Health
Vol.5 No.8C(2013), Article ID:35792,7 pages DOI:10.4236/health.2013.58A3007
Evaluation of functional capacity, body composicion and pulmonary function after bariatric surgery*
![]()
1Uninove—Nove de Julho University, São Paulo, Brazil; #Corresponding Authors: marcelacbarbalho@hotmail.com, dcosta@uninove.br
2UFSCar—Federal University of São Carlos, São Carlos, Brazil
Copyright © 2013 Flávia Sales Leite et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received 19 May 2013; revised 19 June 2013; accepted 20 July 2013
Keywords: Obesity; Bariatric Surgery; Exercise; Spirometry; Muscle Strength
ABSTRACT
Introduction: Obesity has been considered a global epidemic and a serious public health problem closely related to other diseases. Moreover, obese individuals have limitations in physical capacity and pulmonary function. Weight loss induced by bariatric surgery appears to help reverse this situation. However, questions about physical capacity and lung function, and its relationship with body composition remain to be clarified. Objective: To evaluate the physical capacity, body composition and lung function in women undergoing bariatric surgery. Methods: Twenty five women who underwent bariatric surgery between 6 and 24 months ago, and 10 non-obese women were evaluated for exercise capacity by the six minutes walk test (6 MWT), body composition by bio-electrical impedance analysis and lung function by spirometry and measurement of maximal static respiratory pressures. Results: Subjects with BMI wang#Bracket##30 kg/m2 were found to have better physical performance, demonstrated by increased 6 MWT distance, not differing from non-obese women. When compared with non-obese women, there were no significant differences in body composition and lung function. Higher BMI was correlated with shorter distances in 6 MWT. Conclusion: 6 to 24 months after surgery, when the weight loss of patients who underwent bariatric surgery reaches levels considered non-obese, it provides improvement in physical performance to a level similar to that of non-obese patients.
1. INTRODUCTION
According to the World Health Organization (WHO), in 2008, over 200 million men and approximately 300 million women were obese [1]. This number is double the value recorded in 1980 [1]. Thus, obesity has been considered a world epidemic and serious public health problem, since it is associated with other various diseases, such as: diabetes mellitus, systemic arterial hypertension, dyslipidemia, obstructive sleep apnea and others [2, 3].
Obesity is also associated with compromised lung function, such as: reduction in pulmonary volumes, reduction in strength and endurance of respiratory muscles, increase in respiratory work, and reduction in mobility of the diaphragm muscle and hypoxemia [4-6]. These alterations are caused by compromise of the ventilatory mechanics observed in obese individuals, which are proportionally worse as the body mass index (BMI) increases, and in situations which the body fat distribution is located mainly in the abdominal cavity (central obesity) [4-6]. In addition, there are factors of inflammatory and metabolic origin related to obesity, which also negatively influence lung function [4].
In addition to compromising lung function, some studies have demonstrated that obesity is also related to a reduction in physical exercise capacity and oxygen consumption (VO2) [7], and this reduction gradually becomes accentuated with the increase in BMI [8,9]. This poor aerobic conditioning observed in the obese may be due to both the harmed cardiovascular function [10] and the low oxidative capacity of the skeletal muscle [11,12]. The six minute walk test (6MWT) has been used to evaluate the functional capacity of these patients, since it can be performed by severely limited individuals, and those who do not tolerate other functional capacity evaluation tests [13].
Within this context, bariatric surgery has been considered the treatment of choice in cases of morbid obesity, as it results in a significant and sustainable weight loss, in addition to great improvement in associated diseases [2]. Therefore, in spite of recent studies having demonstrated positive post-bariatric surgery weight loss results in the pulmonary and cardiovascular systems [13-15], there is still a gap in the information about the physical and functional respiratory performance of subjects undergoing to bariatric surgery, and the relationship with body composition, particularly, in the medium and long post-operative term, thus justifying the research for further information.
Based on these data, the aim of this study was to compare the physical capacity, body composition and respiratory functional capacity of women submitted to bariatric surgery, with those non-obese, sedentary women.
2. METHODS
2.1. Type of Study
This study, characterized as a cross-sectional type, conducted in the Laboratory of Reparatory Functional Evaluation (LARESP) at Nove de Julho University (UNINOVE), was submitted to and approved by the Research Ethics Committee (CEP) of the institution, under Protocol No.410518.
2.2. Sample
The sample size calculation was made, considering the main variable to be the six minute walk test distance (6 MWTD). Therefore, the sample calculation was applied considering a power of 80% with an alpha error of 0.05 (20%) and the sample suggested was 10 volunteers for each group.
Patients undergoing to bariatric surgery, whose data belonged to the database of the Mandaqui Hospital Complex and the Irmandade da Santa Casa de Misericórdia de São Paulo were evaluated. Contact was made by telephone, with 113 women who met the inclusion criteria, as follows: they had to have been submitted to bariatric a minimum of 6 months and maximum of 24 months ago; they had to be apt to undergo the proposed physical and functional respiratory test, and be older than 18 years of age. Of these 113 volunteers, 48 accepted participating in the study; however, 22 of them dropped and 1 (one) was unable to perform all the tests because she was physically unable to do so, and was therefore excluded. Thus, the Bariatric Group (BG) was composed of 25 patients. At the time of evaluation, as some of the BG patients were still obese (BMI ≥ 30 kg/m2) even after the surgery, for analysis of the results, this group was divided into two other groups, one being denominated Obese Bariatric Group (OBG) and the other Non Obese Bariatric Group (BMI < 30 kg/m2) (NOBG), as illustrated in the experimental design in Figure 1.
To compose the Control Group (CG), 10 healthy sedentary women, in the same age group as those of BG, with a BMI of 18.5 kg/m2 to 24.9 kg/m2 were recruited. The data of sample characteristics are shown in Table 1.
2.3. Experimental Procedure
All the procedures were previously explained to the patients, and took place at LARESP on the same day, according to the sequence described as follows.
