Open Journal of Thoracic Surgery
Vol.3 No.2(2013), Article ID:32639,6 pages DOI:10.4236/ojts.2013.32012
Diabetics Have the Same Risk and Benefits Regarding Postoperative Amiodarone Prophylaxis for Atrial Fibrillation When Undergoing Surgery for Lung Cancer
![]()
1Department of Cardiothoracic and Vascular Surgery, Institute of Clinical Medicine, Aarhus University Hospital, Aarhus, Denmark; 2Department of Cardiothoracic and Vascular Surgery, Institute of Clinical Medicine, Odense University Hospital, Odense, Denmark.
Email: *larspeterriber@gmail.com
Copyright © 2013 Lars P. Riber et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received March 28th, 2013; revised May 1st, 2013; accepted May 9th, 2013
Keywords: Lung Surgery; Atrial Fibrillation; Diabetics
ABSTRACT
Background: To evaluate if the risk for developing atrial fibrillation after lung surgery is higher for diabetics than non-diabetic patients and whether diabetic status prolongs the length of in-hospital stay. Objective: To compare the outcome of amiodarone prophylaxis in diabetics and non-diabetics. Design: Subgroup analysis within a randomized, controlled, double-blinded trial. Results: Development of atrial fibrillation was equally frequent among diabetics (18.2%) and non-diabetics (20.5%) (p = 1.00). Atrial fibrillation occurred in 7.1% of prophylactic diabetics and in 9.3% of prophylactic non-diabetics, while 37.5% non-prophylactic diabetics and 31.3% non-prophylactic non-diabetics experienced atrial fibrillation (p = 0.31). Prophylactic amiodarone was equally effective in diabetics as in non-diabetics with a relative risk of 3.5 (1.8 - 67.0) and the number need to treat of 4.4 (3.3 - 8.3) (p = 0.31). The length of in-hospital stay for diabetics was equal to non-diabetics with an average stay of 7.1 versus 8 days at Aarhus University Hospital (p = 0.61) with similar stays at intermediary and intensive care unit as well as total in-hospital stay of 8.9 versus 10 days (p = 0.60). Conclusions: Diabetics have the same risk of atrial fibrillation and the same benefits from prophylactic amiodarone as non-diabetics after surgery for lung cancer. Furthermore, diabetics have the same length of stay as non-diabetics. No severe adverse effects were found in either group.
1. Introduction
Postoperative atrial fibrillation occurs in around 25% of patients undergoing lung surgery [1-4]. Former studies have shown a significant effect of amiodarone in treating postoperative atrial fibrillation [4,5]. Since a non-randomized prospective study had indicated that prophylactic amiodarone could be used as an effective prophylactic agent [6], we performed the “amiodarone prophylaxis for atrial fibrillation in patients undergoing surgery for lung cancer: a controlled, randomized, double blinded trial (PASCART trial)” to find a safe, practical, feasible, and effective mainly oral regimen to minimize the risk of developing postoperative atrial fibrillation for patients having lung surgery [7]. High dose of amiodarone administrated twice daily for the first five postoperative days after an initial intravenous loading bolus, was found to significantly reduce the risk of postoperative atrial fibrillation.
Diabetics are well known to have a higher postoperative morbidity [8-12], electrolyte imbalance [13] as well as prolonged in-hospital stay [14]. The postoperative increased morbidity in diabetics includes infections, prolonged postoperative anemia, electrolytic imbalance, adverse neurocognitive outcome and a higher risk of atrial fibrillation [13].
Theoretically, diabetics could accordingly have a higher risk of developing atrial fibrillation due to electrolytic imbalance and also be more resistant to prophylactic therapy.
Taken into consideration that amiodarone seems to protect diabetics and non-diabetics undergoing coronary artery bypass grafting equally [14], it is a disease in evolution [15-19], and in-hospital length of stay seems to be prolonged in diabetics [8-12,14], a subgroup analysis seemed relevant.
The hypothesis of this sub-group analysis was therefore that diabetics have a higher risk of developing postoperative atrial fibrillation, the length of in-hospital stay is prolonged for diabetics and that the prophylactic regime induced in the PASCART trial is less efficient in diabetic patients.
