Case Reports in Clinical Medicine
Vol.2 No.1(2013), Article ID:28888,5 pages DOI:10.4236/crcm.2013.21007
Ossified thoracic spinal meningioma with hematopoiesis: A case report and review of the literature
![]()
1Department of Pathology, Nagasaki University Hospital, Nagasaki, Japan; *Corresponding Author: toma@nagasaki-u.ac.jp
2Department of Neurosurgery, Nagasaki University Hospital, Nagasaki, Japan
Received 22 January 2013; revised 28 February 2013; accepted 5 March 2013
Keywords: Spinal Cord; Meningioma; Ossification; Extramedullary Hematopoiesis; Spinal Tumor
ABSTRACT
Meningiomas account for 25% of spinal tumors, and they are often located in the thoracic spine. The ossified subtype is even rarer, and those with hematopoiesis are rarely described. The mechanism of bone formation has not yet been clarified. A case of ossified spinal meningioma with hematopoiesis occurring in a 78-year-old woman is described. Magnetic resonance imaging revealed a lesion with a dural tail sign at the T9 level located dorsal to the spinal cord. Computerized tomography revealed a high density lesion, as high as the bone signal. Total resection was performed, and the symptoms improved. Pathological findings revealed many psammoma bodies (PBs), bone formation, and bone marrow with hematopoiesis. Both PBs and bone seemed to be based on the same background of calcified structures. This report is the second dealing with ossified spinal meningioma with hematopoiesis. The hardness of the tumor can make the operation more difficult, so that the operation should be performed carefully to avoid injuring the spinal cord.
1. INTRODUCTION
Spinal tumors are rare [1], and meningiomas account for 25% of such tumors [2-7]. Typically, meningiomas form intradural extramedullary tumors. They account for 40% of adult extramedullary lesions [2], and they are often located in the thoracic spine [2,4,6].
Ossified meningiomas account for approximately 1% of all meningiomas [8]. Even ossified spinal meningiomas are extremely rare and may be estimated to account for 0.7% - 5.5% of all spinal meningiomas [7,9,10]. There are only a few reported cases of bone formation with hematopoiesis [11].
Most meningiomas are benign and slow growing [5,8, 12,13], and the goal of treatment should be total surgical resection [14]. The ossification type is an additional issue for treatment because of difficulty in resection [6,15,16].
A case of ossified thoracic meningioma with hematopoiesis and a literature review are presented.
2. CASE REPORT
A 78-year-old woman complained of right leg pain that needed a cane for three months. Two months before the operation, pain appeared in both legs that prevented knee extension, resulting in her having to walk on her knees. Detailed examination disclosed a thoracic spinal tumor, and she was referred to our hospital for further detailed examination in September.
Thoracic magnetic resonance imaging (MRI) revealed an intradural, extramedullary tumor at the T9 level located dorsal to the spinal cord, which was severely compressed. The lesion was hypointense on both T1-weighted and T2-weighted MRI, with a dural tail sign (Figure 1). Computed tomography (CT) demonstrated that the lesion and the bone had the same isodensity (Figures 2A and B). These features suggested a spinal meningioma with areas of calcification or ossification.
At surgery, T8-10 laminectomy and excision of the outer yellow ligament were performed, and the dural sac was exposed. The dura attached to the lesion was hard and continuous with the tumor. The dura was divided into inner and outer layers, and the outer was kept.
The boundary between the tumor and the spinal cord was clear, and the tumor did not adhere to the arachnoid. Total resection of the tumor was performed with the inner dura, after which closure of the outer dura and T9-10 laminoplasty were performed.
Postoperatively, the symptoms improved, and the pa-
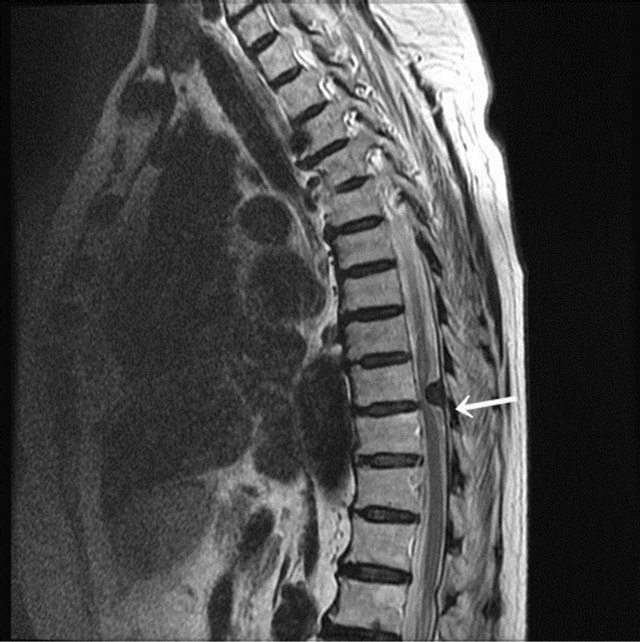
Figure 1. MRI (T2-weighted) of the 14 × 9 × 6 mm intradural extramedullary tumor at the T9 level. It is located dorsal to the spinal cord and compresses the spinal cord from the back. The tumor shows hypoisointensity. The lower part of the tumor shows the dural tail sign comparable finding (arrow).