Initially an interview was held, with the collection of data that included personal data, clinical history, associated diseases, and personal antecedents. After this the patients were weighed on an Electric Bioimpedance scale, submitted to Spirometry, respiratory muscle strength test
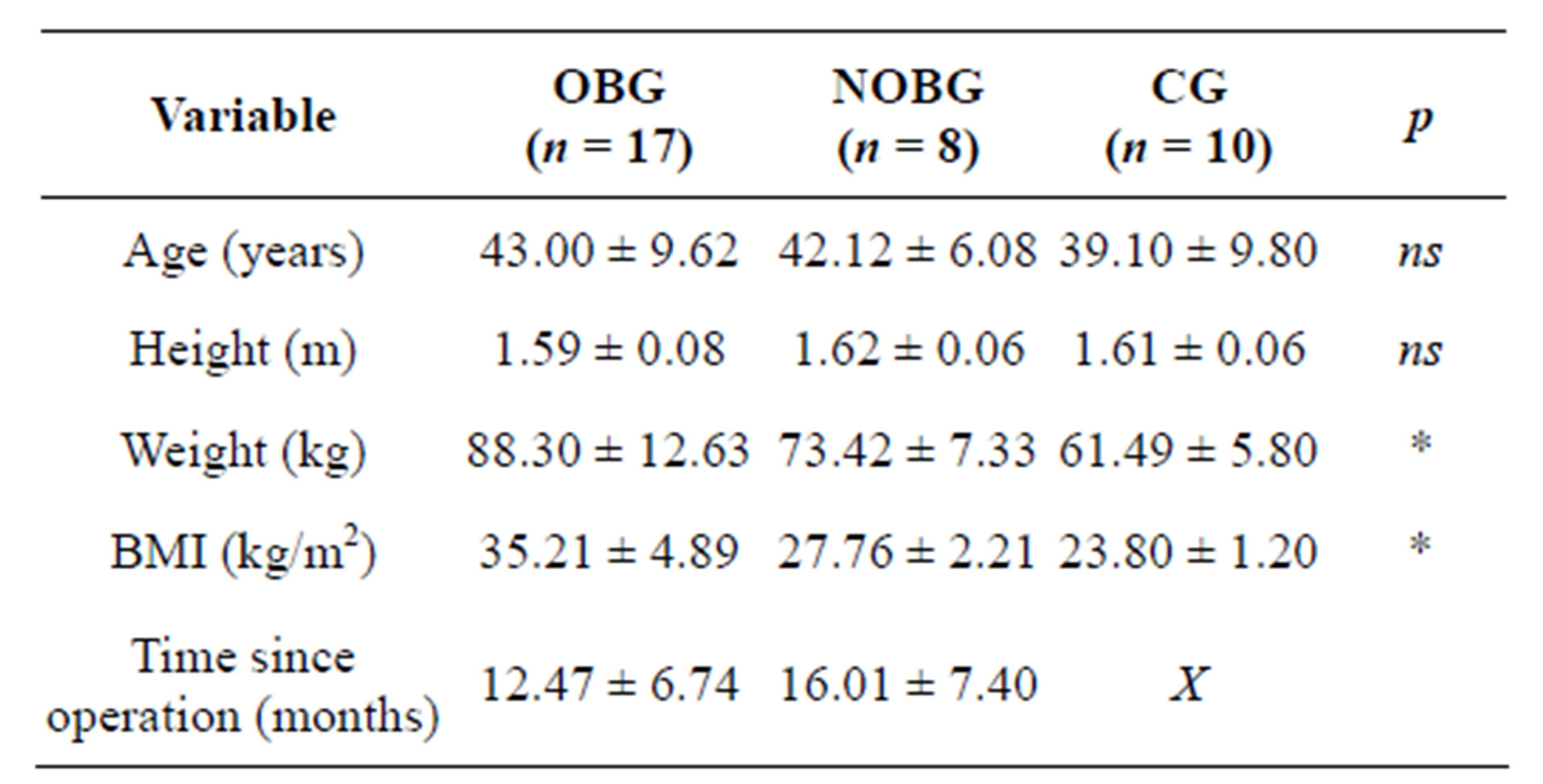
Table 1. General data of sample.
BMI: Body mass index; nsDifference not significant; *p ≤ 0.05. The data are presented as absolute values and standard deviations (SD).
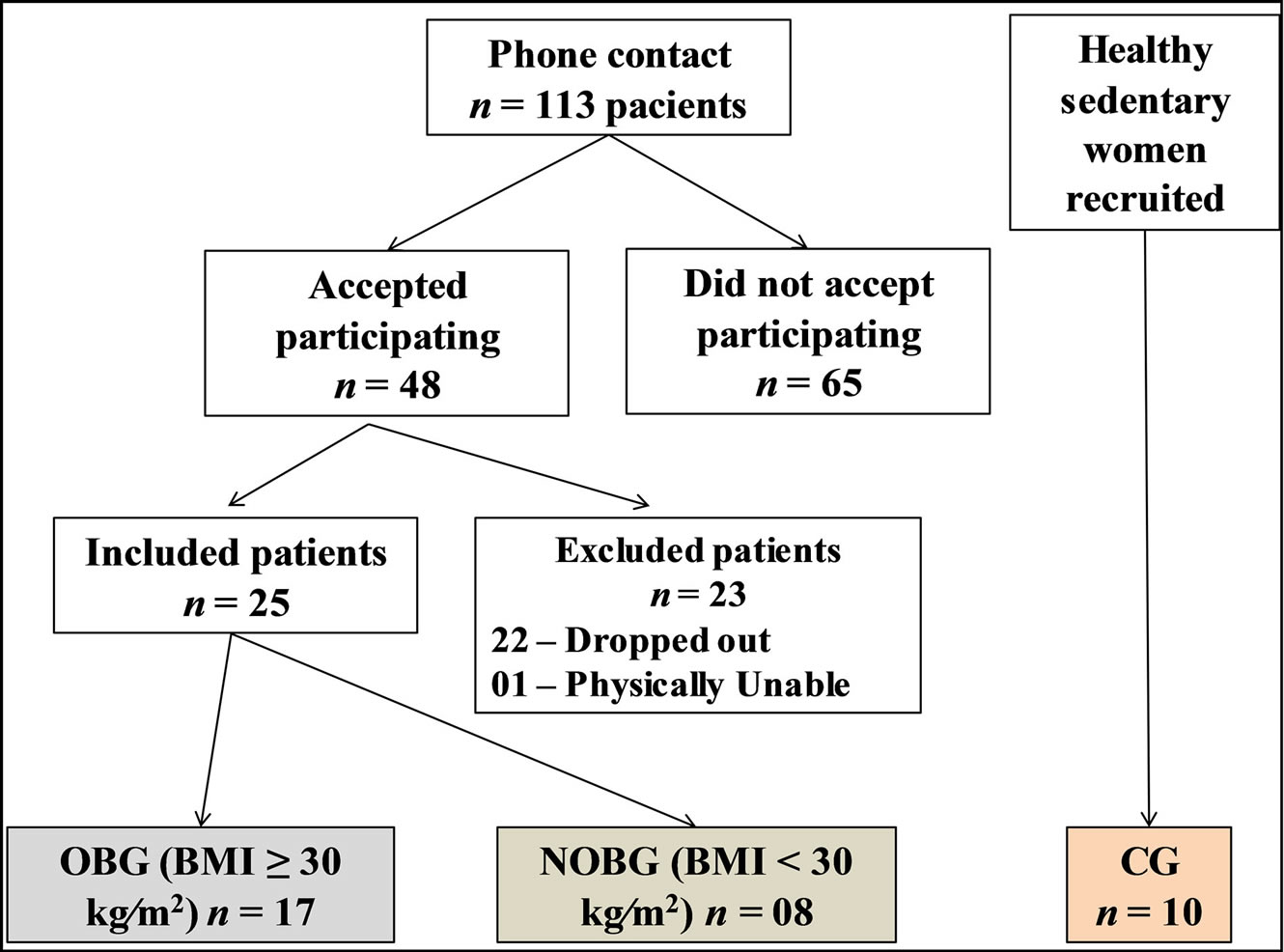
Figure 1. Flow diagram of sample selection. OBG: obese group, NOBG: non obese group, CG: control group.
