Open Journal of Nursing
Vol.3 No.2(2013), Article ID:32471,7 pages DOI:10.4236/ojn.2013.32027
Development of ethical dilemma scale Japanese nurse faced physical restraints to elderly patients with dementia
![]()
Department of Nursing, Kyoto Koka Women’s University, Kyoto, Japan
Email: tokiwa27@hotmail.com
Copyright © 2013 Miwa Yamamoto et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received 25 January 2013; revised 26 February 2013; accepted 15 April 2013
Keywords: Ethical Dilemma Scale; Japanese Nurse; Physical Restraints; Elderly Patients with Dementia
ABSTRACT
Purpose: This study aimed to develop an ethical dilemma scale for nurses faced with the use of physical restraint when caring for elderly patients with dementia. Methods: We used a previously established 20-item dilemma scale. The objective and method of the study were explained to the head of nursing at 17 selected hospitals, and 121 nurses working in the general wards of 14 hospitals (excluding emergency department wards of psychiatry, pediatrics, obstetrics, outpatients, operating rooms and intensive care units) who agreed to participate were enrolled in 2000. Seventy-six nurses from one of the hospitals were selected after eight years (2008) to provide a comparison. Ethical considerations: The study was conducted with the approval of the ethics committee at Meiji University of Integrative Medicine. Results and discussion: Four factors were compared between 2000 and 2008: “execution of treatment and security”, “characteristic features in nursing of elderly patients with dementia”, “cooperative relationship in nursing”, and “priorities in nursing”. The cumulative contribution ratio was 65.3% (KMO = 0.77, p = 0.000) in 2000 and 72.5% (KMO = 0.78, p = 0.000) in 2008. Therefore, the scale dilemma nurse faced physical restraints to elderly patients with dementia in Japan was developed 4 facoters from 17-delremmas items of 20 items.
1. INTRODUCTION
In 2000, Japan established a long-term care insurance system in response to societal concern regarding the aging population and their care. The system ensured asneeded care and support by the society as a whole for elderly Japanese citizens. Long-term care insurance is separate from medical care insurance, and was set up as a first step toward revising the structure of social security.
The Ministry of Health, Labour and Welfare passed a bill prohibiting physical restraint of elderly patients receiving treatment under the long-term care insurance program. As a result, those caring for elderly patients at various institutions were legally prohibited from using physical restraint. Nonetheless, at many general hospitals in Japan, physical restraint is not illegal when treating patients under medical care insurance schemes. In Japan, nursing care continues to include the practice of physical restraint of patients [1], partly due to a lack of effective alternative practices in many general wards, where the use of physical restraint is not specifically prohibited. Physical restraint of patients with dementia is unlikely to end soon, in the absence of alternative nursing care techniques to ensure the safety of senile older people with dementia. A patient with dementia hospitalised in a general hospital differs from a senior citizen who enters an institution for medical care. Extra care is necessary for patients with dementia as they may, for example, remove intravenous infusion tubes. As a result, nurses in many countries including Japan often use physical restraint during the course of treatment [2].
While the motivation for the use of restraint is the welfare of the patient, several studies have demonstrated that physical restraint can instead cause undue harm [3- 6]. The possibility of restraint-related injury and the legislated non-use of physical restraint in Japanese patients under long-term care have created an ethical dilemma for nurses [7,8]. The challenges and conflicting feelings faced by nurses in restraining elderly patients with dementia [9] can cause nurses to question their abilities to deliver high-quality care. The resulting stress, anxiety and indecision may cloud their clinical judgement. Moreover, the causes of dementia remain unclear, and no effective treatment or cure is available. Yet, healthcare needs of the elderly with dementia are changing, and are made worse with increasing age. This has created difficulties in caring for such patients in hospitals in Japan. At the same time, greater societal awareness of the plight of elderly patients with dementia has placed increased emphasis on delivering high-quality and efficient care to these patients. Nurses, as front-line providers of healthcare, are under enormous pressure to deliver effective and humane service [8]. Particularly in general wards, nurses are likely to experience ethical challenges when caring for people with dementia.