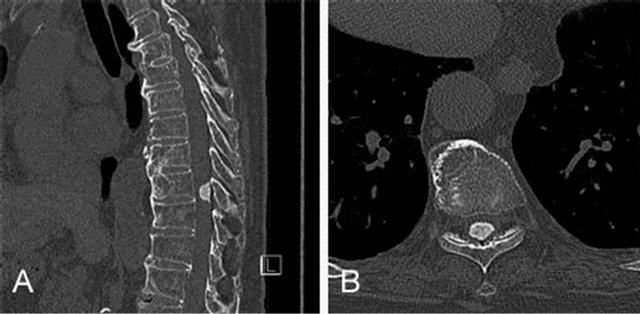
Figure 2. CT A: (sagittal section): the intradural tumor with high density, as high as the bone signal, is located dorsal to the spinal cord. There is multiple osteophyte formation and narrowing of the inner vertebral spaces; B: (transverse section): the spinal cord is compressed from behind, slight convex scoliosis is also seen on the right side, and the 5/6 right intervertebral foramen is constricted.
tient was discharged well.
3. PATHOLOGICAL EXAMINATION
The lesion measured 14.0 × 9.0 × 6.0 mm. The paraffin sections, stained with hematoxylin and eosin (H & E), revealed that the tumor consisted of bland elongated cells with indistinct cell borders and short spindle nuclei. There were psammoma bodies (PBs) and bone formation (Figure 3A). Neither mitotic figures nor necrosis was observed. Many mature bones with a mosaic pattern and bone marrow with hematopoiesis were evident (Figure 3B).
There were areas with crowded PBs (Figure 4A), but the PBs were not always continuous with ossification. There were various combinations of patterns, with gathering of PBs with surrounding hyaline connective tissue (Figure 4A), mature bone entrapping a PB (Figure 4B), mature bone formation without a PB (Figure 4C), and bone formation adjacent to the PBs (Figure 4D). Based on these findings, the lesion was diagnosed as an ossified thoracic meningioma.
4. LITERATURE REVIEW
There have been only 16 reported cases of ossified spinal meningioma in PubMed, including the present case (Table 1). The age range was 15 - 78 years, with a male: female ratio of 2:14, showing clear female predominance. Six cases were reported to have bone marrow formation, but only 2 cases had evidence of hematopoiesis.
5. DISCUSSION
Intraspinal tumors are rare [1]. Meningiomas are com-
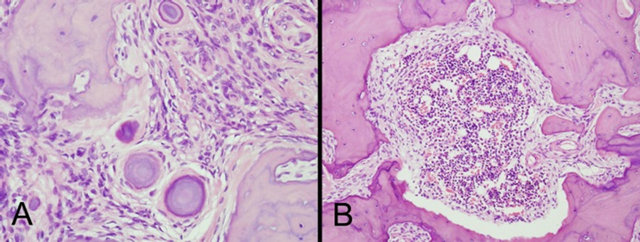
Figure 3. A: The neoplastic lesion consists of elongated cells with indistinct cell borders, short spindle nuclei, PBs, and bone formation. The lamellar bone shows mosaic pattern. (H & E stain, original magnification ×200) B: Formation of mature bones including bone marrow with hematopoiesis is seen (H & E stain, original magnification ×100).
