Open Journal of Obstetrics and Gynecology
Vol.4 No.1(2014), Article ID:41829,9 pages DOI:10.4236/ojog.2014.41007
Comparative study for success rate of vaginal birth after cesarean section following labor induction by two forms of vaginal dinosprostone: A pilot study
1Lecturer of Obstetrics and Gynecology, Faculty of Medicine, Ain-Shams University, Cairo, Egypt
2Assistant Professor in Obstetrics and Gynecology, Faculty of Medicine, Ain-Shams University, Cairo, Egypt
Email: *mahmoudfathy74@yahoo.com
Copyright © 2014 Mahmoud Fathy Hassan, Osama El-Tohamy. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. In accordance of the Creative Commons Attribution License all Copyrights © 2014 are reserved for SCIRP and the owner of the intellectual property Mahmoud Fathy Hassan, Osama El-Tohamy. All Copyright © 2014 are guarded by law and by SCIRP as a guardian.
Received 13 December 2013; revised 4 January 2014; accepted 10 January 2014
ABSTRACT
Background: Cesarean delivery has become the most common major surgical procedure in many parts of the world. Induction of labor in women with prior cesarean delivery is an alternative to mitigate the rising cesarean rates. Objectives: To compare the VBAC success rate between two vaginal forms of dinoprostone for labor induction in women with prior cesarean section. Material and Methods: A pilot study was conducted at a large Governmental Hospital, Dhahran, Saudi Arabia, including 200 women with prior cesarean section and planned for labor induction. Participants were randomly allocated into two groups. Group A (n = 100) received dinoprostone 1.5 mg vaginal tablet. Group B (n = 100) received 10 mg dinoprostone sustained release vaginal pessary. Primary outcome was vaginal delivery rate. Secondary outcomes included maternal and neonatal outcomes. Results: The dinoprostone vaginal tablet and dinoprostone vaginal pessary had a comparable vaginal delivery rate (67% and 64%, respectively; p = 0.78). The median patient satisfaction with the birth process was superior in the dinoprostone vaginal pessary group (p = 0.04). Maternal and neonatal outcomes were similar in both groups. Conclusion: Both forms of dinoprostone were effective methods for labor induction in women with prior cesarean section. However, the patient satisfaction with the birth process was in favor of the dinoprostone sustained release vaginal pessary.
KEYWORDS
Dinoprostone; Induction of Labor; Trial of Labor after Cesarean; TOLAC; Vaginal Birth after Cesarean; VBAC
1. INTRODUCTION
Cesarean section has become the most common major surgical intervention in various portions of the world [1]. Cesarean delivery rates greater than those suggested by the World Health Organization (WHO) have been reported in most parts of the world including developing countries [2]. It is well recognized that the hazards of cesarean delivery for women rise with increasing amounts of cesarean sections. These involve possibly life-threatening complications including hemorrhage, surgical complications and morbidly adherent placenta [3,4]. Vaginal birth after cesarean section (VBAC) is settled from the 1980 National Institutes of Health (NIH) Consensus Conference on Cesarean as a tool to minimize the cesarean delivery rate [5]. The present medical studies show that 60% - 80% of women can attain successful trial of labor after a previous cesarean section [6].
With the rates of cesarean delivery and labor induction on the rise, [5] physicians frequently encounter the problem of whether or not to induce labor in a patient with a prior cesarean delivery. Although VBAC in women with formerly one low transverse cesarean section was considered safe, the threat of uterine rupture associated with labor induction can be amplified [7]. With labor induction in a previous cesarean section, the uterine rupture can be a grave event that can threaten the life and the neurological status of the baby and end in major uterine bleeding which may require a hysterectomy [8]. Many people estimate the risk of uterine rupture in women with previous cesarean section during a trial of labor as ≤1%, [9,10] but the risk may rise to as high as 2% - 3% with labor induction [11]. The elevated risk of uterine rupture has not been linked to a single inducing agent. Actually, studies in literature are contradictory whether or not prostaglandins are independently related to uterine rupture [9-12]. Many studies suggest no further probability to have a cesarean delivery or a uterine rupture in women who experienced labor induction than their spontaneously laboring women [13-15]. As well, the balance between the probable adverse consequences of labor induction in women with a prior cesarean versus the short and long-term complications connected with routine elective cesarean delivery is undefined [16].
The externally provided prostaglandins are effective at the cervical ripening and they hasten the delivery, but they elevate the risk of the uterine hyperstimulation and produce fetal heart rate changes [17]. A sustained release vaginal pessary releases a continuous and expectable dose of dinoprostone at a rate of nearly 0.3 mg/hour for 24 hours [18]. The sustained release formulation of dinoprostone diminishes the risk of uterine hyperstimulation and can be extracted rapidly when labor begins, or in the event of an adverse reaction. In addition, the progressive cervical ripening induced by the sustained release dinoprostone may be more tolerable to patients than the quick onset of contractions observed with other dinoprostone forms [19]. The sustained release dinoprostone vaginal pessary remains for up to 24 hours allowing longer induction, if required, with only solitary application [18].
In the present study, we conducted a pilot study to evaluate the efficiency of two different forms of vaginal prostaglandins E2 (dinoprostone 1.5 mg vaginal tablets and 10 mg dinoprostone sustained release vaginal pessary) for labor induction among women with a history of prior cesarean section.
2. MATERIAL AND METHODS
The present study was carried out at the Department of Obstetrics and Gynecology of a large Governmental Hospital, Dhahran, Saudi Arabia, from February 2009 till March 2013. The study protocol was approved by the Hospital Research and Ethical Committee. This trial was performed in compliance with the Declaration of Helsinki.
Being a pilot study, sample size calculation was not required. Women with a live singleton term fetus (37 - 42 weeks of gestation, as determined by the last menstrual period or by a first or second-trimester ultrasound scan) in cephalic presentation and a reactive non-stress test, who presented with a Bishop score of ≤ 7 before the onset of labor, and with no spontaneous contractions (<4 contractions within 20 minutes) were included. Women in active labor or with uterine surgery other than lower segment cesarean section, ruptured membranes, chorioamnionitis, antepartum hemorrhage, contraindication to prostaglandins use (e.g., bronchial asthma or glaucoma), contraindication to vaginal delivery, nonvertex presentation, multiple pregnancy, major fetal anomalies or demise were excluded.