2. OBJECTIVE
The purpose of this study was to develop an ethical dilemma scale based on the experience of nurses working in general wards who face decisions regarding physical restraint of elderly patients with dementia.
3. DEFINITION OF TERMS
3.1. Ethical Dilemma
Ethical dilemma is a situation in which one must choose between two or more equally unsatisfactory choices. Ethical dilemma has been defined as a situation with conflict between two or more ethical principles, for which each solution may contain unpleasant outcomes for one or more of the involved parties [10]. We defined dilemma in the context of restraining elderly patients as mixed feelings created in the nurses when they cannot arrive at a clear answer in the situation and where the basic responsibilities of nursing result in a conflict of whether or not to use restraint on an elderly patient while nursing at a clinical site.
3.2. Elderly People with Dementia
Elderly people who are hospitalized in general wards presenting with dementia symptoms as recognized by nurses. There is often no guarantee that dementia be diagnosed by a physician.
4. METHODS
4.1. Participants
The degree to which an individual experiences a dilemma differs from person-to-person and is influenced by factors including educational background, nursing and personal life experiences and personal sense of values [10- 12]. The selection of subjects was carried out by the purposeful selection at 17 community hospitals in the midwestern region of Japan. The subjects were registered nurses working at these hospitals. Inclusion criteria for the hospitals were: 1) presence of an independent nursing division or department under nursing management; 2)
policy of continuous training programs for nurses; 3) similar employment conditions for nurses; and 4) identity as a general hospital. The objective and method of the study were explained to the head of nursing in the 17 selected hospitals, and 121 nurses working in general wards (excluding emergency department wards of psychiatry, paediatrics, obstetrics, outpatients, operating rooms and intensive care units) at 14 hospitals, who agreed to take part in the study, were enrolled in 2000.
Participants from one hospital were selected eight years later (2008) to provide a comparison. The participants included 76 nurses at general wards (with the same aforementioned exclusions). We assessed dilemmas in these participants using a 20-item questionnaire previously developed by the author based on dilemma items (a low score of 1 - 5 points suggested that nurses experienced dilemma) [8,13].
4.2. Conceptual Framework
The conceptual framework of this study was based upon the MORAL (M = Massage the Dilemma, O = Outline Options, R = Review Criteria and Resolve, A = Affirm Position and Act and L = Look Back) model [11,12] schemata for describing relationships among constructs, concepts, and measurement tools (referents) relevant to a research question. The MORAL model facilitates the understanding of coping with ethical dilemmas. The aspects of the model are described in more detail below.
Massage the dilemma: The first step involves developing a full understanding of the ethical conflict after gathering significant information about the situation. This process includes recognising whose interests are involved, defining the dilemma and describing conflicting loyalties.
Outline options: Nurses who understand the dilemma recognise the conflict involved in the situation. After recognising the conflict, a nurse can then consider how to solve the problem. Review Criteria and Resolve: The third step in the model aims to identify moral criteria and then define a course of action most congruent with those criteria. This step is crucial to making a moral judgment that will resolve the dilemma. To complete this step of the model, examination of moral principles is essential, and it is ideal that a nurse has ample experience in nursing and philosophy.
Affirm Position and Act: The first three steps of the model result in a moral judgment. This step involves putting the knowledge into action. While developing a moral judgment is the essential preparation for moral action, this alone is insufficient to follow through with the process of the model. A decision-making grid, with actions listed by criteria, may be useful in diagramming this key choice.
Look back: In this step, nurses reflect on their perception of the ethical conflict, resourcefulness in generating options, clarification of moral criteria and assessment of options by these criteria. Their solution to the ethical dilemma brings new insights.
M clarifies the most recurrent ethical dilemmas in a practice. O includes assessing the nature and adequacy of the alternative strategies. R involves reviewing basic moral principles. Thus, the MORAL model provides an ethical decision-making process enabling nurses to respond to ethical dilemmas in their own practice.
