International Journal of Clinical Medicine
Vol.3 No.4(2012), Article ID:20898,3 pages DOI:10.4236/ijcm.2012.34055
Secondary Signs of Surgical Epistaxis Management*
![]()
Department of Otolaryngology-Head and Neck Surgery, North Hospital, Saint-Etienne University Hospital Centre, Saint-Etienne, France.
Email: {#alexander.asanau, alexander.oletski, j.michel.prades, andrei.timochenko}@chu-st-etienne.fr
Received May 21st, 2012; revised June 25th, 2012; accepted July 10th, 2012
Keywords: Epistaxis; Endoscopy; Epistaxis Surgery
ABSTRACT
Severe epistaxis management remains a challenge to otolaryngologists. Despite the large choice of treatment strategies to control epistaxis, the method of regional haemostasis via edoscopic arterial ligation has become frequently used. Arterial supply occlusion is usually performed by electrocautery or application of titanium clips. After placement of titanium clips, they will remain in place forever and could surprisingly be rediscovered later on CT-scan. Most of otolaryngologists are familiar with this method and are able to identify these clips, however, it could be more difficult for radiologists and other practitioners. In order to draw the attention of other specialists to the existence of this method and to help them correctly interpret such CT-scans, the authors present an example of a case that troubled radiologists. In addition, the authors also discussed the vascular supply of the nasal fossa and methods of severe epistaxis management.
1. Introduction
Severe epistaxis management remains a challenge to otolaryngologists. Despite the large choice of treatment strategies of epistaxis control, the method of regional hemostasis via endoscopic arterial ligation has become frequently used [1]. This method is commonly effective and does not cause serious consequences to patients. During the surgical procedure, sphenopalatine artery ligation with or without anterior ethmodal artery ligation is generally performed and may be unior bilateral. Arterial supply occlusion is usually performed by electrocautery or application of titanium clips. After placement of titanium clips, they will remain in place forever and could surprisingly be rediscovered later on CT-scan. Most of otolaryngologists are familiar with this method and are able to identify these clips, however, it could be more difficult for other practitioners [2,3]. In order to draw the attention of other specialists to the existence of this method and to help them correctly interpret such CT-scans, the authors present an example of a case that troubled radiologists.
2. Case Report
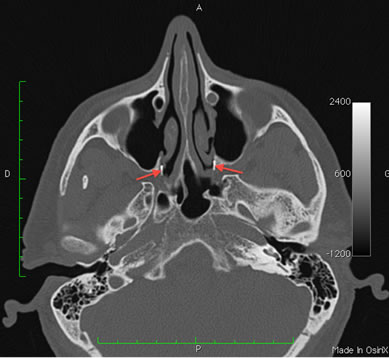
A 76-year-old man, who recently arrived in our region, presented to the emergency department with recurrent headache, without other neurological symptoms. He had a remote history of epistaxis managed under general anesthesia. On physical examination, the blood pressure was normal; the funduscopic examination did not reveal papilledema. A cranial CT-scan was performed to eliminate intracranial lesion; and did not show any cause of headache. However, several strange findings troubled our radiologists. The unidentified findings were located in the nose (Figures 1(a) and (b)) and in the orbits (Figures 1(c) and (d)). For further clarification, the patient with CT-scan images was referred to our department. The nasal endoscopic exam was perfect and the following explanation for the images was proposed: “These images correspond to titanium hemostatic clips that were used during endoscopic regional hemostasis to control an epistaxis; both sphenopalatine (Figures 1(a) and (b)) and anterior ethmoidal (Figures 1(c) and (d)) arteries were bilaterally ligated” [1]. The patient was then directed to the Neurology department for further investigation.