Women who fulfilled the appropriate criteria were invited to participate in the study, and those who agreed provided a written informed consent. This study included 200 women with prior cesarean section and planned for labor induction. The women included in this study were randomly allocated into two equal groups. Group A included 100 women received dinoprostone 1.5 mg vaginal tablet for labor induction, and group B included 100 women received dinoprostone 10 mg sustained release vaginal pessary. The study was open labeled; thus, women and clinicians were aware of the treatment allocation scheme.
Demographic background data and obstetric history were obtained from all participating women immediately before labor induction. Sterile vaginal examination was done to ascertain the Bishop score. Ultrasound was done to assess fetal growth parameters, amniotic fluid index, and placental location. External cardiotocography (CTG) was performed to assess fetal well-being and to confirm the absence of uterine contractions.
Patients in group A received 1.5 mg dinoprostone vaginal tablet (Prostin E2®; Pharmacia & Upjohn, Puurs, Belgium) into the posterior vaginal fornix for a maximum of three doses with 6 hourly intervals. Before application of each dose, vaginal examination to ascertain the Bishop score and CTG was performed to assess fetal well-being and frequency of uterine contractions. Patients in group B received a single dose of dinoprostone 10 mg sustained release vaginal pessary (Propess®; Controlled Therapeutics (Scotland) Ltd., East Kilbride, UK) into the posterior vaginal fornix. The dinoprostone pessary releases at a steady rate (0.3 mg/h). It remained in the vagina for up to 24 hours, as recommended by the manufacturer. It was removed if it was still present 24 hours after placement, if a worrisome fetal heart rate (FHR) pattern persisted, or if the patient had efficient uterine contractions (3 - 4 contractions in 10 minutes). Whenever any patient in both groups had a Bishop score ≥ 8 or passed into active labor, she was started the active management of labor 6 hours after placement the last dinoprostone vaginal tablet or removal of the dinoprostonesustained release vaginal pessary. Active labor was defined as at least three firm, rhythmic uterine contractions with duration at least 45 seconds occurring within a 10- minute period, or achievement of 4 cm dilatation. Active management of labor included amniotomy followed by intravenous oxytocin after 2 hours if no efficient uterine contractions. An initial dose of 2 mU/ min was increased by 2 mU/min at 30 minute intervals to a maximum dose of 16mU/min or until 3 - 4 contractions in 10 minutes were achieved. Once started, oxytocin infusion was continued to delivery unless otherwise indicated. All women were monitored for maternal pulse, blood pressure, temperature, and respiratory rate. FHR was monitored by continuous CTG. Vaginal examination was done at 2 - 4 hours intervals to assess the progress of labor. Cervical dilatation, station, and position were noted at each examination.
Uterine rupture was clearly defined a priori as a fullthickness disruption of the uterine wall accompanied by at least one of the following clinical signs: non-reassuring fetal heart rate tracing immediately prior to surgery, hemoperitoneum, or any sign of maternal hemorrhage (systolic blood pressure <70 mm Hg, diastolic blood pressure <40 mm Hg, or heart rate >120 beats/min). This definition was used to distinguish a clinically significant uterine rupture from an asymptomatic or incidental finding of uterine scar separation or “uterine window” [10]. Uterine hypertonus was defined as one contraction lasted more than 2 minutes, uterine tachysystole was defined as >5 contractions of moderate to severe intensity per 10 minutes, and hyperstimulation syndrome as the presence of non-reassuring FHR tracing combined with either tachysystole or hypertonus [20].
The primary outcome measures were the vaginal delivery rate. Secondary outcomes were induction to delivery time, maternal satisfaction score for the birth process obtained within 24 hours of delivery (a visual analogue scale [VAS] of 0 - 10, with greater score denoting better satisfaction), maternal and neonatal complications. Maternal complications included uterine tachysystole, uterine hypertonus, uterine hyperstimulation, blood loss, blood transfusion, uterine rupture, fever or chorioamnionitisand postpartum endometritis (defined as temperature ≥ 38˚C accompanied by uterine tenderness and/or purulent or foul-smelling lochia beyond the first 24 hours after delivery). Neonatal complications noted were Apgar scores of <7 at 5 minutes, High cord blood base deficit ≥12, low umbilical artery pH < 7.1, birth asphyxia (Criteria for birth asphyxia were arterial cord pH < 7.1, Base deficit ≤12, Apgar score <4 at 5 minutes, neonatal convulsions, coma or brain insult documented with imaging) [21] and admission to the Neonatal Intensive Care Unit (NICU). All cardiotocograms were reviewed by the author to identify and classify abnormal patterns. There is no standard definition for what constitutes failed labor induction. Here, we defined failed induction of labor as when the patient had Bishop Score ≤ 5 after 12 hours of last dinoprostone 1.5 mg vaginal tablet or 24 hours after insertion of dinoprostone sustained release vaginal pessary. The decision to perform a cesarean delivery was made based on our usual obstetric practice, and the indication for the cesarean section was recorded (failed induction of labor, failure to progress in established labor, or non-reassuring fetal status [based on FHR patterns]).
Statistical analysis was done using the SPSS (Statistical package of Social Sciences) for Windows version 14 (SPSS Inc., Chicago, IL). Analysis was done by intention to treat. Normal distribution of continuous variables was assessed by the Kolmogorov-Smirnov test. The Fisher exact test was used for analysis of categorical variables and data were presented as number (%). Unpaired student t test was used for normally distributed continuous variables and data were presented as mean ± standard deviation, while the non-normally distributed variables were compared by the Mann-Whitney U test and data were presented as median (range). Two tailed P value < 0.05 was considered to indicate statistical significance.