An important aspect of the theoretical framework is the conceptualisation of the term dilemma. The conceptual framework of this study was based upon the MORAL model described by Crisham [11]. We assumed that nurses experienced a dilemma when faced with the decision to restrain an elderly patient and that situations requiring the use of restraint would arise. Areas of dilemma were practice of nursing, cooperative relationship in nursing, execution of treatment and security, individual value system of the nurse, and nursing duties involving elderly patients with dementia. The study was performed using an independently prepared, 20-item questionnaire based on prior studies [8,11,12] as a reference for nursing dilemma items [14]. We assigned each item to the area of best fit. This yielded 20 items, with five areas each receiving four items. It was further assumed that dilemmas could be measured using a five-point Likert scale, with a higher score indicating the likelihood that nurses would have mixed feelings. Internal consistency and reliability of the constructed dilemma items were examined using Cronbach’s α coefficient with the criterion set at a coefficient of >0.6. Construction validity was assessed using factor analysis. Internal consistency of the 20 independently prepared items used to measure dilemmas was tested and had a Cronbach’s α coefficient value of 0.87 (Table 1).
Request sheets disclosing the objective of the study,
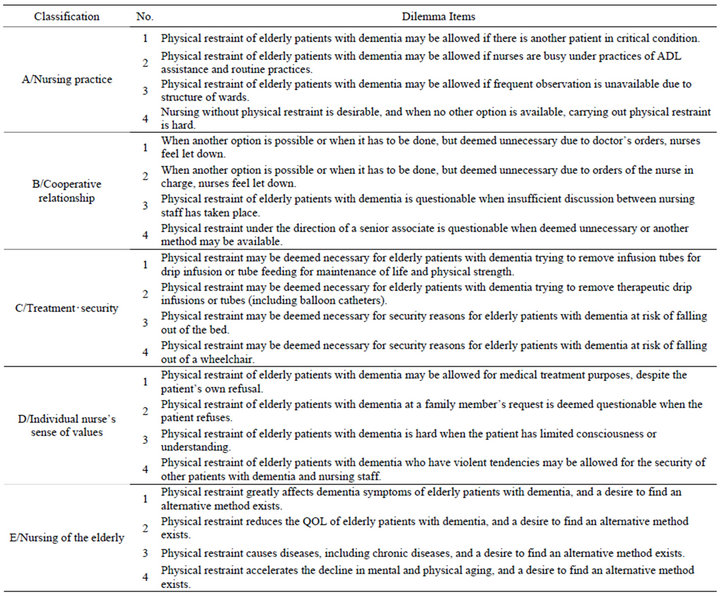
Table 1. 20 dilemma items.
methods of distribution and retrieval of questionnaires and addresses of the investigators were distributed. Alternatively, investigators were interviewed. Details of the study were explained to the head of nursing in the targeted hospitals/wards. A request sheet defining the terms physical restraint and elderly patients, explaining how to fill out the questionnaires, the period of response and the objective of the present study was sent to individual nurses. Addresses of the investigators were also enclosed to help facilitate understanding of the study by nurses. A preliminary survey was carried out with 10 nurses working in orthopedic surgery wards in community hospitals (general hospitals with 400 beds) and the obtained results were used to improve the questionnaire. The resulting revised questionnaire was used in this study.
4.3. Ethical Considerations
The questionnaire was designed to ensure privacy and anonymity, while allowing participants to complete the form themselves. Participants inserted and sealed the completed questionnaire into an envelope that was provided in advance. The study was conducted with the approval of the ethics committee at Meiji University of Integrative Medicine.
4.4. Statistical Analysis
The factor structure was confirmed after exploratory factor analysis (maximum likelihood method: promax rotation) to assess construct validity. The criteria of sample validity for the factor analysis aimed at a Kiser-MeyerOlkin measure value of >0.6 and a cumulative contribution ratio of >60.0% [15]. The inclusion of items was applied to a factor loading of >0.4 without any difficulty in interpretation.
5. RESULTS
5.1. Reliability and Validity of 20 Dilemma Items
The internal consistency of the 20 independently prepared items of stress was tested with Cronbach’s coefficient. A value of 0.78 (excluding no answer; n = 121) was obtained. The correlation coefficient for 15 of 20 items was low (0.2 - 0.3), indicating independent responses, and a negligible change in the coefficient was found, regardless of the deletion of any single item.