(manovacuometry) and then to the six minute walk test (6MWT).
Evalutation Tests
Six Minute Walk Test (6MWT)—This test, with the aim of evaluating functional capacity, was performed by a trained evaluator, in a corridor 30 meters long, in which the patient was instructed to walk for six minutes. The following measures were evaluated: Heart rate (HR), peripheral pulse oxymetry (SpO2), arterial body pressure (BP), respiratory rate (RR) and the Borg scale for dyspnea and lower limb tiredness at the beginning and end of each test. During the entire test, the patient was monitored by means of an oxymeter, with HR and SpO2.
Electric Bioimpedance—The patients were weighed barefooted, on an electric bioimpedance scale (BC 554— Tanita Iron Man®), with their feet having been previously cleaned with a 70% alcohool solution. This same opportunity was taken to measure their height, using a wall stadiometer for this purpose. The BMI was calculated by dividing the body weight (kg) by the height in square meters (m2).
All the data with reference to the follow were collected: body fat, total water, muscle mass and bone mass.
Other authors have shown [16,17] that the Electric Bioimpedance, used in this study to evaluate the physical constitution of the volunteers had a good correlation with Dual X-ray absorptiometry (DEXA), which is the technique considered the gold standard for measures of physical constitution.
Spirometry—For spirometry, an Easy on-PC VA 1.0.0.7 Spirometer of the NDD Medizintechnik AG® Brand (Zurich, Switzerland) was used. The tests were performed by the same evaluator and the patients used a nose clip, and remained seated. A minimum of three acceptable and reproducible curves, and a maximum of eight measures were collected, and the highest values were computed. All the procedures were performed in accordance with the guidelines of the American Thoracic Society (ATS) and European Respiratory Society (ERS) [18] in a duly climatized room with controlled temperature and barometric pressure.
The maneuvers of Slow Vital Capacity (SVC), Forced Vital Capacity (FVC) and Maximum Voluntary Ventilation (MVV) were performed.
Respiratory Muscle Strength (RMS)—To measure the RMS an analogical manovacuometer of the Ger-Ar® brand was used, scaled in cmH2O, with an operating limit from 0 to ±300 cm H2O. The volunteers were in a seated position, and to obtain the maximum inspiratory pressure (MIP) they were asked to perform maximum expiration, up to the level of residual volume (VR), followed by maximum inspiration sustained for a minimum of 1 second. To obtain the maximum expiratory pressure (MEP) they were asked to perform a maximum inspiration up to the level of total lung capacity (TLC) and after this to perform a maximum expiration, also sustained for a minimum of 1 second. Both maneuvers were performed a minimum of three times, and a maximum of 5 times, so that the highest value was recorded, provided it did not differ more than 10% from the immediately lower value. In addition to the values obtained, the respective values foreseen for each volunteer were also calculated according to the reference equations for healthy individuals, proposed by Costa, et al. [19].
Data Treatment and Analysis—The software program GraphPad Instat was used. The data are presented in tables as absolute values and standard deviations (SD). The Kolmogorov-Smirnov adherence test was used. For the comparison of variables in the 3 groups (OBG, NOBG and CG) the (one way) ANOVA and Bonferroni post-hoc tests were used. For correlation between the variables in the 6MWTD and BMI, Pearson’s correlation was used.
3. RESULTS
Of the patients undergoing to bariatric surgery, 80% lost a minimum of 50% of their excess body weight (EBW); of whom 60% lost from 50% to 74% of EBW, and 20% lost from 75% to 100% of EBW. No patient gained weight or lost less than 25% of EBW. To compute the percentage of EBW (%EBW) the following calculation was used: from the initial weight (before surgery) the present weight was subtracted, thus the weight loss was obtained. Once again, from the initial weight, the ideal weight was subtracted, in accordance with a standardized table, and thus, the excess weight was obtained. The value of 100% was attributed to the excess weight, so that the value of weight loss is the percentage that was sought.
Six minute walk test (6MWT)—This test, with the object of evaluating physical capacity, was explored by the absolute values of the distance covered, percentages of the value obtained in relation to the predicted values [20]; in addition to the estimated values of VO2 [21]. The patients of the OBG walked significantly less than the volunteers in CG and NOBG, however, without statistical difference between the latter two. In the tests between the groups, significant difference was also found between the estimated values of VO2. The VO2 attained in 6MWT by the OBG was significantly lower in comparison with the values attained by CG and NOBG, however, without statistical difference for the latter (Table 2). The distance walked in 6MWT (6MWTD) presented a negative correlation with the BMI (r = −0.59; p < 0.01), as illustrated in Figure 2.