3. RESULTS
In total, 271 women were recruited in this study. Seventy one women declined from the study as they were not meeting the criteria for inclusion (n = 29) or refusing induction of labor (n = 42). Two hundred women were randomly allocated to induction of labor with dinoprostone 1.5 mg vaginal tablet (n = 100) or dinoprostone sustained release vaginal pessary (n = 100).
Table 1 revealed that maternal demographic and obstetric characteristics in both groups were similar. No statistical difference was found in maternal age, body mass index (BMI), gestational age, parity, prior vaginal delivery, pre-induction Bishop Score. Likewise, patients had similar indications for labor induction.
Maternal outcomes were shown in Table 2. The delivery method did not differ significantly between both groups, with cesareans performed in 33 women (33%) in the dinoprostone 1.5 mg group compared with 36 women (36%) in the sustained release dinoprostone group (P = 0.78). The indications for cesarean delivery were similar between the two groups. No maternal or neonatal deaths occurred during the study, and no adverse events led to premature withdrawal of any participants from the study. In both groups of women treated with the dinoprostone 1.5 mg and the 10 mg sustained release dinoprostone, the induction to delivery time was similar (19.3 ± 4.6, 19.5 ± 5.2, respectively; p = 0.72). The frequency of non-reassuring FHR patterns occurring at any time during labor that prompts intervention was not statistically different between both groups. Non-reassuring FHR patterns were the most common indication for cesarean birth. It occurred in 14 cases (42.4%), and 12 cases (33.3%) of par-
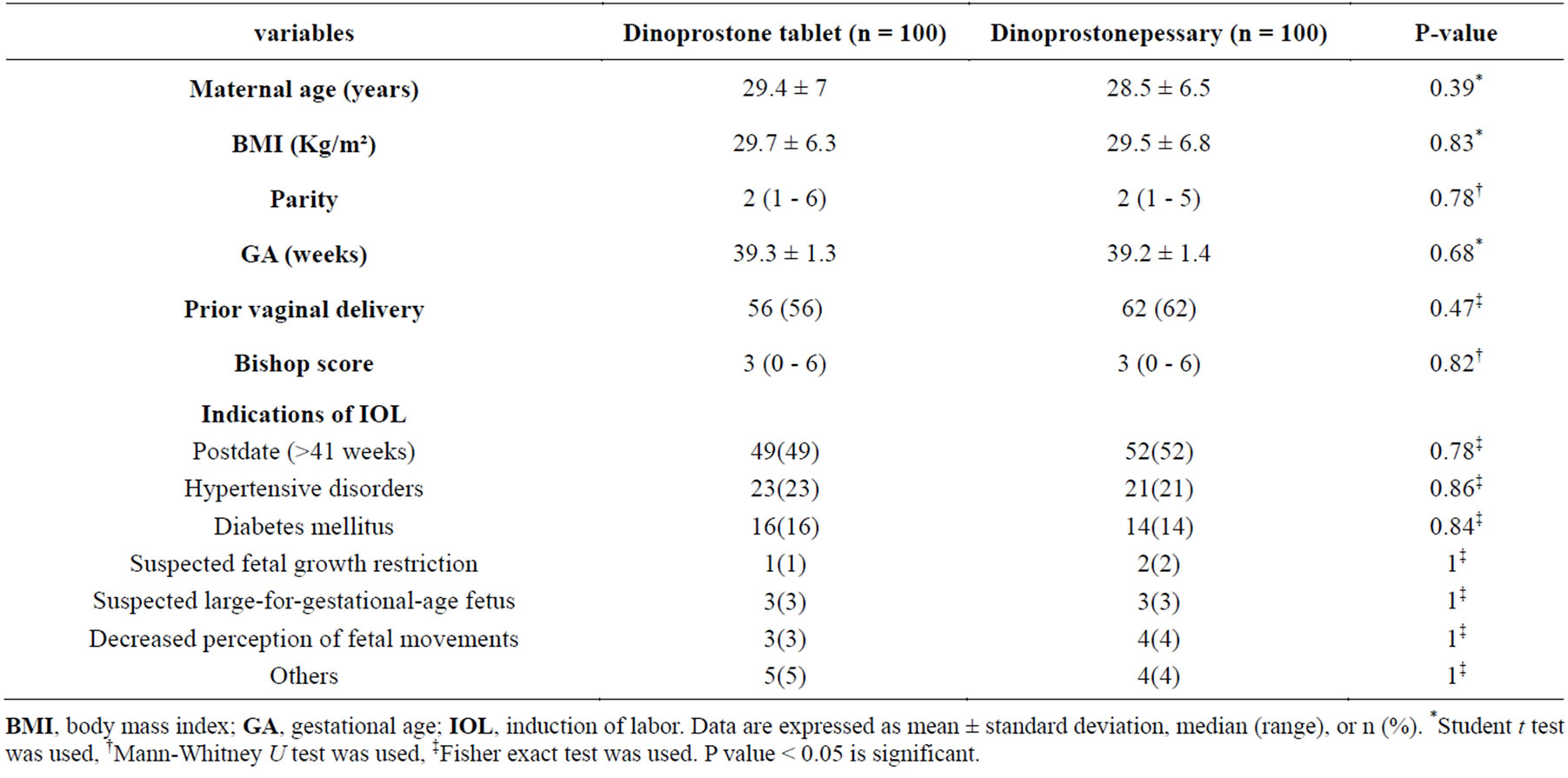
Table 1. Baseline characteristics of participants.
BMI, body mass index; GA, gestational age; IOL, induction of labor. Data are expressed as mean ± standard deviation, median (range), or n (%). *Student t test was used, †Mann-Whitney U test was used, ‡Fisher exact test was used. P value < 0.05 is significant.