The aim of the study was to compare diabetics and non-diabetics in regards to the postoperative risk of developing atrial fibrillation in the length of in-hospital stay and to evaluate whether the instituted prophylactic regimen had the same effect in diabetics and non-diabetics.
2. Material and Methods
The study was described in the main article [7], why only a summary is referred.
2.1. Study Design
Subgroup analyses of the randomized, controlled trial entitled: “amiodarone prophylaxis for atrial fibrillation in patients undergoing surgery for lung cancer: a controlled, randomized, double blinded trial” (PASCART trial) [7].
Twenty-two (9%) of the 242 consecutively enrolled patients for lung surgery suffered from diabetes, which was registered in the continuous report form in the PASCART trial.
The study was performed at the department of Cardiothoracic and Vascular Surgery & Institute of Clinical Medicine, Aarhus University Hospital and local hospitals.
2.2. Statistical Analysis and Sample Size
Data Analysis
The original study population was stratified according to their diabetic status. Intention-to-treat analyses of the endpoints were performed. Thirty day relative risks and 95% confidence intervals were given. Heterogeneity between diabetics and non-diabetics was tested. Analyses regarding length of stay were performed using 2-way ANOVA. The data were analyzed using Stata 9© software (StataCorp, Texas, USA).
3. Results
3.1. Trial Flow & Baseline Characteristics
The trial flowchart and baseline characteristics showed no difference between the placebo and amiodarone groups [7] or between diabetics and non-diabetics with respect to prophylactic status (Table 1 & Figure 1). The patients had no record of atrial fibrillation and the operations performed were identical in the four groups. Eleven percent in the amiodarone group and seven percent in the placebo group suffered from diabetes (p = 0.26).
3.2. Endpoints
At 30 days of follow-up atrial fibrillation was equally distributed among diabetics (18.2%) and non-diabetics (20.5%) (p = 1.00) (Figure 2). The prophylactic regime instituted to prevent asymptomatic and symptomatic atrial fibrillation, was found to be equally efficient in diabetics and non-diabetics as atrial fibrillation occurred in 7.14% of prophylactic diabetics and in 9.26% of prophylactic non-diabetics. Thirty-eight percent of non-prophylactic diabetics and thirty-one percent of non-prophylactic non-diabetics experienced atrial fibrillation (p = 0.31). Prophylactic amiodarone was therefore found equally effective in diabetics as in non-diabetics with a relative risk of 3.5 (1.8 - 67.0) and the number need to treat of 4.4 (3.3 - 8.3) (p = 0.31) (Table 2).
The length of in-hospital stay for diabetics was equal to non-diabetics with an average stay of 7.1 versus 8 days at Aarhus University Hospital (p = 0.61) with similar stays at intermediary and intensive care unit as well as total in-hospital stay of 8.9 versus 10 days (p = 0.60) (Table 3).
There was further no sign that amiodarone prophylaxis did alter the total in-hospital length of stay for neither diabetic nor non-diabetic patients (Table 3).
4. Discussion
The risk of developing atrial fibrillation, the duration, and the time of occurrence after lung surgery was the same for diabetics and non-diabetics, why diabetic status was not found to be a risk factor for atrial fibrillation after lung surgery.
The efficiency of the instituted prophylaxis was the same for diabetics and non-diabetics in regards of preventing postoperative atrial fibrillation, and it is therefore a useful prophylactic regimen regardless of diabetic status.
Regarding length of stay, patients suffering from atrial fibrillation were hospitalized for a longer period than people having sinus rhythm [7], while there was no difference in in-hospital length of stay in concern to diabetic status. This indicates that diabetics have the same benefits as non-diabetics in regards to lung surgery and does not have an increased in-hospital length of stay due to enhanced perioperative morbidity resulting in a longer recovery period as described in former studies [8-11].