5.2. Validity of Item Selection and Dilemma Factors
The items were subjected to a factor analysis (maximum likelihood method: promax rotation) for the clarification of the dilemma factors. The four dilemma factors were: “execution of treatment and security”, “characteristic features in nursing of elderly patients with dementia”, “cooperative relationship in nursing” and “priorities in nursing”. The cumulative contribution ratio in 2000 and 2008 was 65.3% (KMO = 0.77, p = 0.000) (Table 2) and 72.5% (KMO = 0.78, p = 0.000) (Table 3), respectively.
5.3. Interpretation of Each Extracted Factor
“Execution of treatment and security” accounted for 28.2% of the cumulative variance. Most items were related to dilemmas occurring in the treatment practises and the security of elderly patients while executing treatment. “Characteristic features in nursing of elderly patients with dementia” accounted for 49.6% of the cumulative variance and was composed of items expressing characteristic features in the practical nursing of elderly patients. “Cooperative relationship in nursing” accounted for 60.6% of the cumulative variance and was composed of items considered to express dilemmas with staff members in nursing. “Priorities in nursing” accounted for 68.3% of the cumulative variance and was composed of items related to dilemmas in trying to smoothly carry out duties for the elderly, among patients of various ages.
6. DISCUSSION
Cronbach’s overall coefficient for the 20 items of dilemma was high (0.78) and the factor analysis extracted four dilemma factors as having a characteristic value of 1 (Kaiser-Meyer-Olkin measure value = 0.81) with a cumulative contribution ratio of 68.3%. The high Cronbach’s values for these items (0.85, 0.87, 0.87 and 0.81) confirmed the internal consistencies. The four ethical dilemma factors—treatment and security, nursing the elderly, cooperative relationship and priorities in nursing —are serious dilemmas faced by nurses in decision regarding the use of physical restraint of elderly patients. These findings provide greater understanding of the needs for immediate countermeasures. Each item is considered in more detail below.
Execution of treatment and security: Practising nurses are expected to secure the elderly patients, but they are also expected to follow physicians’ orders even though they feel that physical restraint might cause harm to the elderly. The strategy for this could be that the nurses should communicate with their medical colleagues, discuss patients’ care and reach a consensus. In addition, the nurses should explore alternatives to restraint devices.
Characteristics in nursing of elderly patients with dementia: Although nurses try to avoid restraining elderly patients as much as possible, they may still believe that the elderly should be restrained to protect them from falling and hurting themselves. The implication for this is to allocate elderly care specialists in each ward. Conse-
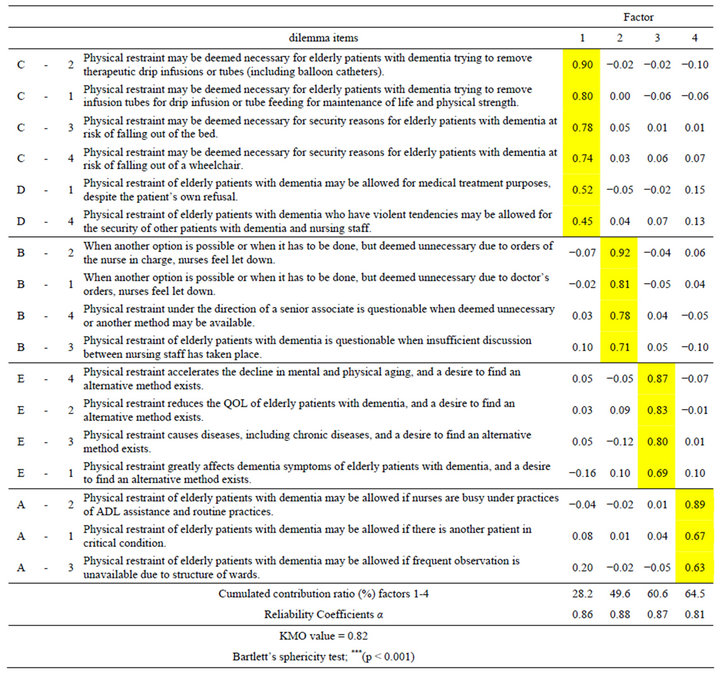
Table 2. Factore analysis of nurses’s dilemma for pyhsical restrainted elderly patientes with dementia in 2000.
quently, the nurses might acquire skills to care for the elderly without restraint.