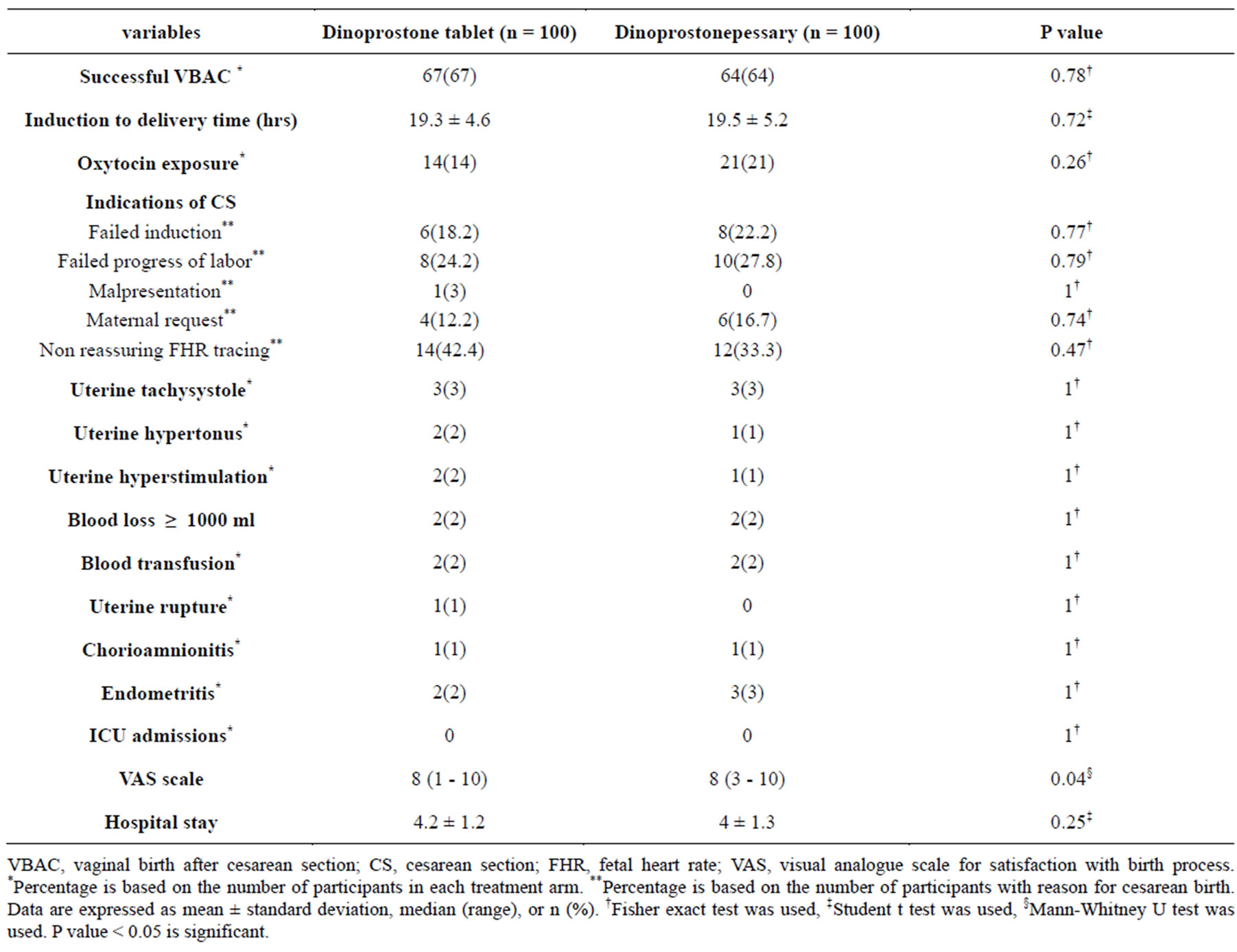
Table 2. Maternal outcome.
VBAC, vaginal birth after cesarean section; CS, cesarean section; FHR, fetal heart rate; VAS, visual analogue scale for satisfaction with birth process. *Percentage is based on the number of participants in each treatment arm. **Percentage is based on the number of participants with reason for cesarean birth. Data are expressed as mean ± standard deviation, median (range), or n (%). †Fisher exact test was used, ‡Student t test was used, §Mann-Whitney U test was used. P value < 0.05 is significant.
ticipants treated with the dinoprostone 1.5 mg and sustained release dinoprostone respectively (Table 2). The frequencies of uterine contractile abnormalities throughout labor were similar between the dinoprostone 1.5 mg and sustained release dinoprostone (Table 2). Medication-related uterine hyperstimulation syndrome occurred in three conditions (1.5%) of the 200 induced women, two cases in group A and one case in group B (Table 2). Oxytocin was administered to 14(14%) of participants in the dinoprostone 1.5 mg group and 21(21%) in the sustained release dinoprostone group (p = 0.26) (Table 2).
The VAS satisfaction scores revealed statistical preferences toward dinoprostone sustained release pessary. The median VAS satisfaction scores for the dinoprostone 1.5 mg group and sustained release dinoprostone group were [8 (1 - 10) and 8 (3 - 10), respectively; P = 0.04]. No significant difference in maternal outcome with respect to postpartum blood loss, postpartum hemorrhage (>1000 mL), blood transfusion, chorioamnionitis, postpartum endometritis or hospital stay was found between the two groups (Table 2). The overall uterine rupture rate in the study was 0.5 % (only one case in the dinoprostone 1.5 mg group compared with no cases in the dinoprostone sustained release group), but with no statistical difference between the two study groups (Table 2).
Table 3 presented data for neonatal outcomes during labor and delivery setting. Fetal body weight was similar in both groups. Neonatal Apgar scores both at 1 and 5 minutes, 5-minute Apgar score <7, umbilical cord pH (arterial and venous), arterial base deficit, respiratory morbidity, neonatal sepsis, and NICU admission did not differ significantly between the two groups. There was one case with a provisional diagnosis of neonatal asphyxia occurred in the dinoprostone 1.5 mg group. The baby was intubated for two days. Later, the baby was extubated and stayed in the NICU for another seven days, and then discharged home well.