However the number of patients was a limitation as only 22 patients out of the study group of 242 patients
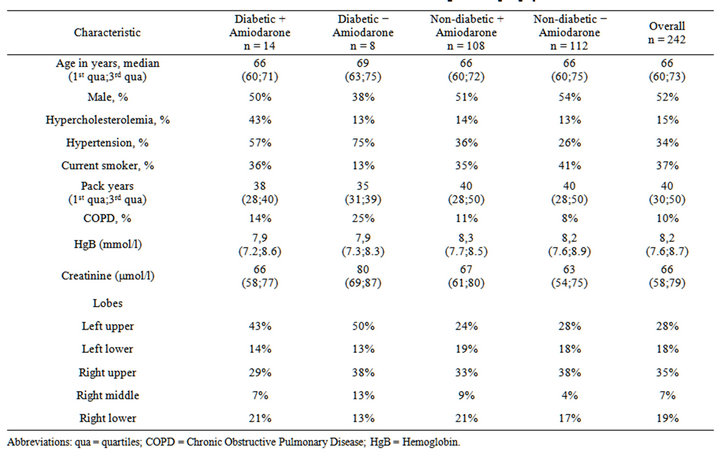
Table 1. Baseline data for diabetics and non-diabetics in regards to prophylactic status.
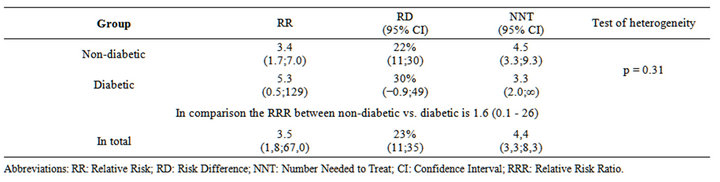
Table 2. Atrial fibrillation, relative and absolute effects regarding treatment arm and diabetic status.
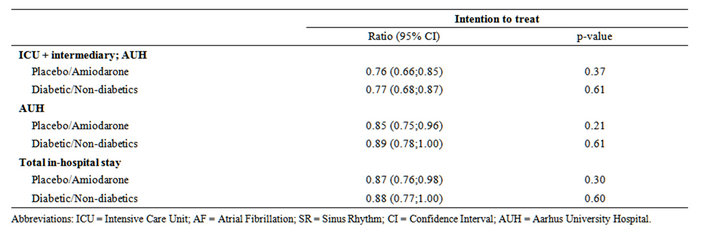
Table 3. Length of stay regarding treatment and diabetic status.
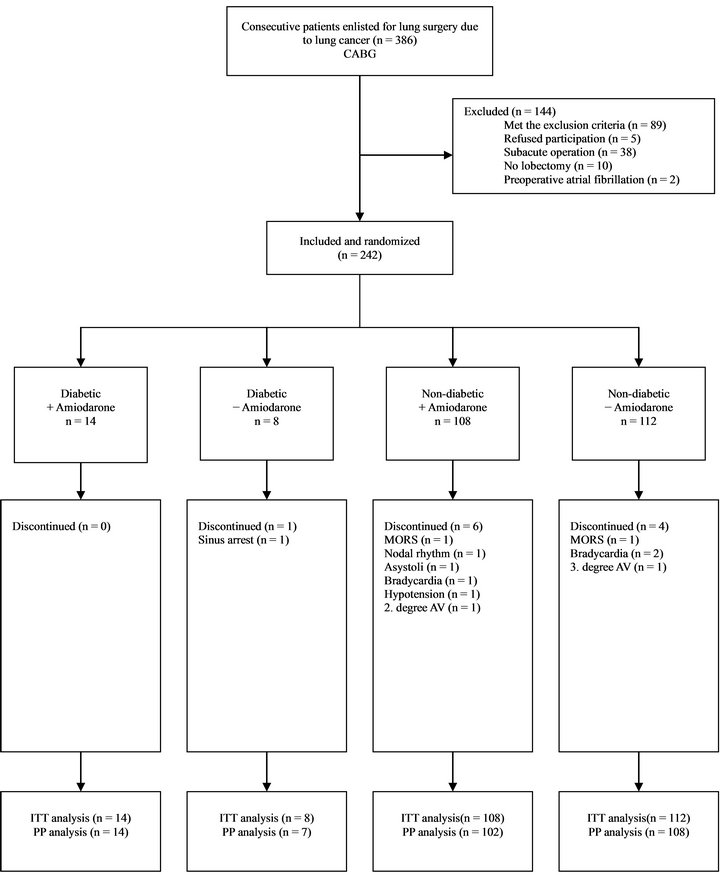
Figure 1. Flow chart.