3. Discussion
In the past years, the main therapy of severe epistaxis has become the surgical endoscopic ligation of the arterial supply of the nasal cavity [1]. It has evolved from external carotid ligation to minimally invasive approaches. This management is more cost effective than embolization and may be less risky [4]. Nevertheless, alternative methods can be employed with proper patient selection
 (a)
(a)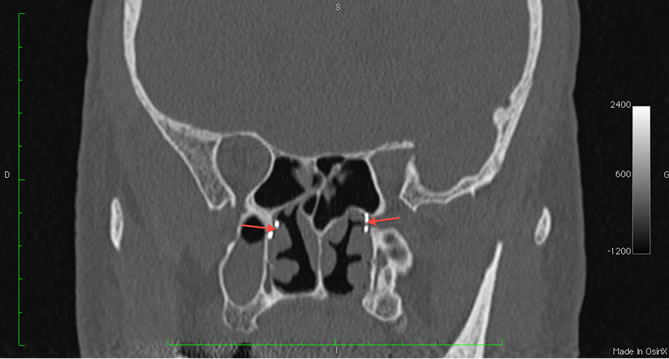 (b)
(b)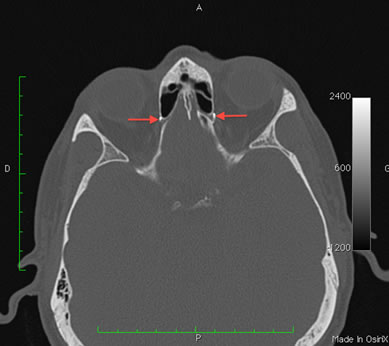 (c)
(c)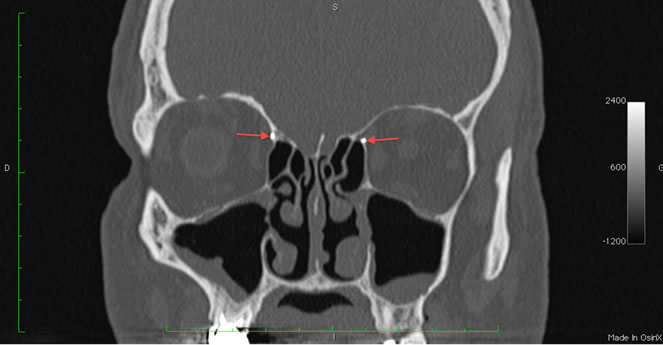 (d)
(d)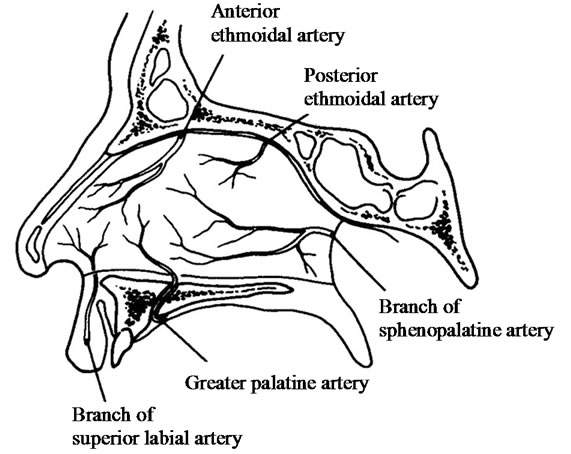 (e)
(e)
Figure 1. (a) CT-scan (horizontal section view), arrows indicate the emplacement of titanium clips at the sphenopalatine foramen level; (b) CT-scan (coronal section view), arrows indicate the emplacement of titanium clips at the sphenopalatine foramen level; (c) CT-scan (horizontal section view), arrows indicate the emplacement of titanium clips in the medial wall of the orbit; (d) CT-scan (coronal section view), arrows indicate the emplacement of titanium clips in the medial wall of the orbit; (e) Arterial anatomy of the nasal septum.
[5]. The practicing physician has to be familiar with the advantages and disadvantages of selected course of action. She/he should be capable as well to choose the part of arterial supply to block during a hemostatic procedure. The choice could be difficult, due to the fact that sometimes it impossible to identify precisely the epistaxis origin [1].
The vascular anatomy of the nasal fossa is complex. This radiological case reminds us that the intranasal blood supply depends of two arterial systems that could anastomose between each other. There is the system of external carotid artery (ECA) and the system of internal carotid artery (ICA) [6,7]. In addition, veins always accompany arteries.
Five main arteries supply the mucoperiosteum of the nasal cavity on each side: three arteries depend on the ECA and two arteries depend on the ICA (Figure 1(e)). The sphenopalatine artery, which arrives via the sphenopalatine foramen, is the most important of these vessels [8]. The greater palatine artery enters in the nose by the incisive foramen. Both arteries originate from the maxillary artery. The septal branch of the superior labial artery, which originates from the facial artery, supplies nasal fossa by the pyriform aperture.