4. COMMENTS
In the present study, we demonstrated that the 10 mg sustained release dinoprostone vaginal pessary had almost identical results for the efficacy and safety profile as the dinoprostone 1.5 mg vaginal tablet. Our results also demonstrated a low rate of uterine rupture (0.5%) in the 200 women attempting vaginal birth after cesarean section (VBAC) with induced labor (one patient in the dinoprostone 1.5 mg group versus no patient in the 10mg dinoprostone sustained release group). Furthermore, the median maternal satisfaction with the birth process (VAS score) was statistically significant in favor of the 10 mg sustained release dinoprostone vaginal pessary for labor induction. These data support and encourage the trial of labor after cesarean section (CS). Due to the rise in cesarean section in the current years, there were trials to reduce the number of repeat CS and induction of labor was considered in selected women with previous CS. This is principally beneficial in places where people are opting for a large family as there is increased incidence of complications [22]. Several studies suggested that for appro-
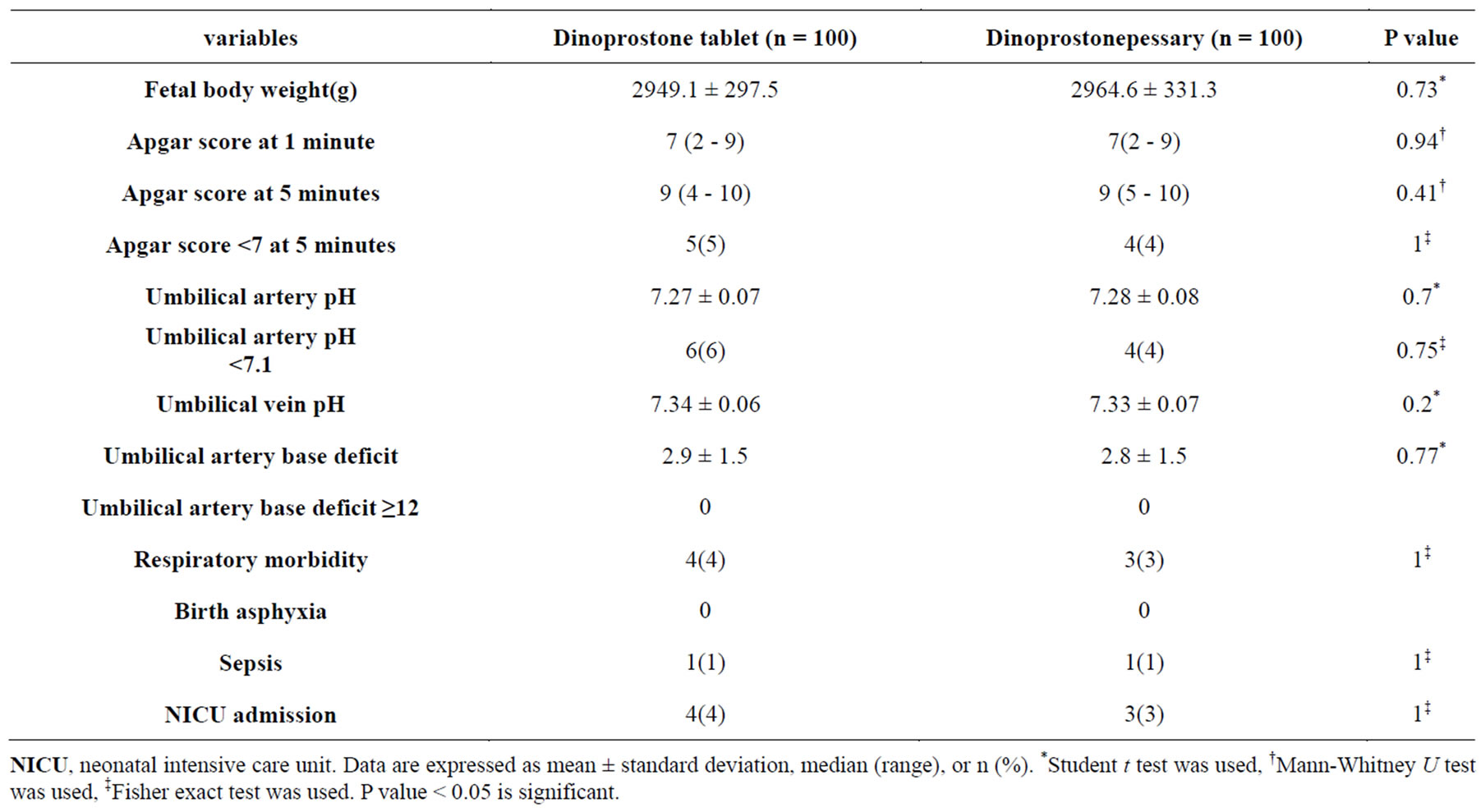
Table 3. Neonatal outcome.
NICU, neonatal intensive care unit. Data are expressed as mean ± standard deviation, median (range), or n (%). *Student t test was used, †Mann-Whitney U test was used, ‡Fisher exact test was used. P value < 0.05 is significant.
priately selected women with previous CS, a trial of labor is safe, even safer than elective repeat CS. The need for labor induction in women with previous CS poses a dilemma for physicians [23]. The American College of Obstetricians and Gynecologists (ACOG) updated their guidelines concerning vaginal delivery after previous CS. The ACOG Committee on Obstetrics: Maternal and Fetal Medicine stated; “the concept of routine repeat cesarean birth should be replaced by a specific indication for a subsequent abdominal delivery and in the absence of a contraindication, a woman with prior cesarean delivery with a low transverse incision should be counseled and encouraged to attempt labor in her present pregnancy” [24]. Moreover, the use of prostaglandins has been advocated by the Royal College of Obstetricians and Gynecologists (RCOG) even in cases with prior cesarean birth [25].
