D. DONATACCIO ET AL.
Copyright © 2011 SciRes. SS
260
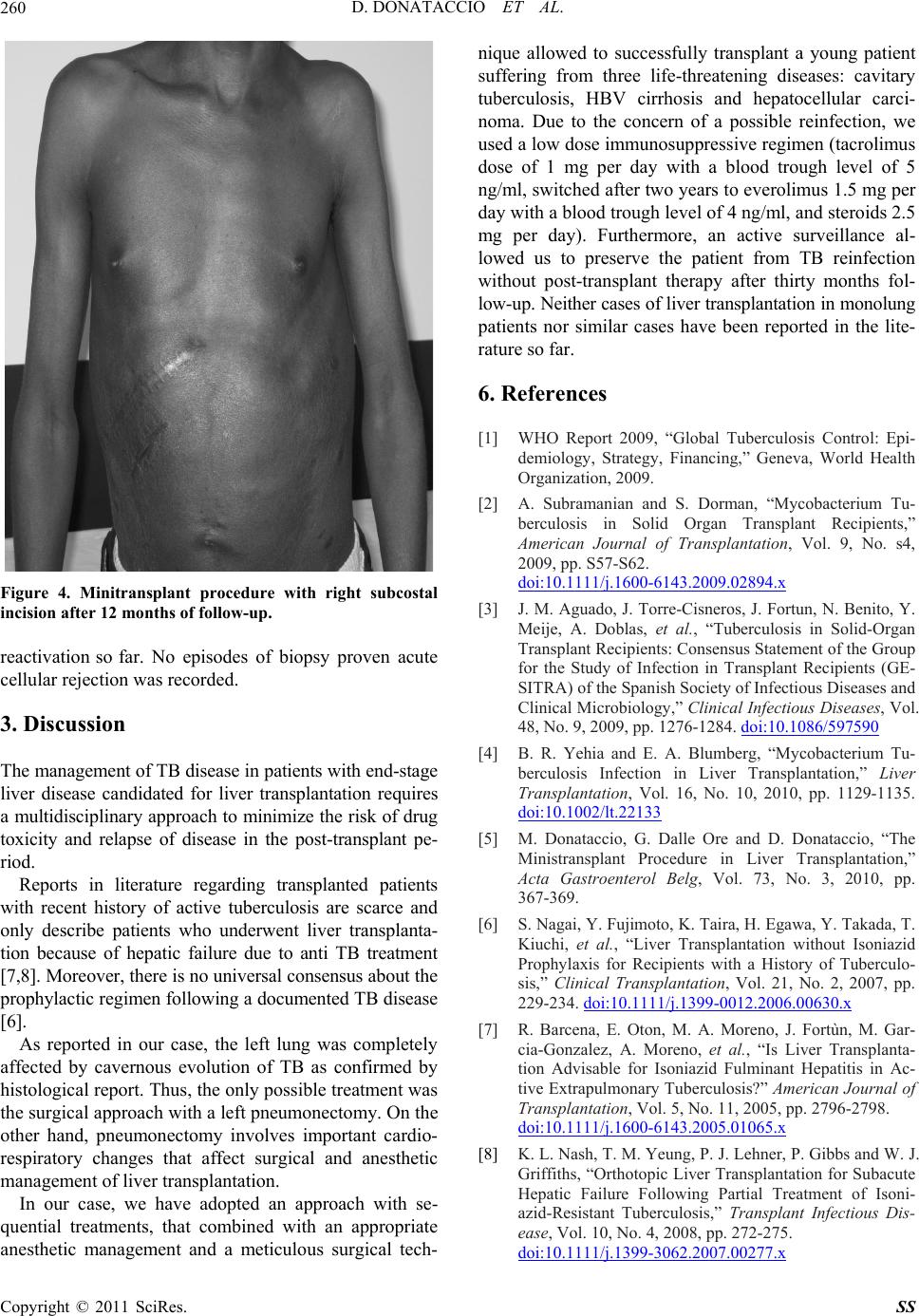
Figure 4. Minitransplant procedure with right subcostal
incision after 12 months of follow-up.
reactivation so far. No episodes of biopsy proven acute
cellular rejection was recorded .
3. Discussion
The management of TB disease in patients with end-stage
liver disease candidated for liver transplantation requires
a multidisciplinary approach to minimize the risk of drug
toxicity and relapse of disease in the post-transplant pe-
riod.