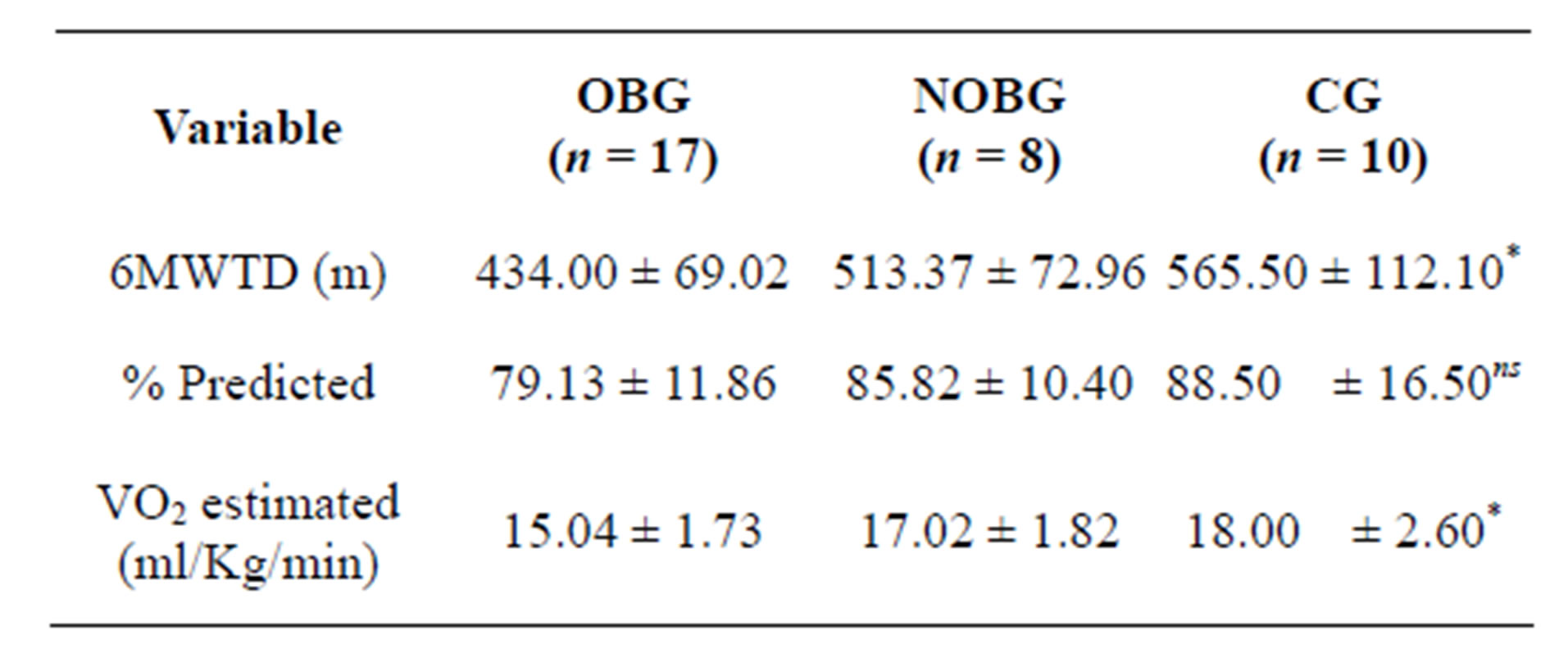
Table 2. Results of six minute walk test (6MWT).
OBG Obese bariatric group; NOBG: Non obese bariatric group; CG: Control Group; *p < 0.05 for OBG vs CG; nsnot significant. The data are presented as absolute values and standard deviations (SD).
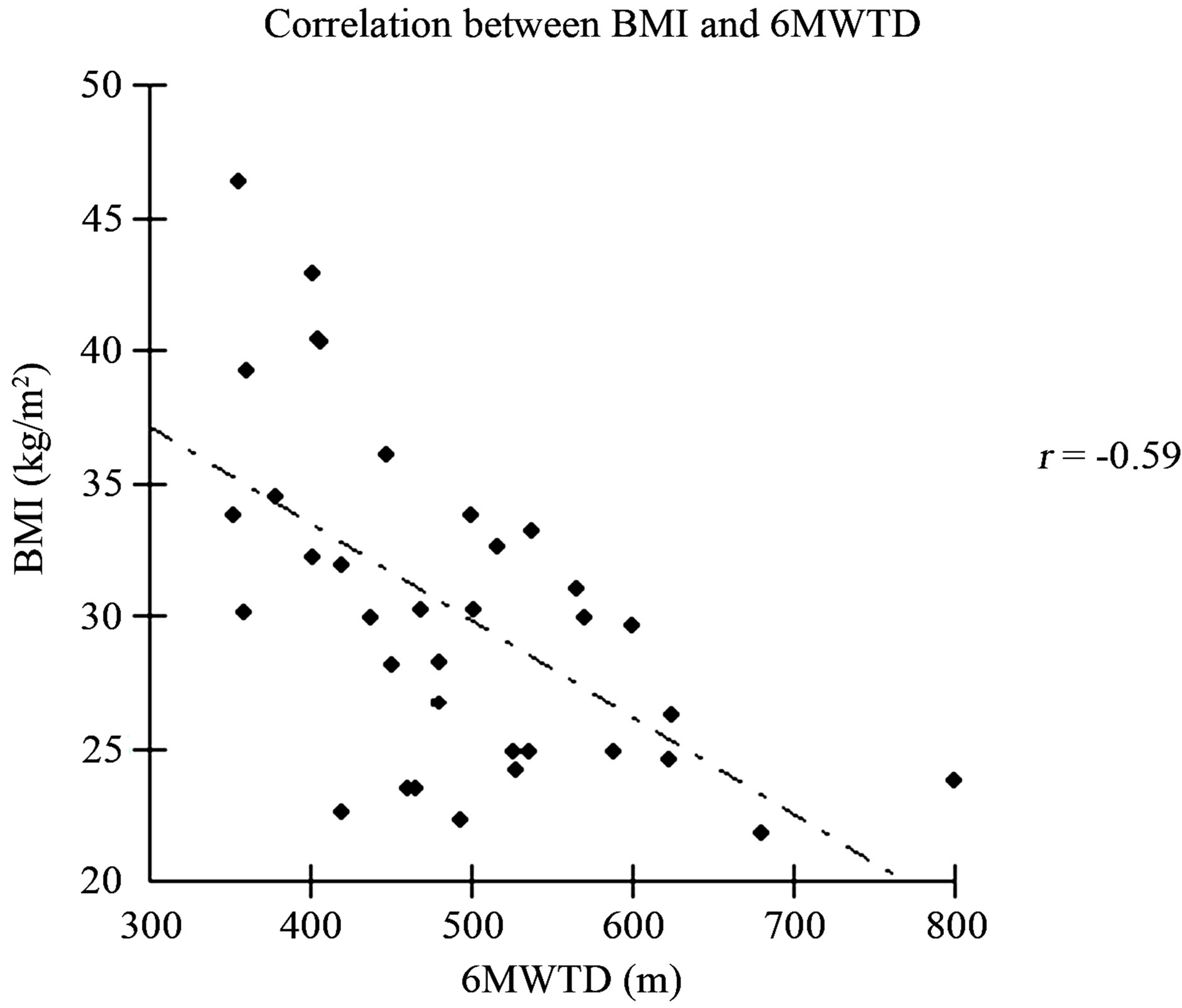
Figure 2. Graph of correlation between six minute walk test distance (6MWTD) and body mass index (BMI).