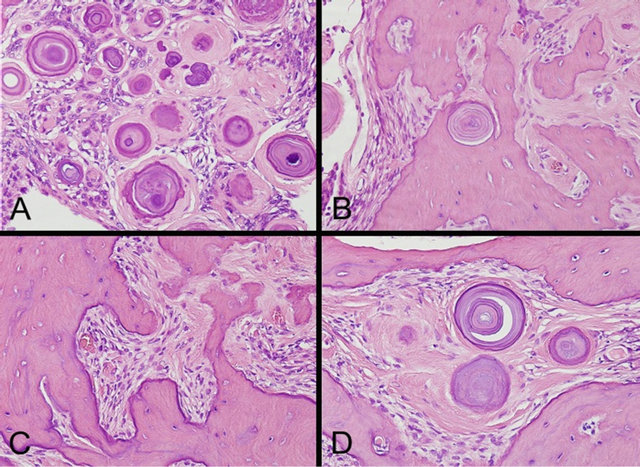
Figure 4. A: There are many PBs; some surrounded by hyaline tissue; B: Mature bone formation entrapping a PB; C: Mature bone formation without PB; D: Mature bones and PB formation (H & E stain, original magnification ×200).
Table 1. Reported cases of ossified spinal meningioma.
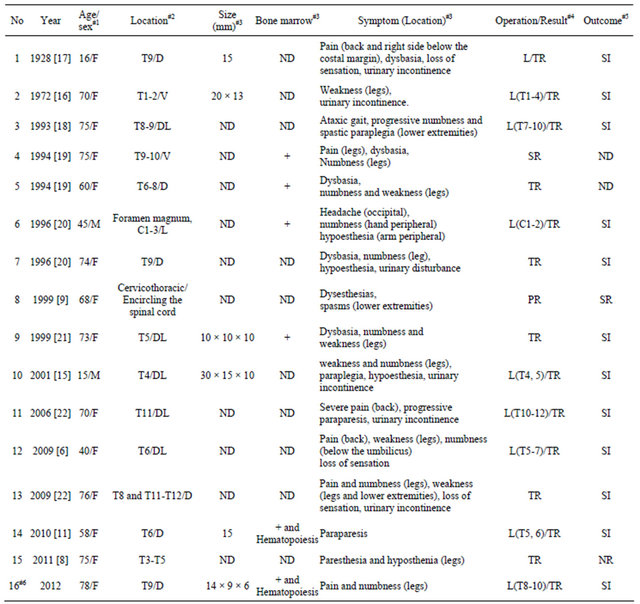
#1M: Male; F: Female; #2D: Dorsal to spinal cord; V: Ventral to spinal cord; L: Lateral to spinal cord; DL: Dorsolateral to the spinal cord; #3ND: No data; #4L: Laminectomy; R: Resection; PR: Partial resection; SR: Subtotal resection; TR: Total resection; #5SI: Symptoms improved; SR: Symptoms remained; NR: No recurrences; ND: No data; #6Present case.
mon; accounting for 25% of spinal meningiomas [2-7]. There is a difference in location depending on sex. In women, the majority of meningiomas is located in the thoracic region (80%), followed by the cervical (15%) and lumbosacral (5%) regions [2,4,6,23-25], while in men, meningiomas are located in the thoracic region (50%), followed by the cervical (40%) region [23,26].
Spinal ossified meningiomas are extremely rare, with only 16 cases in PubMed, including the present case (Table 1). The histogenesis of the ossification in meningiomas is not clear. There are some hypotheses about the ossification. Barresi et al. presented two pathways. One was that bone formation was the final step of longstanding calcification, as frequently found in psammomatous meningiomas. The other was that the neoplastic cells surrounding bone trabeculae develop osteoblast-like properties, expressing osteopontin, as well as enchondral ossification with remodeling, by osteoclasts [8]. Uchida et al. mentioned that premature arachnoid cells with pluripotency, which are the origin of the neoplastic cells, differentiate into the metaplastic cells with bone formation [27].
The present case showed remarkable PBs formation. The hyalinized collagen surrounding the PBs was continuous with those attached to bone formation. There was also an area where bone entrapped a PB. Though there were no transitions between PB and bone, they seemed to be related. Both PB and bone might be based on same background tendency to develop calcified structures.
Licci et al. stated that the presence of lamellar bone in the lesion is sometimes reported; however, the formation of hematopoietic tissue in the marrow space is rarely mentioned [11]. Therefore, the present case is only the second case of ossified spinal meningioma with hematopoietic bone marrow. Mathew et al. suggested two mechanisms of de novo extramedullary hematopoiesis within meningiomas. First, the induced neoplastic growth of meningeal cells may cause erythroid differentiation in the multipotent stem cells. Second, the quiescent heterotopic cell rests that were isolated during development may develop proliferative changes and differentiation by the increased oxygen and nutritional demands of the tumor cells [28]. Licci et al. mentioned that a third mechanism of mesenchymal multipotentiality of meningeal or meningiomatous cells could cause hematopoietic differentiation [11].