The anterior and posterior ethmoidal arteries originate from the ophthalmic artery, branch of the ICA. To supply the ethmoid they pass through the successive foramina, which lie in the medial wall of the orbit along the frontoethmoidal suture line.
During severe epistaxis management only the branches of the sphenopalatine arteries and anterior ethmoidal arteries could be considered to occlusion without serious consequences. In the opposite case, complications may occur [9]. The method of angiographic embolization that offers the advantages of avoiding surgery or general anesthesia should possibly not be used if there is other option [3,4]. As far as the anterior ethmoidal artery selective occlusion is concerned, it is feasible only by surgical approach [1].
To ligate arterial branches we usually use the Montgomery-Youngs Rhinoforce® II Clip Applicator 452650 C or D (Karl Storz GmbH & Co. KG, Germany) with titanium clips 8665T (Karl Storz GmbH & Co. KG, Germany). Once the sphenopalatine artery, arising from shenopalatine foramen, was identified in the nasal fossa, one titanium clip is placed on each main branch of it with care taken to ensure that the entire width of the artery is enclosed within the clip [1]. It is always performed under endoscopic guidance to minimize the artery damage. When indicated, the anterior etmoidal artery is clipped in the space between the retracted periorbita and the lamina papyracea, by use of the standard external approach along the frontoethmoidal suture [1]. We neither use the diathermy of vessels nor the placing of multiple clips, because it carries potential risk of vascular division and retraction with continued bleeding from a difficult-toaccess source.
4. Conclusion
This case demonstrates that severe epistaxis could be managed surgically and that some practitioners may not be aware of it. Secondary signs of surgical treatment of epistaxis may be discovered later on CT-scan and sometimes not interpreted correctly. In order to provide timely and most efficient care to patients, it is important for radiologists and other specialists to be aware of such method and to be able to read and fully understand such CT-scans.
REFERENCES
- A. Asanau, A. P. Timoshenko, P. Vercherin, C. Martin and J. M. Prades, “Sphenopalatine and Anterior Ethmoidal Artery Ligation for Severe Epistaxis,” Annals of Otology, Rhinology and Laryngology, Vol. 118, No. 9, 2009, pp. 639-644.
- K. Strach, A. Schrock, K. Wilhelm, et al., “Endovascular Treatment of Epistaxis: Indications, Management, and Outcome,” Cardiovascular and Interventional Radiology, Vol. 34, No. 6, 2011, pp. 1190-1198. doi:10.1007/s00270-011-0155-5
- A. Asanau, A. P. Timoshenko and J. M. Prades, “Strategy of Modern Epistaxis Management,” Cardiovascular and Interventional Radiology, Vol. 35, No. 3, 2011, pp. 709- 710. doi:10.1007/s00270-011-0231-x
- J. P. Bent III and B. P. Wood, “Complications Resulting from Treatment of Severe Posterior Epistaxis,” Journal of Laryngology & Otology, Vol. 113, 1999, pp. 252-254. doi:10.1017/S0022215100143701
- R. P. Manes, “Evaluating and Managing the Patient with Nosebleeds,” Medical Clinics of North America, Vol. 94, No. 5, 2010, pp. 903-912. doi:10.1016/j.mcna.2010.05.005
- F. N. Ritter, “The Vasculature of the Nose,” Annals of Otology, Rhinology and Laryngology, Vol. 79, 1970, pp. 468-474
- A. G. Osborn, “The Nasal Arteries,” American Journal of Roentgenology, Vol. 130, No. 1, 1978, pp. 89-97
- J. M. Prades, A. Asanau, A. P. Timoshenko, M. B. Faye and C. Martin, “Surgical Anatomy of the Sphenopalatine Foramen and Its Arterial Content,” Surgical and Radiologic Anatomy, Vol. 30, No. 7, 2008, pp. 583-587. doi:10.1007/s00276-008-0390-x
- N. P. Christensen, D. S. Smith, S. L. Barnwell and M. K. Wax, “Arterial Embolization in the Management of Posterior Epistaxis,” Otolaryngology—Head and Neck Surgery, Vol. 133, No. 5, 2005, pp. 748-753. doi:10.1016/j.otohns.2005.07.041
NOTES
*All the authors contributed equally to the work described in this paper and all take responsibility for it. None of the information described in this paper has been published elsewhere. None of the authors have any conflict of interest.
#Corresponding author.