Cooperative relationship in nursing practise: Practising nurses are responsible for clinical decision-making, but they have substantially less authority than physicians to assist patients. Nurse administrators should be sensitive to the quality patient care regarding physical restraints and should understand the situations in which nurses experience a dilemma in the use of physical restraint. A strategy to assist nurses is to ensure the existence and use of institutional policies and safety standards. Toward this end, the administrators might need to arrange for the health-care organization to be objectively evaluated.
Priorities in nursing: When nurses take more time to care for acutely ill patients than for elderly patients, they are likely to think that the use of physical restraints for the elderly is needed. This might mean that the nurses are upholding their individual code of ethics or that they are required to choose the institutional polices. In either case, the nurses might report their feelings of confusion or uncertainty. Continuing education helps nurses to improve their skills in making ethical decisions. The most important component of a relevant educational program is that nurses can recognize the ethically difficult situation in which they are involved. Therefore, the construction and implementation of the countermeasures addressing these four factors are recommended to cope with
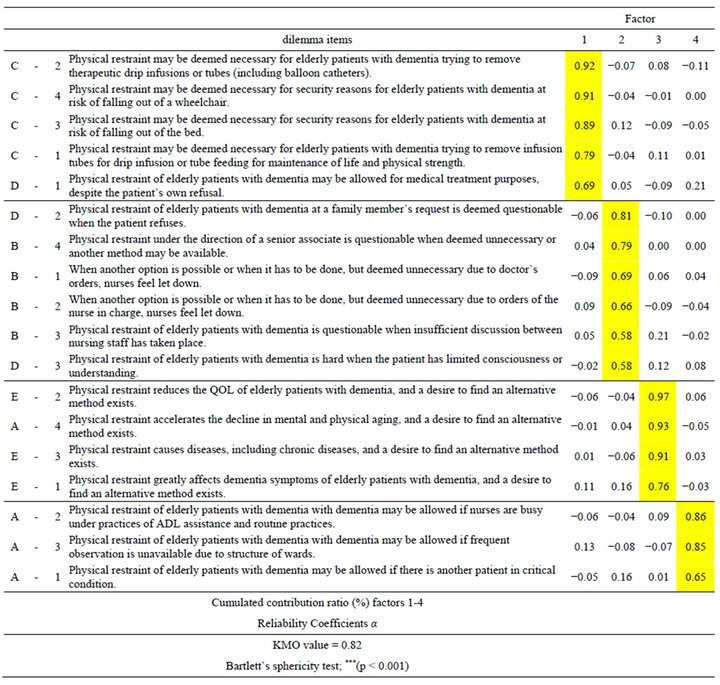
Table 3. Factore analysis of nurses’ dilemma for pyhsical restrainted elderly patients with dementia in 2008.
nurses’ dilemmas.
Our results echo the findings from studies on dilemmas nurses face in all clinical fields [16,17] and might be common to nurses working in general wards. However, concerning the second dilemma factor, “characteristics in nursing of elderly patients with dementia”, similar findings have been reported in nurses caring for adult and acute-phase patients in the general ward setting.
Practising nurses are expected to behave in a moral manner on a daily basis, but they continue to report ethical confusion and uncertainty regarding restraint of the elderly in the general ward. We suggest that addressing aforementioned four factors would help nurses better cope with these dilemmas, for example, by dialoguing with their medical colleagues to share judgments and attitude toward the use of physical restraint for elderly people. Having a dialogue, even in the setting of a conference, is not costly and can be implemented immedi ately.