Many systematic reviews evaluated labor induction in women with previous CS using different agents with successful VBAC in 50% - 70% of women [25-27]. Dinoprostone vaginal tablets are the simplest formulation to administer, but it may need repeated application. Meanwhile, the sustained release dinoprostonepessary releases a continuous and predictable dose of dinoprostone at a rate of approximately 0.3 mg/h for 24 h with single vaginal application. The progressive cervical ripening induced by the controlled release of dinoprostone may be more acceptable to patients than the rapid onset of contractions observed with dinoprostone vaginal tablets [19]. The present study demonstrated that both forms of vaginal dinoprostone (1.5 mg tablet and 10 mg sustained release pessary) were efficient in inducing labor among women with previous CS. Our data displayed that the vaginal delivery rate was 67% in the 1.5 mg dinoprostone group A and 64% in the 10 mg dinoprostone sustained release group with no statistical difference. A similar success rate of labor induction was reported by Stock et al., [28] who performed a retrospective study on women with one previous CS, in Scotland and United Kingdom over 27 years. The overall vaginal delivery rate was achieved in nearly 60% of women attempting labor induction between 39 and 42 weeks (4399/7401). Similarly, Ouzounian et al., [29] performed a retrospective cross-sectional cohort study on 6833 patients with prior CS. Of these, 5027 women had spontaneous onset of labor and 1806 women had labor induced with either dinoprostone vaginal tablets or oxytocin. They showed that women with labor induction had an overall successful VBAC in 66.4% of cases. Furthermore, two recent prospective studies had evaluated dinoprostone for labor induction in patients with previous CS and demonstrated a comparable successful vaginal rate. On the other hand, Gómez and colleagues [30] conducted a retrospective study to compare the efficacy and safety profile between the dinoprostone vaginal pessary and oxytocin for labor induction in 526 pregnant women with prior CS. They revealed no significant difference between the two methods in the rates of vaginal delivery (64.4% for the dinoprostone group and 65.9% for the oxytocin group, P = 0.71). Meanwhile, Aslam et al., [31] conducted a retrospective review over a period of 3 years, evaluating the maternal and fetal outcome of labor induction with 10 mg dinoprostone vaginal pessary in women with previous CS, and revealed successful VBAC in 52% (30/58) of women after labor induction. The difference in the successful VBAC rate after labor induction could be attributed to the use of different induction protocols, using dinoprostonepessary in place for either 12 or 24 hours, different definition of labor induction failure, and altered patients' selection criteria.
Our pilot study revealed that the safety profile of the two forms of dinoprostone for labor induction in patients with prior CS was similar for both the maternal and neonatal outcomes. The overall risk of uterine rupture was 0. 5% out of the 200 participants in the study for labor induction with no statistical difference between individual groups (1% in the dinoprostone 1.5 mg group versus no patient in the dinoprostone sustained release group). Uterine rupture was measured in many previous studies [7,13,14,32] evaluating labor induction in patients with prior cesarean delivery and finding uterine rupture rate ranging between 0.35% [13] and 4.35% [32]. The wide range of uterine rupture rate among those studies may be explained by the lack of clear definition of uterine rupture because it is only those that cause symptoms are relevant to the assessment of the health risks of VBAC. The present study displayed a low rate of uterine rupture as it provided a clear definition for uterine rupture. Furthermore, the relatively low rate of dinoprostone related complications found in the present study may be correlated to our implementation of a strict protocol of labor induction, avoidance of additional applications of dinoprostone vaginal tablets or removal of the dinoprostone vaginal pessary if spontaneous uterine contractions are recorded, cautious use of oxytocin and on top of it, generous performance of CS.
The other maternal outcomes in both groups, including major bleeding, blood transfusion, chorioamnionitis, postpartum endometritis, and uterine contractile abnormalities (uterine tachysystole, hypertonus and hyperstimulation) were infrequently reported in our study with no statistical difference noted between both groups. These data were consistent with the systematic review including 203 studies conducted by Guise et al., [33] over the period 1980 to 2009 to evaluate maternal and neonatal outcomes in relation to VBAC. They stated that the adverse outcomes were rare for both elective repeat cesarean delivery and trial of labor. Meanwhile, the uterine contractile abnormalities were evaluated in a recent study conducted by Ziyauddin and colleagues [34] on seventy women with previous CS and required induction of labor. They reported incidence of uterine tachysystole and hypertonus in the dinoprostone vaginal gel group of 8.6% and 2.9%, respectively. The higher rate of tachysystolein this study may be related to the high rate of oxytocin usage (74.3%) compared with our study (14% and 21% in group A and B respectively).On the contrary, our study revealed that the maternal satisfaction score for the birth process was significantly in favor of dinoprostone sustained release pessary for labor induction when compared withdinoprostone vaginal tablets (p = 0.04). Likewise, Rath [35] stated that the progressive cervical ripening induced by the controlled release of dinoprostone may be more acceptable to patients than the rapid onset of contractions observed with other dinoprostone agents. Moreover, Kalkatand colleagues [36] conducted a randomised controlled trial to compare the safety profile, efficiency, and cost-effectiveness of dinoprostonepessary (Propess) with dinoprostone vaginal gel (Prostin) for labor induction on a total of 120 women, and stated that the number of vaginal examinations was significantly lower in the Propess group, and Propess was found to be more cost effective compared with Prostin in view of single dose and less midwifery hours.
The present study displayed a low rate of adverse neonatal outcomes with no statistical difference in the neonatal morbidity between the two study groups. These findings are in agreement with some studies [28,29,33,37], but disagree with others [6,32] that demonstrated a higher rate of adverse neonatal outcome in association with a failed trial of scar, non-availability of modern neonatology equipment, or increased uterine rupture rate.
5. CONCLUSION
In conclusion, the current study showed that the sustained release dinoprostone pessary had a high success rate of vaginal delivery after labor induction in terms of pregnant women with prior cesarean delivery. In addition, both forms of dinoprostone did not adversely affect maternal or neonatal outcome. However, dinoprostone sustained release vaginal pessary had a superior patient satisfaction in labor induction over dinoprostone vaginal tablets. We cautiously suggest that when there is no absolute indication for repeated cesarean section, induction of labor with either form of dinoprostone may be considered. Though, the study had some limitations. First, it was the pilot study design. Second, the study had a small sample size for justification of results and the maternal and neonatal complications. Third, the women and caregivers were not blinded to drug allocation. So, it is important to have a larger multicenter randomized controlled study within ethnically different populations, to reach a more powerful conclusion and to evaluate the safety profile of both forms of dinoprostone for labor induction in patients with prior cesarean section.
CONFLICTS OF INTEREST
The authors have stated that there are no conflicts of interest in connection with this article.