Reports in literature regarding transplanted patients
with recent history of active tuberculosis are scarce and
only describe patients who underwent liver transplanta-
tion because of hepatic failure due to anti TB treatment
[7,8]. Moreover, there is no universal consensus about the
prophylactic regimen following a documented TB disease
[6].
As reported in our case, the left lung was completely
affected by cavernous evolution of TB as confirmed by
histological report. Thus, the only possible treatment was
the surgical approach with a left pneumonectomy. On the
other hand, pneumonectomy involves important cardio-
respiratory changes that affect surgical and anesthetic
management of liver transplantation.
In our case, we have adopted an approach with se-
quential treatments, that combined with an appropriate
anesthetic management and a meticulous surgical tech-
nique allowed to successfully transplant a young patient
suffering from three life-threatening diseases: cavitary
tuberculosis, HBV cirrhosis and hepatocellular carci-
noma. Due to the concern of a possible reinfection, we
used a low dose immunosuppressive regimen (tacrolimus
dose of 1 mg per day with a blood trough level of 5
ng/ml, switched after two years to everolimus 1.5 mg per
day with a blood trough level of 4 ng/ml, and steroids 2.5
mg per day). Furthermore, an active surveillance al-
lowed us to preserve the patient from TB reinfection
without post-transplant therapy after thirty months fol-
low-up. Neither cases of liver transplantation in monolung
patients nor similar cases have been reported in the lite-
rature so far.
6. References
[1] WHO Report 2009, “Global Tuberculosis Control: Epi-
demiology, Strategy, Financing,” Geneva, World Health
Organization, 2009.
[2] A. Subramanian and S. Dorman, “Mycobacterium Tu-
berculosis in Solid Organ Transplant Recipients,”
American Journal of Transplantation, Vol. 9, No. s4,
2009, pp. S57-S62.
doi:10.1111/j.1600-6143.2009.02894.x
[3] J. M. Aguado, J. Torre-Cisneros, J. Fortun, N. Benito, Y.
Meije, A. Doblas, et al., “Tuberculosis in Solid-Organ
Transplant Recipients: Consensus Statement of the Group
for the Study of Infection in Transplant Recipients (GE-
SITRA) of the Spanish Society of Infectious Diseases and
Clinical Microbiology,” Clinical Infectious Diseases, Vol.
48, No. 9, 2009, pp. 1276-1284. doi:10.1086/597590
[4] B. R. Yehia and E. A. Blumberg, “Mycobacterium Tu-
berculosis Infection in Liver Transplantation,” Liver
Transplantation, Vol. 16, No. 10, 2010, pp. 1129-1135.
doi:10.1002/lt.22133
[5] M. Donataccio, G. Dalle Ore and D. Donataccio, “The
Ministransplant Procedure in Liver Transplantation,”
Acta Gastroenterol Belg, Vol. 73, No. 3, 2010, pp.
367-369.
[6] S. Nagai, Y. Fujimoto , K. Tair a, H. Egawa, Y. T akada, T.
Kiuchi, et al., “Liver Transplantation without Isoniazid
Prophylaxis for Recipients with a History of Tuberculo-
sis,” Clinical Transplantation, Vol. 21, No. 2, 2007, pp.
229-234. doi:10.1111/j.1399-0012.2006.00630.x
[7] R. Barcena, E. Oton, M. A. Moreno, J. Fortùn, M. Gar-
cia-Gonzalez, A. Moreno, et al., “Is Liver Transplanta-
tion Advisable for Isoniazid Fulminant Hepatitis in Ac-
tive Extrapulmonary Tuberculosis?” American Journal of
Transplantation, Vol. 5, No. 11, 2005, pp. 2796-2798.
doi:10.1111/j.1600-6143.2005.01065.x
[8] K. L. Nash, T. M. Yeung, P. J. Lehner, P. Gibbs and W. J.
Griffiths, “Orthotopic Liver Transplantation for Subacute
Hepatic Failure Following Partial Treatment of Isoni-
azid-Resistant Tuberculosis,” Transplant Infectious Dis-
ease, Vol. 10, No. 4, 2008, pp. 272-275.
doi:10.1111/j.1399-3062.2007.00277.x