Electric Bioimpedance—The physical constitution was evaluated by Electric Bioimpedance, by means of the following variables: % body fat; % of total water; % of muscle mass, and % of bone mass. It was found that there was significant difference between all the variables that composed the body composition among the patients of Groups OBG and CG; and OBG and NOBG. There was no statistically significant difference between NOBG and CG, and the patients in these groups presented a lower percentage of fat, and higher percentage of muscle mass, total water and bone mass than the OBG (Table 3).
Spirometry—The spirometric variables are presented in absolute values and percentages of those obtained in relation to the predicted values [22]. There was no statistically significant difference between the groups for the spirometric variables evaluated (Table 4).
Respiratory Muscle Strength (RMS)—The RMS values are presented in Table 5 in absolute and percentage values of those obtained in relation to the predicted values [19]. Although there was a trend towards the mean MIP and MEP values being lower in OBG, this was not statistically significant.
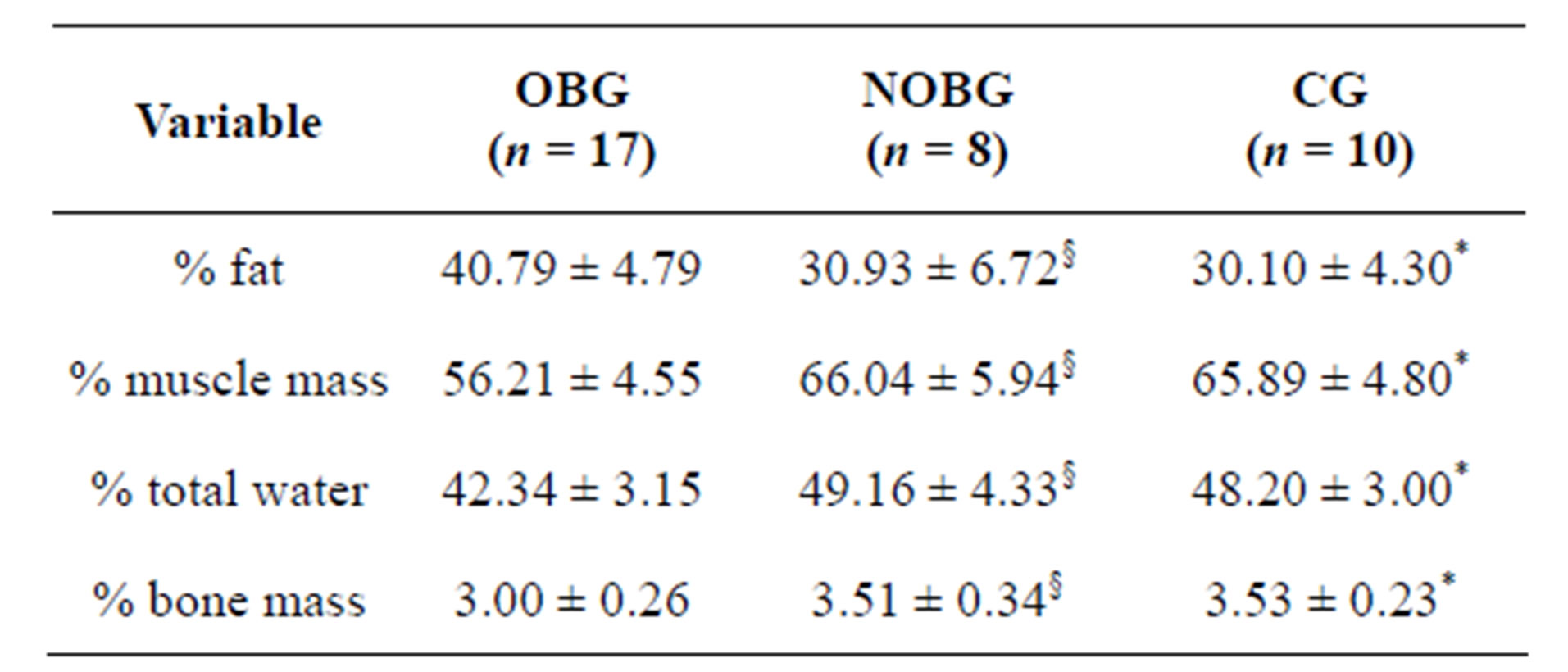
Table 3. Results of electric bioimpedance test.
OBG: Obese bariatric group; NOBG: Non obese bariatric group; CG: Control Group; §p < 0.05 for OBG vs NOBG; *p < 0.05 for OBG vs CG. There was no statistical difference between NOBG and CG. The data are presented as absolute values and standard deviations (SD).