ACKNOWLEDGEMENTS
No financial or commercial interests from any company were involved.
REFERENCES
- Lumbiganon, P., Laopaiboon, M., Gülmezoglu, A.M., Souza, J.P., Taneepanichskul, S., Ruyan, P., Attygalle, D.E., Shrestha, N., Mori, R., Nguyen, D.H., Hoang, T.B., Rathavy, T., Chuyun, K., Cheang, K., Festin, M., Udomprasertgul, V., Germar, M.J., Yanqiu, G., Roy, M., Carroli, G., Ba-Thike, K., Filatova, E. and Villar, J. (2010) Method of delivery and pregnancy outcomes in Asia: The WHO global survey on maternal and perinatal health 2007-08. Lancet, 375, 490-499. http://dx.doi.org/10.1111/j.1537-2995.2008.01697.x
- Buekens, P., Curtis, S. and Alayón, S. (2003) Demographic and health surveys: Cesarean section rates in subSaharan Africa. British Medical Journal, 326, 136. http://dx.doi.org/10.1136/bmj.326.7381.136
- Silver, R.M., Landon, M.B., Rouse, D.J., Leveno, K.J., Spong, C.Y., Thom, E.A., Moawad, A.H., Caritis, S.N., Harper, M., Wapner, R.J., Sorokin, Y., Miodovnik, M., Carpenter, M., Peaceman, A.M., O’Sullivan, M.J., Sibai, B., Langer, O., Thorp, J.M., Ramin, S.M. and Mercer, B.M. (2006) Maternal morbidity associated with multiple repeat cesarean deliveries. Obstetrics and Gynecology, 107, 1226-1232. http://dx.doi.org/10.1097/01.AOG.0000219750.79480.84
- Knight, M., Kurinczuk, J.J., Spark, P. and Brocklehurst, P. (2008) Cesarean delivery and peripartum hysterectomy. Obstetrics and Gynecology, 111, 97-105. http://dx.doi.org/10.1097/01.AOG.0000296658.83240.6d
- Martin, J.A., Hamilton, B.E., Sutton, P.D., Ventura, S.J., Menacker, F., Kirmeyer, S. and Munson, M.L. (2007) Births: Final data for 2005. National Vital Statistics Reports, 56, 1-103.
- Islam, A., Ehsan, A., Arif, S., Murtaza, J., and Hanif, A. (2011): Evaluating trial of scar in patients with a history of cesarean section. North American Journal of Medical Sciences, 3, 201-205. http://dx.doi.org/10.4297/najms.2011.3201
- Harper, L.M., Cahill, AG., Boslaugh, S., Odibo, A.O., Stamilio, D.M., Roehl, K.A. and Macones, G.A. (2012) Association of induction of labor and uterine rupture in women attempting vaginal birth after cesarean: A survival analysis. American Journal of Obstetrics and Gynecology, 206, 51.e1-5. http://dx.doi.org/10.1016/j.ajog.2011.09.022
- Lydon-Rochelle, M., Holt, V.L., Easterling, T.R. and Martin, D.P. (2001) Risk of uterine rupture during labor among women with a prior cesarean delivery. The New England Journal of Medicine, 345, 3-8. http://dx.doi.org/10.1056/NEJM200107053450101
- Macones, G.A., Peipert, J., Nelson, D.B., Odibo, A., Stevens, E.J., Stamilio, D.M., Pare, E., Elovitz, M., Sciscione, A., Sammel, M.D. and Ratcliffe, S.J. (2005) Maternal complications with vaginal birth after cesarean delivery: A multicenter study. American Journal of Obstetrics and Gynecology, 193, 1656-1662. http://dx.doi.org/10.1016/j.ajog.2005.04.002
- American College of Obstetricians and Gynecologists (2010) ACOG practice bulletin no. 115: Vaginal birth after previous cesarean delivery. Obstetrics and Gynecology, 116, 450-463. http://dx.doi.org/10.1097/AOG.0b013e3181eeb251
- Dekker, G.A., Chan, A., Luke, C.G., Priest, K., Riley, M., Halliday, J., King, J.F., Gee, V., O’Neill, M., Snell, M., Cull, V. and Cornes, S. (2010) Risk of uterine rupture in Australian women attempting vaginal birth after one prior cesarean section: A retrospective population-based cohort study. BJOG: An International Journal of Obstetrics and Gynecology, 117, 1358-1365. http://dx.doi.org/10.1111/j.1471-0528.2010.02688.x
- Sanchez-Ramos, L. and Kaunitz, A.M. (2000) Uterine rupture associated with the use of prostaglandin E1 in patients with previous cesarean delivery. American Journal of Obstetrics and Gynecology, 182, 990-991. http://dx.doi.org/10.1016/S0002-9378(00)70363-2
- Stovall, T.G., Shaver, D.C., Solomon, S.K. and Anderson, G.D. (1987) Trial of labor in previous cesarean section patients, excluding classical cesarean section. Obstetrics and Gynecology, 70, 713-717.
- Flamm, B.L., Goings, J.R., Fuelberth, N., Fischerman, E., Jones, C. and Hersh, E. (1987) Oxytocin during labor after previous cesarean section: Results of a multicenter study. Obstetrics and Gynecology, 70, 709-712.
- Lao, T.T. and Leung, B.F. (1987) Labor induction for planned vaginal delivery in patients with previous cesarean section. Acta Obstetrics Gynecology Scandinavia, 66, 413-416. http://dx.doi.org/10.3109/00016348709022044
- Steer, P.J. and Modi, N. (2009) Elective cesarean sections-risks to the infant. Lancet, 374, 675-676. http://dx.doi.org/10.1016/S0140-6736(09)61544-0
- Kelly, A.J., Malik, S., Smith, L., Kavanagh, J. and Thomas, J. (2009) Vaginal prostaglandin (PGE2 and PGF2α) for induction of labor at term. Cochrane Database Systematic Review, 4, CD 003101. http://dx.doi.org/10.1002/14651858.CD003101.pub2
- Lyrenas, S., Clason, I. and Ulmsten, U. (2001) In vivocontrolled release of PGE2 from a vaginal insert (0.8 mm, 10 mg) during induction of labor. BJOG: An International Journal of Obstetrics and Gynecology, 108, 169-178.
