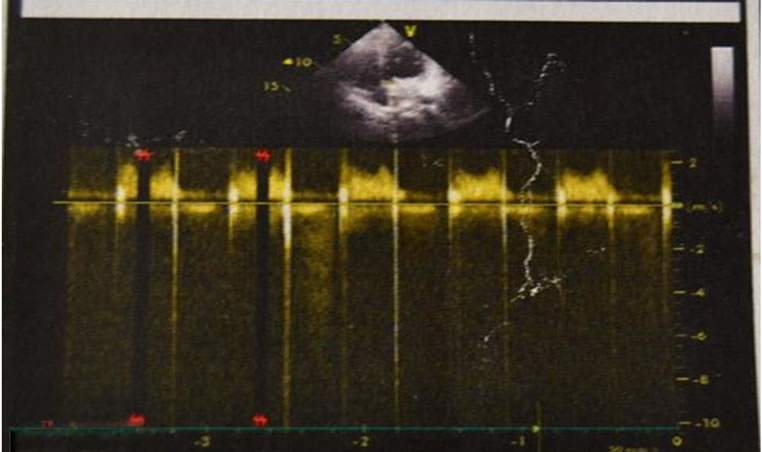
Figure 1. Transthoracic echocardiography demonstrating the echogenicity with thrombus formation on the left ventricular side and on the mechanical mitral valve.
cleared from the prosthetic valve (Figure 2). The BjorkShiley mechanical valve was exised and 25 no. St.Jude mechanical mitral prosthesis was replased using 2/0 teflon pledgetted suture. The patient weaned from CPB without any inotropic support. During the postoperative period LMWH was started twice a daily followed by the initiation of warfarin treatment. The patient was discharged with instructions after the regulation of the INR values above 2.5.
3. DISCUSSION
As we know that pregnancy increases the risk of thrombosis of mechanical prosthetic valve [2,3]. Warfarine, as an oral anticoagulant, is the most effective drug for the prevention of MPHV thrombosis, but the treatment of pregnants using a high dose (over 5 mg daily) warfarine with highest risk to the fetus [4]. Heparine is the most common drug for the prevention of thrombotic complications in pregnants. LMWH reduces the risk of fetal harmfull but it is a less effective anticoagulant even with an adequate range of anti Xa levels. UFH is an effective and safe anticoagulant, but its administration during pregnancy should be considered only during in-hospital stays [4].
Abildgaard et al. have reported an incidence of thromboembolic complications of 7.1% in pregnant women with mechanical heart valve who were anticoagulated with LMWH during the entire pregnancy; 3.6% (0.6% - 13.4%) for LMWH during first trimester and warfarin in the following two, and 2.4% (1.1 - 5.2) for nine months oral anticoagulant [5]. Given the high teratogenic risk of oral anticoagulant and the elevated rate of miscarriages associated to warfarine derivatives in the first trimester of pregnancy, these drugs should be only used in cases at a very high risk of thromboembolic events, leaving LMWH the first option for anticoagulation of MPHV in this period [4,6,7]. During the 2nd and 3rd trimester, oral anticoagulant seem safe for the fetus [4-6].

Figure 2. Shows that the prosthetic mitral mechanical valve after removing from the heart.
In our case, we maintained the patient on LMWH after the operation and changed it to coumadine on the postoperative 2 day. Prior to discharge we stopped the LMWH when the INR was over the 2.5.
The ACC/AHA [8], recommend the use of thrombolysis when surgical risk is high or surgery is not possible. When we research the English literature, there is a limited number of pregnant patients who underwent CPB due to mechanical heart valve thrombosis. Mahli et al. [3] reported a mortality of 1.5% - 5% for the mother and 16% - 33% for the fetus, in pregnant women undergoing cardiac surgery with CPB. Gestational age of <25 weeks was a predictor of fetal mortality. Fetal outcomes are poor, especially at early gestational ages.
When we see the literature the results of fibrinolytic treatment in pregnancy are poorly studied. Leonhardt et al. [9] reported a review of the results of fibrinolysis with recombinant tissue plasminogen activator on 28 pregnant patients. 7 of them with prosthetic thrombosis, with a 7% maternal mortality, 11% therapeutic failure and 24% fetal and peripartum mortality. Besides, fibrinolysis is associated with an elevated mortality (6.1% - 9.3%) and a high incidence of intracranial bleeding (up to 19.8%) [10]. Based on these data, surgery seems preferable over fibrinolysis in the management of left prosthesis thrombosis in pregnancy.
The latest guidelines recommend the use of warfarin up to the 36th week of pregnancy, excluding the period between week 6 and 12, in order to prevent mechanical valve thrombosis.
In our case, mechanical prosthetic valve replacement was performed before pregnancy and there was a regular use of warfarin. However, on the physician’s recommendation warfarin was stopped and low molecular weight heparin was initiated in our patient. Although, there was no valvular thrombosis before pregnancy in our patient, the prosthetic valve led to thrombosis as a result of the propensity of pregnancy for thrombosis and also due to the use of low molecular weight heparin, instead of warfarin.
Similar cases have also been reported in our country. Tuygun et al. [11] successfully performed valve replacement on a patient with mitral valve thrombosis by the 27th week of pregnancy. Ulas et al. [12] in their study also identified valvular thrombosis after administering low molecular weight heparin in a 3.5 month pregnant woman, and successfully performed a valve replacement. Koçak et al. was performed elective valve replacement on the 8th day following delivery in a 35-week pregnant woman who visited due to mitral valve thrombosis [13]. Inanc et al. have previously reported two pregnant cases who have been treated successfully [14]. One of them have treated medically and the other one treated surgically.