Abbreviations: ITT = Intention-to-Treat; PP = Per Protocol; n = numbers.
were accounted as diabetics. Out of these 22 patients, 14 were in amiodarone prophylaxis (11%) and the remnant 8 patients received placebos (7%), why the randomization was acceptable (p = 0.26). This could be a contrib-
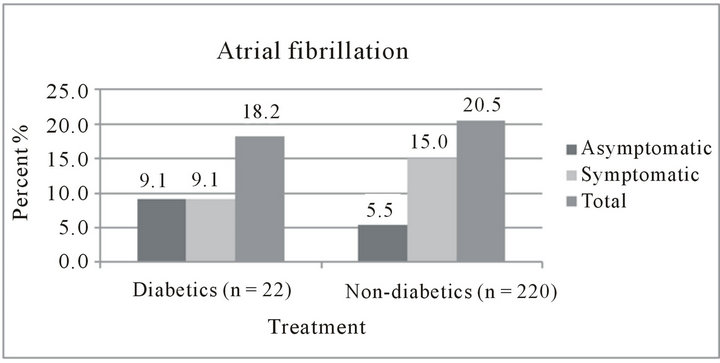
Figure 2. Distribution of atrial fibrillation in percent regarding diabetic status.
uting factor to the equal length of stays for diabetics and non-diabetics, as the group was too small to proper evaluate, if there was an enhanced risk of postoperative morbidity for diabetics. Further subgroup analyses were avoided due to the risk of multiple statistical testing errors. Furthermore diabetes was defined as receiving antidiabetic treatment at admission and not on the basis of blood samples. Therefore the actual number was underestimated, but probably equally underestimated in the two groups.
5. Conclusion
The prophylactic regime instituted is equally efficient for diabetics and non-diabetics in preventing postoperative atrial fibrillation after lung surgery. Diabetes is furthermore not associated with an increased risk of atrial fibrillation after lung surgery and the in-hospital length of stay is not altered in regards to diabetic status.
REFERENCES
- J. J. Curtis, B. M. Parker, C. A. McKenney, C. C. Wagner-Mann, J. T. Walls, T. L. Demmy and R. A. Schmaltz, “Incidence and Predictors of Supraventricular Dysrhythmias after Pulmonary Resection,” The Annals of Thoracic Surgery, Vol. 66, No. 5, 1998, pp. 1766-1771. doi:10.1016/S0003-4975(98)00942-4
- O. Rena, E. Papalia, A. Oliaro, C. Casadio, E. Ruffini, P. L. Filosso, C. Sacerdote and G. Maggi, “Supraventricular Arrhythmias after Resection Surgery of the Lung,” European Journal Cardio-Thoracic Surgery, Vol. 20, No. 4, 2001, pp. 688-693. doi:10.1016/S1010-7940(01)00890-9
- C. A. Polanczyk, L. Goldman, E. R. Marcantonio, E. J. Orav and T. H. Lee, “Supraventricular Arrhythmia in Patients Having Noncardiac Surgery: Clinical Correlates and Effect on Length of Stay,” Annals of Internal Medicine, Vol. 129, No. 4, 1998, pp. 279-285. doi:10.7326/0003-4819-129-4-199808150-00003
- P. Ciriaco, P. Mazzone, B. Canneto and P. Zannini, “Supraventricular Arrhythmia Following Lung Resection for Non-Small Cell Lung Cancer and Its Treatment with Amiodarone,” European Journal Cardio-Thoracic Surgery, Vol. 18, No. 1, 2000, pp. 12-16. doi:10.1016/S1010-7940(00)00428-0
- N. Barbetakis and M. Vassiliadis, “Is Amiodarone a Safe Antiarrhythmic to Use in Supraventricular Tachyarrhythmias after Lung Cancer Surgery?” BMC Surgery, Vol. 4, 2004, p. 7. doi:10.1186/1471-2482-4-7
- L. A. Lanza, A. L. Visbal, P. A. DeValeria, A. R. Zinsmeister, N. N. Diehl and V. F. Trastek, “Low-Dose Oral Amiodarone Prophylaxis Reduces Atrial Fibrillation after Pulmonary Resection,” The Annals of Thoracic Surgery, Vol. 75, No. 1, 2003, pp. 223-230. doi:10.1016/S0003-4975(02)04285-6
- L. P. Riber, T. D. Christensen, H. K. Jensen, A. Hoejsgaard and H. K. Pilegaard, “Amiodarone Significantly Decreases Atrial Fibrillation in Patients Undergoing Surgery for Lung Cancer,” The Annals of Thoracic Surgery, Vol. 94, No. 2, 2012, pp. 339-346. doi:10.1016/j.athoracsur.2011.12.096
- K. W. Garey, N. Kumar, T. Dao, V. H. Tam and L. O. Gentry, “Risk Factors for Postoperative Chest Wound Infections Due to Gram-Negative Bacteria in Cardiac Surgery Patients,” Journal of Chemotherapy, Vol. 18, No. 4, 2006, pp. 402-408.