- Westgate, J. and Williams, J.A. (1994) Evaluation of a controlled release vaginal prostaglandin E2 pessary with retrieval system for the induction of labor. Journal of Obstetrics and Gynecology, 14, 146-150. http://dx.doi.org/10.3109/01443619409004060
- American College of Obstetricians and Gynecologists (1995) ACOG Practice Bulletin no 207. Washington DC, American College of Obstetricians and Gynecologists. Fetal heart rate patterns: monitoring, interpretation, and management. International Journal of Gynecology and Obstetrics, 51, 65-74. http://dx.doi.org/10.1016/0020-7292(95)80014-4
- American College of Obstetricians and Gynecologists Committee on Obstetric Practice (2006) ACOG Committee opinion No. 348: Umbilical cord blood gas and acid base analysis. Obstetrics and Gynecology, 108, 1319- 1322. http://dx.doi.org/10.1097/00006250-200611000-00058
- Geetha, P. (2012) Induction of labor with prostaglandin E2 vaginal gel in women with one previous cesarean section. Middle East Fertility Society Journal, 17, 170-175.
- Yogev, Y., Ben-Haroush, A., Lahav, E., Horowitz, E., Hod, M. and Kaplan, B. (2004) Induction of labor with prostaglandin E2 in women with previous cesarean section and unfavorable cervix. European Journal of Obstetrics & Gynecology and Reproductive Biology, 116, 173- 176. http://dx.doi.org/10.1016/j.ejogrb.2004.02.019
- American College of Obstetricians and Gynecologists Committee on Obstetric Practice (2006) ACOG Committee opinion No. 342: Induction of labor for vaginal birth after cesarean delivery. Obstetrics & Gynecology, 108, 465- 468. http://dx.doi.org/10.1097/00006250-200608000-00045
- McDonagh, M.S., Osterweil, P. and Guise, J.M. (2005) The benefits and risks of inducing labor in patients with prior cesarean delivery: A systemic review. BJOG: An International Journal of Obstetrics and Gynecology, 112, 1007-1015. http://dx.doi.org/10.1111/j.1471-0528.2005.00623.x
- Dodd, J. and Crowther, C. (2004) Induction of labor for women with a previous Cesarean birth: A systematic review of the literature. Australian and New Zealand Journal of Obstetrics and Gynecology, 44, 392-395. http://dx.doi.org/10.1111/j.1479-828X.2004.00258.x
- Dodd, J.M. and Crowther, C.A. (2012) Elective repeat cesarean section versus induction of labor for women with a previous caesarean birth. Cochrane Database of Systematic Reviews, 5, CD004906. http://dx.doi.org/10.1002/14651858.CD004906.pub3
- Stock, S.J., Ferguson, E., Duffy, A., Ford, I., Chalmers, J. and Norman, JE. (2013) Outcomes of induction of labor in women with previous cesarean delivery: A retrospective cohort study using a population database. PLoS ONE, 8, e60404. http://dx.doi.org/10.1371/journal.pone.0060404
- Ouzounian, J., Miller, D., Hiebert, C., Battista, L. and Lee, R. (2011) Vaginal birth after cesarean section: Risk of uterine rupture with labor induction. American Journal of Perinatology, 28, 593-596. http://dx.doi.org/10.1055/s-0031-1275386
- Gómez, L.R., Burgos, J., Cobos, P., Melchor, J.C., Osuna, C., Centeno Mdel, M., Larrieta, R., Fernández-Llebrez, L. and Martínez-Astorquiza, T. (2011) Oxytocin versus dinoprostone vaginal insert for induction of labor after previous cesarean section: A retrospective comparative study. Journal of Perinatal Medicine, 39, 397-402. http://dx.doi.org/10.1515/jpm.2011.030
- Aslam, N., Ghatak, S., Mulay, A. and Sharma, S. (2010) Outcome of IOL with propess in previous cesarean section. Archives of Disease in Childhood. Fetal and Neonatal Edition, 95, Fa77-Fa78.
- Meehan, F.P. and Burke, G, (1989) Trial of labor following prior section; a 5 year prospective study (1982-1987). European Journal of Obstetrics & Gynecology and Reproductive Biology, 31, 109-117. http://dx.doi.org/10.1016/0028-2243(89)90171-8
- Guise, J., Denman, M., Emeis, C., Marshall, N., Walker, M., Rongwei, F., Janik, R., Nygren, P., Eden, K. and McDonagh, M. (2010) Vaginal birth after cesarean: New insights on maternal and neonatal outcomes. Obstetrics and Gynecology, 115, 1267-1278. http://dx.doi.org/10.1097/AOG.0b013e3181df925f
- Ziyauddin, F, Hakim, S. and Beriwal, S. (2013) The transcervical foley catheter versus the vaginal prostaglandin E2 gel in the induction of labor in a previous one cesarean section: A clinical study. Journal of Clinical and Diagnostic Research, 7, 140-143. http://dx.doi.org/10.7860/JCDR/2012/5003.2689
- Rath, W. (2005) A clinical evaluation of controlled-release dinoprostone for cervical ripening—A review of current evidence in hospital and outpatient settings. Journal of Perinatal Medicine, 33, 491-499. http://dx.doi.org/10.1515/JPM.2005.087
- Kalkat, R.K., McMillan, E., Cooper, H. and Palmer, K. (2008) Comparison of Dinoprostone slow release pessary (Propess) with gel (Prostin) for induction of labor at term—A randomised trial. Journal of Obstetrics & Gynecology, 28, 695-699. http://dx.doi.org/10.1080/01443610802462522
- Wanyonyi, S. and Karuga, R. (2010) The utility of clinical care pathways in determining perinatal outcomes for women with one previous cesarean section; a retrospective service evaluation. BMC Pregnancy and Childbirth, 10, 62-68. http://dx.doi.org/10.1186/1471-2393-10-62
NOTES
*Corresponding author.