Because of spatial restriction, symptoms are more frequent with spinal meningiomas than with cranial meningiomas [19]. The most common symptoms are pain [7, 10,12], followed by muscle weakness such as paresis or plegia, and sensory loss such as hypoesthesia, paresthesia, or anesthesia [12]. In the cases of spinal ossified meningiomas, muscle weakness is more frequent (Table 1).
There are some reports mentioning difficulty in resection for calcified or ossified meningiomas [6-8,15,16]. In the present case, probably because the tumor was dorsal to the spinal cord and it was not too large, the operation was not difficult.
When the tumors are resected completely, the symptoms improve [6,11,15,16,21,22,27]. However, when the tumor is not resected completely because of its hardness or large size, the symptoms remain [9].
In conclusion, spinal ossified meningiomas with hematopoietic bone marrow are extremely rare. The histogenesis of the bone and hematopoiesis is still unknown. The hardness of the tumor makes surgery more difficult, but a good outcome is expected with total resection of the tumor. Careful surgery is needed for hard tumors to avoid spinal cord injury.
REFERENCES
- Helseth, A. and Mørk, S.J. (1989) Primary intraspinal neoplasms in Norway, 1955 to 1986. A population-based survey of 467 patients. Journal of Neurosurgery, 71, 842- 845. doi:10.3171/jns.1989.71.6.0842
- Raza, S.M., Anderson, W.S., Eberhart, C.G., Wolinsky, J.P. and Gokaslan, Z.L. (2005) The application of surgical cordectomy in the management of an intramedullary-extramedullary atypical meningioma: Case report and literature review. Journal of Spinal Disorders & Techniques, 18, 449-54. doi:10.1097/01.bsd.0000155032.69394.23
- Wang, X.Q., Zeng, X.W., Zhang, B.Y., Dou, Y.F., Wu, J.S., Jiang, C.C., Zhong, P. and Chen, H. (2012) Spinal meningioma in childhood: Clinical features and treatment. Child’s Nervous System, 28, 129-136. doi:10.1007/s00381-011-1570-2
- Cramer, P., Thomale, U.W., Okuducu, A.F., Lemke, A.J., Stockhammer, F. and Woiciechowsky, C. (2005) An atypical spinal meningioma with CSF metastasis: Fatal progression despite aggressive treatment. Case report. Journal of Neurosurgery: Spine, 3, 153-158. doi:10.3171/spi.2005.3.2.0153
- Delgado-López, P.D., Martín-Velasco, V., Castilla-Díez, J.M., Fernández-Arconada, O., Corrales-García, E.M., Galacho-Harnero, A., Rodríguez-Salazar, A. and PérezMies, B. (2006) Metastatic meningioma to the eleventh dorsal vertebral body: Total en bloc spondylectomy. Case report and review of the literature. Neurocirugia, 17, 240- 249. doi:10.4321/S1130-14732006000300004
- Tahir, M., Usmani, N., Ahmad, F.U., Salmani, S. and Sharma, M.S. (2009) Spinal meningioma containing bone: A case report and review of literature. BMJ Case Reports, Epub.
- Roux, F.X., Nataf, F., Pinaudeau, M., Borne, G., Devaux, B. and Meder, J.F. (1996) Intraspinal meningiomas: Review of 54 cases with discussion of poor prognosis factors and modern therapeutic management. Surgical Neurology, 46, 458-464. doi:10.1016/S0090-3019(96)00199-1
- Barresi, V., Caffo, M., Ieni, A., Alafaci, C. and Tuccari, G. (2011) Osteoblastic meningiomas: Clinico-pathological and immunohistochemical features of an uncommon variant. Journal of Neurooncology, 105, 225-232. doi:10.1007/s11060-011-0588-3
- Klekamp, J. and Samii, M. (1999) Surgical results for spinal meningiomas. Surgical Neurology, 52, 552-562. doi:10.1016/S0090-3019(99)00153-6
- Levy Jr., W.J., Bay, J. and Dohn, D. (1982) Spinal cord meningioma. Journal of Neurosurgery, 57, 804-812. doi:10.3171/jns.1982.57.6.0804
- Licci, S., Limiti, M.R., Callovini, G.M., Bolognini, A., Gammone, V. and Di Stefano, D. (2009) Ossified spinal tumour in a 58-year-old woman with increasing paraparesis. Neuropathology, 30, 194-196. doi:10.1111/j.1440-1789.2009.01076.x
- Gezen, F., Kahraman, S., Canakci, Z. and Bedük, A. (2000) Review of 36 cases of spinal cord meningioma. Spine, 25, 727-731.