- M. Jovanovic, J. Perovic and A. Grubor, “The Impact of Diabetes Mellitus on Postoperative Morbidity in Laryngeal Surgery,” Acta Chirurgica Iugoslavica, Vol. 53, No. 1, 2006, pp. 51-55. doi:10.2298/ACI0601051J
- A. Notzold, K. Michel, A. A. Khattab, H. H. Sievers and M. Huppe, “Diabetes Mellitus Increases Adverse Neurocognitive Outcome after Coronary Artery Bypass Grafting Surgery,” The Journal of Thoracic and Cardiovascular Surgery, Vol. 54, No. 5, 2006, pp. 307-312. doi:10.1055/s-2006-924089
- Y. Wang, Y. H. Liu, W. P. Zheng, Y. Ming and Z. Y. Shen, “Study on Risk Factors for Early Postoperative Infection after Orthotopic Liver Transplantation in Adults,” Chinese Critical Care Medicine, Vol. 18, No. 7, 2006, pp. 406-408.
- W. Jung, U. Meyerfeldt and R. Birkemeyer, “Atrial ArRhythmias after Cardiac Surgery in Patients with Diabetes Mellitus,” Clinical Research in Cardiology, vol. 95, Suppl. 1, 2006, pp. i88-i97. doi:10.1007/s00392-006-1120-1
- H. L. Lazar, S. R. Chipkin, C. A. Fitzgerald, Y. Bao, H. Cabral and C. S. Apstein, “Tight Glycemic Control in Diabetic Coronary Artery Bypass Graft Patients Improves Perioperative Outcomes and Decreases Recurrent Ischemic Events,” Circulation, Vol. 109, No. 12, 2004, pp. 1497- 1502. doi:10.1161/01.CIR.0000121747.71054.79
- L. R. Zebis, T. D. Christensen, H. F. Thomsen and V. E. Hjortdal, “Amiodarone Protects Diabetics and Non-Diabetics Undergoing Coronary Artery Bypass Grafting Equally,” Scandinavian Cardiovascular Journal, Vol. 42, No. 3, 2008, pp. 173-177. doi:10.1080/14017430701798820
- G. Eknoyan, “A History of Obesity, or How What Was Good Became Ugly and Then Bad,” Advances in Chronic Kidney Disease, Vol. 13, No. 4, 2006, pp. 421-427. doi:10.1053/j.ackd.2006.07.002
- P. A. Albertsson, R. Kohnke, S. C. Emek, J. Mei, J. F. Rehfeld, H. E. Akerlund and C. Erlanson-Albertsson, “Chloroplast Membranes Retard Fat Digestion and Induce Satiety: Effect of Biological Membranes on Pancreatic Lipase-Colipase,” Biochemical Journal, Vol. 401, No. 3, 2007, pp. 727-733. doi:10.1042/BJ20061463
- K. Makrilakis and N. Katsilambros, “Prediction and Prevention of Type 2 Diabetes,” Hormones (Athens), Vol. 2, No. 1, 2003, pp. 22-34.
- T. Gill, “Epidemiology and Health Impact of Obesity: An Asia Pacific Perspective,” Asia Pacific Journal of Clinical Nutrition, Vol. 15, 2006, pp. 3-14.
- J. P. Despres, “Intra-Abdominal Obesity: An Untreated Risk Factor for Type 2 Diabetes and Cardiovascular Disease,” Journal of Endocrinological Investigation, Vol. 29, Suppl. 3, 2006, pp. 77-82.
NOTES
*Corresponding author.