The guidelines recommend the evaluation of anti-Xa when administering low molecular weight heparin to a pregnant woman [6]. In our case the level of aPTT was not evaluated regularly. As we know that these two types of heparin do not lead to fetal hemorrhage and teratogenicity because they do not cross the placenta. As a result both heparins can be considered to be safer than warfarin. However, pregnant women using unfractionated heparin or low molecular weight heparin have been found to have a 12% - 24% higher risk of developing thromboembolic complications such as valvular thrombosis, when compared to warfarin.
The choice of the type of prosthetic valve in women of child bearing age has always been controversial. Although bioprosthetic valves do not need anticoagulation, they are prone to rapid degeneration during the early stage. Pregnancy accelerates this process and a second surgical operation is necessary due to damage to the valve at an early stage. On the other hand, mechanical valves are preferred due to their durability. However, because of the need for anticoagulation, they may threaten the current pregnancy and future anticipated pregnancies.
In conclusion, in the late stage of pregnancy the patients with thrombotic heart valve can be operated safely after urgent caeserian delivery. We believe that these limited cases will be given encourage to the cardiac surgeons about the management of pregnants who need surgery. Female patients with mechanical prosthetic valves who are planning pregnancy should be informed about thromboembolic complications associated with anticoagulation therapy changes, and they should discuss and decide with their physician before choosing the anticoagulation therapy to be used during pregnancy.
REFERENCES
- Roudaut, R., Serri, K. and Lafitte, S. (2007) Thrombosis of prosthetic heart valves: Diagnosis and therapeutic considerations. Heart, 93, 137-142. doi:10.1136/hrt.2005.071183
- Clark, P., Brennand, J., Conkie, J.A., McCall, F., Greer, I.A. and Walker, I.D. (1998) Activated protein C sensivity, protein C, protein S and coagulation in normal pregnancy. Thrombosis and Haemostasis, 79, 1166-1170.
- Mahli, A., Izdes, S. and Coskun, D. (2000) Cardiac operations during pregnancy: Review of factors influencing fetal outcome. The Annals of Thoracic Surgery, 69, 1622-1626. doi:10.1016/S0003-4975(00)01178-4
- Chan, W.S., Anand, S. and Ginsberg, J.S. (2000) Anticoagulation of pregnant women with mechanical heart valves: As systematic review of the literature. Archives of Internal Medicine, 160, 191-196. doi:10.1001/archinte.160.2.191
- Abildgaard, U., Sanset, P.M., Hammerstrom, J., Gjestvang, F.T. and Tveit, A. (2009) Management of pregnant women with mechanical heart valve prosthesis: Thromboprophylaxix with low molecular weight heparin. Thrombosis Research, 124, 262-267. doi:10.1016/j.thromres.2008.12.005
- Bates, S.M., Greer, I.A., Pabinger, I., Sofaer, S. and Hirsh, J. (2008) Venous thromboembolism. Thrombophilia, antithrombotic therapy, and pregnancy: American College of Chest Physicians Evidence Based Clinical Practice Guidelines, 8th edition. Chest, 133, 844-886.
- Alcázar, M.C., Lacruz, F.R., Villalobos, L.M. and Hernández, J.E.R. (2010) Mechanical prosthetic mitral valve thrombosis in a first trimester pregnant woman. Interactive CardioVascular and Thoracic Surgery, 10, 116- 118. doi:10.1510/icvts.2009.220806
- American College of Cardiology/American Heart Association Task Force on Practice Guidelines, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Thoracic Surgeons, Bonow, R.O., et al. (2006) ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (writing committee to revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): Developed in collaboration with the Society of Cardiovascular Anesthesiologists: Endorsed by the Society for Cardiovascular Angiography and Interventions and the Society of Thoracic Surgeons. Circulation, 114, e84-e231.
- Leonhardt, G., Gaul, C., Nietsc, H.H., Buerke, M. and Scleussner, E. (2006) Thrombolytic therapy in pregnancy. Journal of Thrombosis and Thrombolysis, 21, 271-276. doi:10.1007/s11239-006-5709-z
- The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group (1995) Tissue plasminogen activator for acute ischemic stroke. The New England Journal of Medicine, 333, 1581-1587. doi:10.1056/NEJM199512143332401
- Tuygun, A.K., Olsun, A., Yurtseven, N., et al. (2004) Gebelik ve açık kalp cerrahisi: İki ucu keskin kılıç. Turkish Journal of Thoracic and Cardiovascular Surgery, 12, 262- 264.
- Ulaş, M.M., Çağlı, K., Çetin, E., Boysan, E., Mavioğlu, L. and Sarıtaş, A. (2005) Mitral kapak replasmanı sonrası ikinci gebeliği esnasında tromboza bağlı mekanik kapak disfonksiyonu nedeniyle opere edilen bir hasta. Anatolian Journal of Cardiology, 5, 240-241.
- Koçak, T., Güzelmeriç, F., Oğuş, H., Orki, T. and Erkılıç, A. (2006) Mitral protez kapak disfonksiyonu ve pulmoner hipertansiyonu olan gebede acil sezaryen operasyonunda anestezik yaklaşım (olgu sunumu). Turkish Journal of Anesthesia, 14, 269-272.
- Inanç, M.T., Doğdu, O., Kaya, M.G. and Doğan, A. (2009) Prosthetic mechanic valve thrombosis in pregnant women: A report of two cases. Turk Kardiyoloji Dernegi Arsivi, 37, 57-60.