- Perry, A., Louis, D.N., Scheithauer, B.W., et al. (2007) Meningiomas. In: Louis, D.N., Ohgaki, H., Wiestler, O.D. and Cavenee, W.K., Eds., WHO Classification of Tumors of the Central Nervous System. IARCC Press, Lyon, 164- 172.
- Saito, T., Arizono, T., Maeda, T., Terada, K. and Iwamoto, Y. (2001) A novel technique for surgical resection of spinal meningioma. Spine, 26, 1805-1808.
- Naderi, S., Yilmaz, M., Canda, T. and Acar, U. (2001) Ossified thoracic spinal meningioma in childhood: A case report and review of the literature. Clinical Neurology and Neurosurgery, 103, 247-249. doi:10.1016/S0303-8467(01)00157-3
- Freidberg, S.R. (1972) Removal of an ossified ventral thoracic meningioma. Case report. Journal of Neurosurgery, 37, 728-730. doi:10.3171/jns.1972.37.6.0728
- Rogers, L. (1928) A spinal meningioma containing bone. British Journal of Surgery, 15, 675-677.
- Niijima, K., Huang, Y.P., Malis, L.I. and Sachdev, V.P. (1993) Ossified spinal meningioma en plaque. Spine, 18, 2340-2343.
- Kitagawa, M., Nakamura, T., Aida, T., Iwasaki, Y., Abe, H. and Nagashima, K. (1994) Clinicopathologic analysis of ossification in spinal meningioma. Noshuyo Byori, 11, 115-119.
- Nakayama, N., Isu, T., Asaoka, K., Harata, T., Hayashi, S., Aoki, T., Mabuchi, S. and Takahashi, T. (1996) Two cases of ossified spinal meningioma. No Shinkei Geka, 24, 351- 355. In Japanese.
- Huang, T.Y., Kochi, M., Kuratsu, J. and Ushio, Y. (1999) Intraspinal osteogenic meningioma: Report of a case. Journal of the Formosan Medical Association, 98, 218- 221.
- Liu, C.L., Lai, P.L., Jung, S.M. and Liao, C.C. (2006) Thoracic ossified meningioma and osteoporotic burst fracture: Treatment with combined vertebroplasty and laminectomy without instrumentation: Case report. Journal of Neurosurgical Spine, 4, 256-259. doi:10.3171/spi.2006.4.3.256
- Saraceni, C. and Harrop, J.S. (2009) Spinal meningioma: Chronicles of contemporary neurosurgical diagnosis and management. Clinical Neurology and Neurosurgery, 111, 221-226. doi:10.1016/j.clineuro.2008.10.018
- Gottfried, O.N., Gluf, W., Quinones-Hinojosa, A., Kan, P. and Schmidt, M.H. (2003) Spinal meningiomas: Surgical management and outcome. Neurosurgical Focus, 14, e2. doi:10.3171/foc.2003.14.6.2
- McCormick, P.C., Post, K.D. and Stein, B.M. (1990) Intradural extramedullary tumors in adults. Neurosurgery Clinics of North America, 1, 591-608.
- Van Goethem, J.W., van den Hauwe, L., Ozsarlak, O., De Schepper, A.M. and Parizel, P.M. (2004) Spinal tumors. European Journal of Radiology, 50, 159-176. doi:10.1016/j.ejrad.2003.10.021
- Uchida, K., Nakajima, H., Yayama, T., Sato, R., Kobayashi, S., Mwaka, E.S., Imamura, Y. and Baba, O.H. (2009) Immunohistochemical findings of multiple ossified en plaque meningiomas in the thoracic spine. Journal of Clinical Neuroscience, 16, 1660-1662. doi:10.1016/j.jocn.2009.03.013
- Mathews, M.S., Duma, C.M., Brant-Zawadzki, M., Hasso, A., Westhout, F.D., Klein, D.J. and Vanhorn, D. (2008) Extramedullary hematopoeisis within a convexity meningioma. Surgical Neurology, 69, 522-525. doi:10.1016/j.surneu.2007.02.017