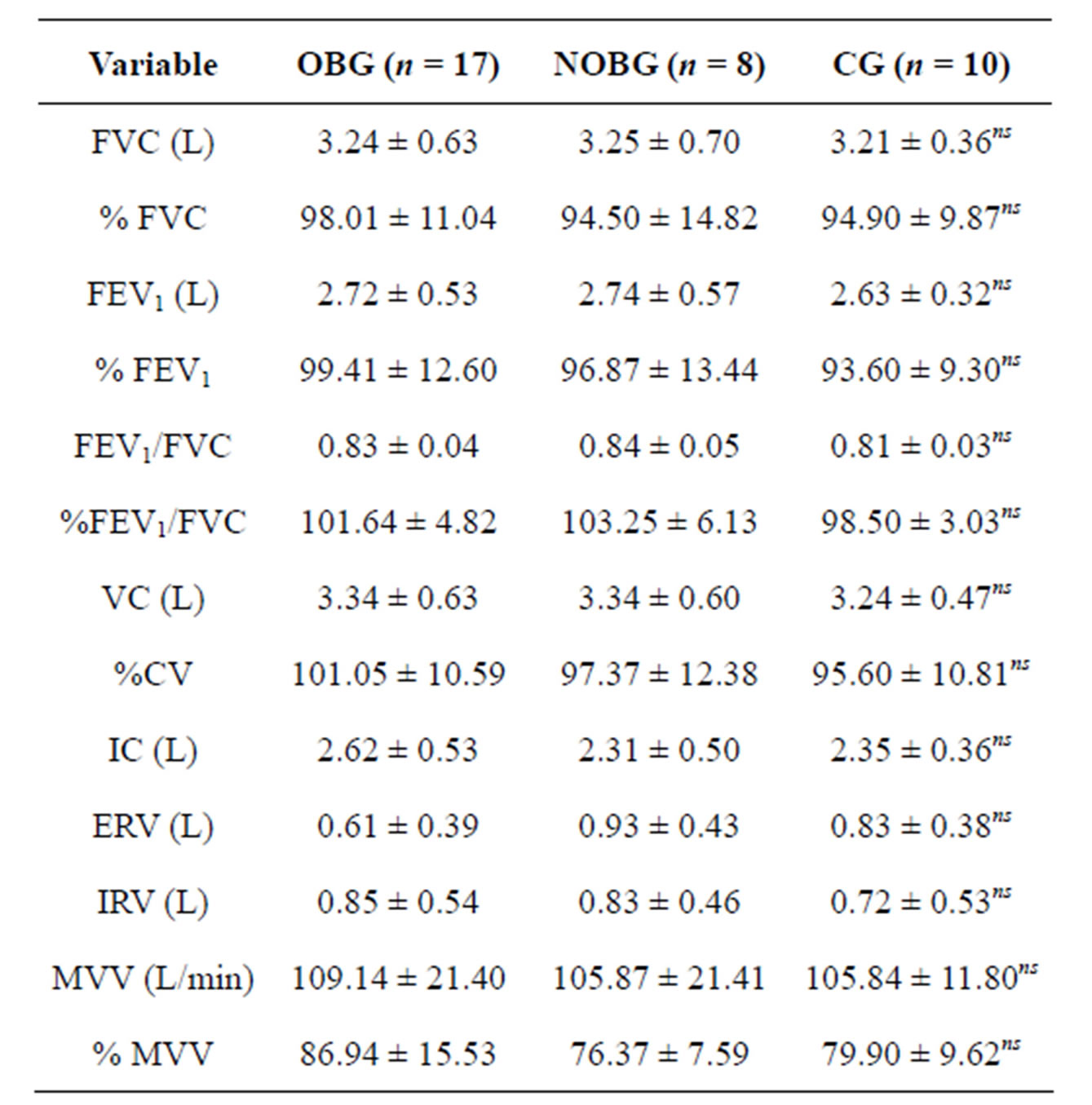
Table 4. Spirometry results.
OBG: Obese bariatric group; NOBG: Non obese bariatric group; CG: Control Group; FVC: Forced vital capacity; FEV1: Forced expiratory volume in one second; VC: Vital capacity; IC: Inspiratory capacity; ERV: Expiratory reserve volume; IRV: Inspiratory reserve volume; MVV: Maximum voluntary ventilation. nsnot significant. The data are presented as absolute values and standard deviations (SD).
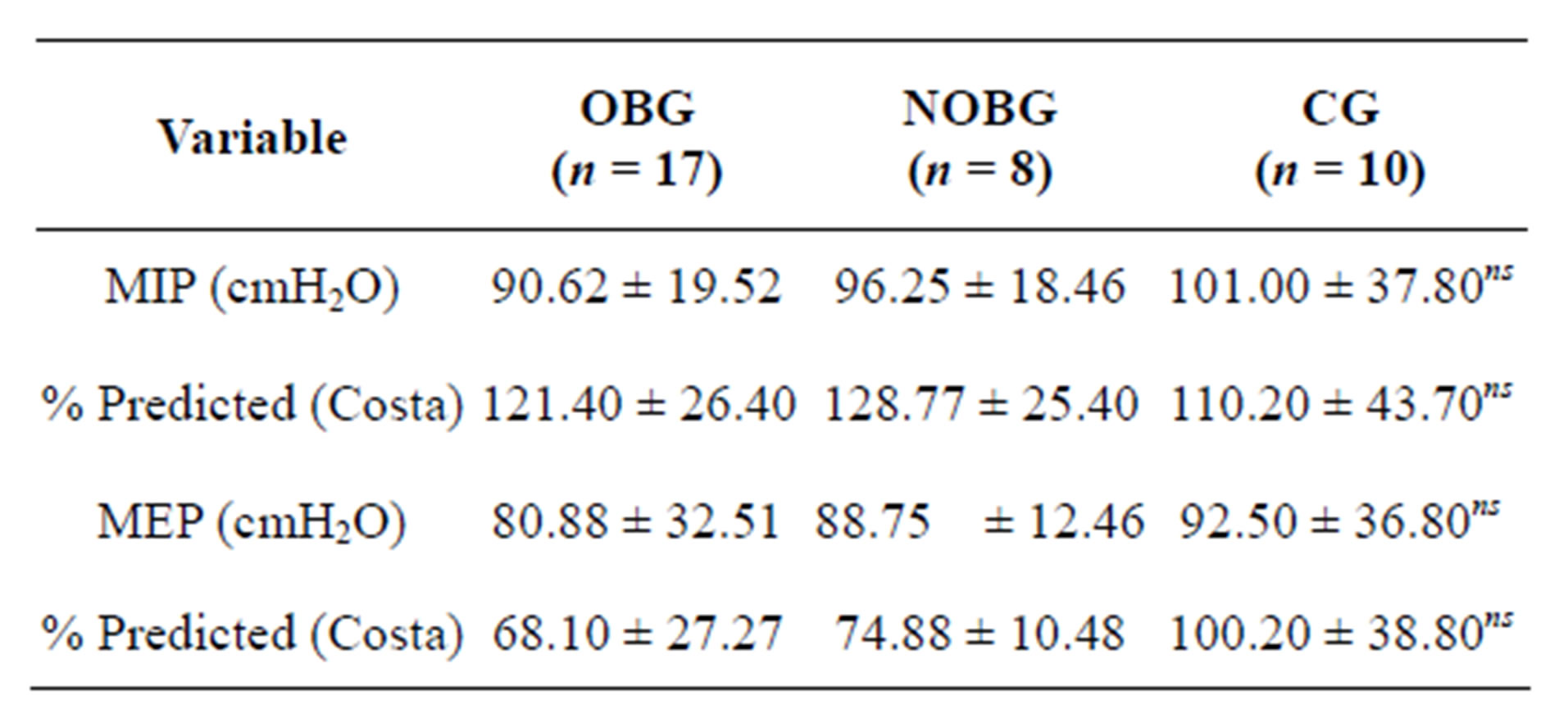
Table 5. Results of respiratory muscle strength (MIP and MEP).
OBG Obese bariatric group; NOBG: Non obese bariatric group; CG: Control Group; MIP: Maximum inspiratory pressure; MEP: Maximum expiratory pressure; nsnot significant. The data are presented as absolute values and standard deviations (SD).