The results of the present study highlight the need for further consideration into nursing for patients with dementia, as being faced with dilemmas on a daily basis is not a favourable working environment for nurses. Concerning the use of physical restraint, nurses should carefully reconsider the customary use of this practice on the elderly, not merely to diffuse their feelings of dilemma but as a means of actively improving the quality of care and quality of life of the elderly patients. Few studies have been carried out in Japan to examine the conscience of nurses regarding physical restraint of elderly patients. Ethical dilemmas are likely to be influenced by many factors that may wax and wane over time.
There were several limitations to this study. The present study did not examine factors that could influence an individual nurse’s sense of value or individual experiences and attributes, such as educational background, religious affiliation, nursing experience and gender [10]. In addition, the questionnaires were completed only once during the study period. A detailed analysis of changes in conscience over time remains one of the problems to be investigated in the future. In addition, we need to consider that the questionnaires were analysed without regard to gender (gender differences were hard to assess, given the very small number of male participants). Despite these limitations, the results of this research are useful in coping with dilemmas regarding the use of restraint for elderly patients with dementia.
In summary, an ethical dilemma scale for nurses faced with the use of physical restraint when caring for elderly patients with dementia in Japan was developed, which revealed four important factors from 17 of 20 dilemma items.
REFERENCES
- Ujiie, S. (2005) Shintaiteki yokusei [Physical restraints]. 6th, Edition, Igaku Syoin, Yokiyo.
- Hamers, J.P. and Huizing, A.R. (2005) Why do we use physical restraints in the elderly? Zeitschrift für Gerontologie und Geriatrie, 38, 19-25. doi:10.1007/s00391-005-0286-xdoi:10.1007/s00391-005-0286-x
- Catchen, H. (1983) Repeaters: Inpatient accidents among the hospitalized elderly. Gerontologist, 23, 273-276. doi:10.1093/geront/23.3.273
- Evans, L. (1990) Restraint effectiveness, occupant ejection from cars, and fatality reductions. Accident Analysis & Prevention, 22, 167-175. doi:10.1016/0001-4575(90)90067-U
- Burton, L.C., et al. (1992) Physical restraint use and cognitive decline among nursing home residents. Journal of the American Geriatrics Society, 40, 811-816.
- Parker, K. and Miles S.H. (1997) Deaths caused by bedrails. Journal of the American Geriatrics Society, 45, 797- 802.
- Scherer, Y.K., et al. (1991) The nursing dilemma of restraints. Journal of Gerontological Nursingm, 17, 14-17.
- Yamamoto, M., Izumi, K. and Usui K. (2006) Dilemmas facing Japanese nurses regarding the physical restraint of elderly patients. Japan Journal of Nursing Science, 3, 43-50. doi:10.1111/j.1742-7924.2006.00056.x
- Evans, L.K. and Cotter, V.T. (2008) Avoiding restraints in patients with dementia: Understanding, prevention, and management are the keys. The American Journal of Nursing, 108, 40-49. doi:10.1097/01.NAJ.0000311827.75816.8b
- Ham, K. (2004) Principled thinking: A comparison of nursing students and experienced nurses. Journal of Continuing Education in Nursing, 35, 66-73.
- Crisham, P. (1985) Moral: How can I do what’s right? Nursing Management, 16, 42A-42N. doi:10.1097/00006247-198503000-00006
- Crisham, P. (1981) Measuring moral judgment in nursing dilemmas. Nursing Research, 30, 104-110. doi:10.1097/00006199-198103000-00012
- International Council of Nurses (ICN) (1974) International Council of Nurses: Code for nurses. ANEC, 5, 32- 33.
- Kojima, M. (1997) Mapping for management of dilemmas of nurses—Communication with doctors for nursing focused on patients. Igaku Syoin, Tokyo.
- Ishimura, S. (2001) Dictionary of statistics. Tkyou Tosyo, Tokyo.
- Fry, S.T. (1982) Ethical principles in nursing education and practice: A missing link in the unification issue. Nursing and Health Care, 3, 363-368.
- Barbara, L. Tate (1977) International Council of Nurses, Geneva, Switzerland: The nurse’s dilemma—Ethical considerations in nursing practice, USA, 1977. In: ICN, Ed., by Katsuko Kodama, Japanese Nursing Association, Div. of Publishing, Tokyo, 1977.