4. DISCUSSION
According to the results presented, it was possible to verify that patients undergoing to bariatric surgery, but with a normal BMI, had a body composition and functional capacity similar to those of volunteers in the Control Group (non obese). On the other hand, patients submitted to bariatric surgery, but who still continued to be obese, walked less than the others, and therefore there is greater compromise of functional capacity, associated with a higher percentage of body fat and lower percentage of muscle mass. Moreover, 80% of the patients submitted to bariatric surgery lost a minimum of 50% of excess body weight after the period from 6 to 24 months after surgery, which is in agreement with findings in the literature [23,24].
The improvement in functional capacity after a great weight loss induced by bariatric surgery, has also been related by means of the increase in distance walked in 6 MWT and by the longer time of duration of exercise in the cardiopulmonary test [13,25,26]. A reminder, however, that not all the obese subjects find it easy to perform a cardiopulmonary test, but all found it easy to perform a 6MWT. Furthermore, as has been demonstrated by Maniscalco, et al. [26], we could find a longer 6 MWTD, associated with a lower BMI value, confirming that patients with a lower BMI walked longer distances. This increase in the 6MWTD appears to be mainly due to the improvement in respiratory mechanics, and conesquently, greater ease in breathing during physical efforts, such as walking, in which, after weight reduction, there is also a reduction in work and energy spent to move the body during performance of the test, and improvement in cardiovascular function [25,27]. Nevertheless, it must be considered that in spite of the increase in 6MWTD after large weight losses, this does not represent an improvement in aerobic capacity. Stegen, et al. [27], have suggested that the implementation of a physical exercise program is necessary to achieve more effective benefits in the physical and functional performance of these subjects.
In spite of the 6MWT not offering sufficient information to determine the main causes in limitation on physical exercise [20], this test has important advantages, mainly because it is simple, low cost, and because it is a sub-maximum test, very similar to the effort made during daily life activities, and can be easily be performed by obese individual, especially by those who do not tolerate maximum efforts [13].
Another factor that may influence the 6MWTD is the percentage of lean mass. Some studies have demonstrated that patients submitted to bariatric surgery lose weight, both by means of the reduction in fat mass and in lean mass [27,28]. Nevertheless, one has to consider that the loss of muscle mass may, alone, be a component that is harmful to physical performance, because contrary to this, our patients who presented a higher percentage of muscle mass were able to cover longer distances in TC6. According to Aquino, et al. [28], the hypocaloric diet frequently prescribed in the post-operative period drives proteolysis to meet the metabolic demands, and this fact would explain the reduction in lean mass. Herein lies the importance of establishing a strict nutritional follow-up and programs of physical activities for post-bariatric surgery patients. These authors [28] suggest that diets with emphasis on protein consumption, associated with physical activity after bariatric surgery could be effective strategies for minimizing the loss of lean mass.
As regards the spirometric results, in addition to not finding any type of ventilatory disturbance, either of an obstructive or restrictive nature, no difference were verified in the spirometric variables between the different groups either, in spite of the difference in BMI among them, which is in agreement with the results of Domingos-Benício, et al. [29], in which no significant difference was also observed in the FVC and FEV1 between obese and non obese subjects. Nevertheless, controversies persist in the literature about respiratory volumes and capacities in obese subjects, because there is information that lower BMI values are related to higher spirometric values, when comparing obese and non obese or preand post-bariatric surgery subjects [15].
In a similar manner to that which occurs with pulmonary function, observed by spirometry, respiratory muscle strength has also presented controversies in the data in the literature, because, while Dávila-Cervantes, et al. [15] found increases in MIP and MEP after weight loss induced by bariatric surgery, Wadstrom, et al. [30] found a reduction in respiratory muscle strength after bariatric surgery. Associated with this, Stegen, et al. [27] also found a reduction in peripheral muscle strength in obese subjects after bariatric surgery. This reduction has been attributed to the reduction in lean mass due to weight loss [27]. In the present study, although no significant differences in respiratory muscle strength were found between the different groups studied, it was shown that the absolute values of PImax and PEmax obtained in the obese patients were overestimated in the former and underestimated in the latter, according to the predicted values for non obese subjects [19], in the same age range. This fact justifies the need for seeking equation of predicted values specifically for this population of obese individuals.
Attention is drawn to a limitation of this study, the fact that the patients were not evaluated before bariatric surgery, in order to obtain data with respect to the evolution and progression, or not, of pulmonary function and functional capacity, and of respiratory muscle strength.
5. CONCLUSION
Based on the results observed in this study, it could be concluded that the obese patients submitted to bariatric surgery, with normal BMI, have functional capacity and body composition similar to that of non obese subjects, while those who continue to be obese, have greater compromise of their functional capacity associated with a higher percentage of body fat and lower percentage of lean mass. Furthermore, it was concluded that the longer distance covered in the walk test was related to the lower BMI value.
6. ACKNOWLEDGEMENTS
The authors thank all the volunteers who participated in this study, and are grateful for the support received by means of CNPq Process No: 504228/2010-2, CNPq Process No.: N 579981/2008-8, and CAPES AUX PE PNPD Process No.: 2562/2011.
REFERENCES
- World Health Organization (WHO). (2011) Obesity and Overweight. WHO Fact Sheet N˚311, March 2011. www.who.int
- World Health Organization (WHO). (2000) Obesity: Preventing and managing the global epidemic. Report of a WHO Consultation, World Health Organization technical report series, 894, 1-253.
- National Task Force on Prevention and Treatment of Obesity. (2000) Overweight, obesity and health risk. Archives of Internal Medicine, 160, 898-904. doi:10.1001/archinte.160.7.898
- Zammit, C., Liddicoat, H., Moonsie, I. and Makker, H. (2010) Obesity and respiratory diseases. International Journal of General Medicine, 3, 335-343. doi:10.1186/1465-9921-9-31
- Thyagarajan, B., Jacobs, Jr. D.R., Apostol, G.G., Smith, L.J., Jensen, R.L., Crapo, R.O., Barr, R.G., Lewis, C.E. and Williams, O.D. (2008) Longitudinal association of body mass index with lung function: The CARDIA Study. Respiratory Research, 9, 31.
- Costa, D., Barbalho, M.C., Miguel, G.P.S., Forti, E.M.P. and Azevedo, J.L.M.C. (2008) The impact of obesity on pulmonary function in adult women. Clinics, 63, 719- 724. doi:10.1590/S1807-59322008000600002
- Salvadori, A., Fanari, P., Fontana, M., et al. (1999) Oxygen uptake and cardiac performance in obese and normal subjects during exercise. Respiration, 66, 25-33. doi:10.1159/000029333
- Gallagher, M.J., Franklin, B.A., deJong, A., et al. (2004) Cardiorespiratory fitness levels in obesity approximate those of heart failure patients: Implications for exercise prescription. Circulation, 110, 822A.
- McCullough, P.A., Gallagher, M.J., deJong, A.T., Sandberg, K.R., Trivax, J.E., Alexander, D., Kasturi, G., Jafri, S.M.A., Krause, K.R., Chengelis, D.L., Moy, J. and Franklin, B.A. (2006) Cardiorespiratory fitness and shortterm complications after bariatric surgery. Chest, 130, 517-525. doi:10.1378/chest.130.2.517
- Vanhecke, T.E., Franklin, B.A., Miller, W.M., et al. (2009) Cardiorespiratory fitness and sedentary lifestyle in the morbidly obese. Clinical Cardiology, 32, 121-124. doi:10.1002/clc.20458
- Cortright, R.N., Sandhoff, K.M., Basilio, J.L., et al. (2006) Skeletal muscle fat oxidation is increased in AfricanAmerican and white women after 10 days of endurance exercise training. Obesity, 14, 1201-1210. doi:10.1038/oby.2006.137
- Privette, J.D., Hickner, R.C., Macdonald, K.G., et al. (2003) Fatty acid oxidation by skeletal muscle homogenates from morbidly obese black and white American women. Metabolism, 52, 735-738. doi:10.1016/S0026-0495(03)00034-9
- De Souza, S.A., Faintuch, J., Fabris, S.M. et al. (2009) Six-minute walk test: Functional capacity of severely obese before and after bariatric surgery. Surgery for Obesity and Related Diseases, 5, 540-543. doi:10.1016/j.soard.2009.05.003
- Zarvosky, G.S., kim, D.J., Sylvestre, J.L. and Christou, N.V. (2008) Alveolar membrane diffusing capacity improves in the morbidly obese after bariatric surgery. Obesity Surgery, 18, 256-263. doi:10.1007/s11695-007-9294-9
- Davila-Cervantes, A., Dominguez-Cherit, G., Borunda, D., Gamino, R., Vargas-Vorackova, F., González-Barranco, J. and Herrera, M.F. (2004) Impact of surgically-induced weight loss on respiratory function: A prospective analysis. Obesity Surgery, 14, 1389-1392. doi:10.1381/0960892042583996
- Braulio, V.B., Furtado, V.C.S., Silveira, M.G., Fonseca, M.H. and Oliveira, J.E. (2010) Comparison of body composition methods in overweight and obese Brazilian women. Arquivos Brasileiros de Endocrinologia & Metabologia, 54, 398-405. doi:10.1590/S0004-27302010000400009
- Pateyjohns, I.R., Brinkworth, G.D., Buckley, J.D., Noakes, M. and Clifton, P.M. (2006) Comparison of three bioelectrical impedance methods with DXA in overweight and obese men. Obesity, 14, 2064-2070. doi:10.1038/oby.2006.241
- Miller, M.R., Hankinson, J., Brusasco, V., Burgos, F., Casaburi, R., Coates, A., et al. (2005) Series ATS/ERS task torce: Standardisation of lung function testing. Standardisation of spirometry. European Respiratory Journal, 26, 319-338. doi:10.1183/09031936.05.00034805
- Costa, D., Gonçalves, H.A., De Lima, L.P., Ike, D., Cancelliero, K.M. and Montebelo, M.I. (2010) New reference values for maximal respiratory pressures in the Brazilian Population. Jornal Brasileiro de Pneumologia, 36, 306- 312. doi:10.1590/S1806-37132010000300007
- Enright, P.L. and Sherrill, D.L. (1998) Reference equation for the six-minute walk in healthy adults. American Journal of Respiratory and Critical Care Medicine, 158, 1384-1387. doi:10.1164/ajrccm.158.5.9710086
- Ross, R.M., Murthy, J.N., Wollak, I.D. and Jackson, A.S. (2010) The sixtminute walk test accurately estimates mean peak oxygen uptake. BMC Pulmonary Medicine, 10, 31. doi:10.1186/1471-2466-10-31
- Knudson, R.J., Lebowitz, M.D., Holberg, C.J. and Burrows, B. (1983) Changes in the normal maximal expiratory flow-volume curve with growth and aging. American Review of Respiratory Disease, 127, 725-734.
- Valezi, A.C., Mali Junior, J., De Menezes, M.A., De Brito, E.M. and De Souza, S.A. (2010) Weight loss outcome after silastic ring Roux-en-Y gastric bypass: 8 years of follow-up. Obesity Surgery, 20, 1491-1495. doi:10.1007/s11695-010-0264-2
- Xavier, M.A.F., Ceneviva, R., Terra Filho, J. and Sankarankutty, A.K. (2010) Pulmonary function and quality of life in patients with morbid obesity six months after bariatric surgery. Acta Cirúrgica Brasileira, 25, 407-415. doi:10.1590/S0102-86502010000500005
- Serés, L., Lopez-Ayerbe, J., Coll, R., Rodriguez, O., Vila, J., Formiguera, X., Alastrue, A., Rull, M. and Valle, V. (2006) Increased exercise capacity after surgically induced weight loss in morbid obesity. Obesity, 14, 273-279. doi:10.1038/oby.2006.35
- Maniscalco, M., Zedda, A., Giardiello, C., et al. (2006) Effect of bariatric surgery on the six-minute walk test in severe uncomplicated obesity. Obesity Surgery, 16, 836- 841. doi:10.1381/096089206777822331
- Stegen, S., Derave, W., Calders, P., Van Laethem, C. and Pattyn, P. (2011) Physical fitness in morbidly obese patients: effect of gastric bypass surgery and exercise training. Obesity Surgery, 21, 61-70. doi:10.1007/s11695-009-0045-y
- De Aquino, L.A., Pereira, S.E., Silva, J.S., Sobrinho, C.J.S. and Ramalho, A. (2012) Bariatric surgery: Impact on body composition after Roux-en-Y gastric bypass. Obesity Surgery, 22, 195-200. doi:10.1007/s11695-011-0500-4
- Domingos-Benício, N.C., Gastaldi, A.C., Perecin, J.C., Avena, K.M., Guimarães, R.C., Sologuren, M.J.J. et al. (2004) Medidas espirométricas em pessoas eutróficas e obesas nas posições ortostática, sentada e deitada. Revista da Associação Médica Brasileira, 50, 142-147. doi:10.1590/S0104-42302004000200028
- Wadstrom, C., Muller-Suur, R. and Backman, L. (1991) Influence of excessive weight loss on respiratory function. A study of obese patients following gastroplasty. European Journal of Surgery, 157, 341-346.
NOTES
*Conflict of Interest: The authors declare there is no conflict of interests.

