K. Taori et al.
OALibJ | DOI:10.4236/oalib.1100670 4 July 2014 | Volume 1 |
We gave the possibility of infantile myofibroma of posterior fossa as most likely diagnosis over other more
common lesio ns in this locati on like primitive neuroectodrmal tumor and a typical ter atoid rhab doid tumor. I m-
aging fe at ur e s fa vo urin g the po ssi bi lity was iso i nt e nsi t y of the l esi o n to b r ai n pa r enc hyma o n d iffus i o n we i ght ed
sequence. Skeletal survey and ultrasonography of abdomen was done which did not reveal any significant ab-
nor malit y.
The mass in our case possibly arose from the lateral dural margin directly invaded the right sigmoid sinus and
eroded the petrous temporal bone. The MR images confirmed the obliteration of the sigmoid sinus and enlarge-
ment of the jugular foramen. Supra-tentorial brain parenchyma showed normal gray-white matter.
Patient was referred to neurosurgery where biopsy was performed and specimen was pathlogically conrfimed
to be consistent with imaging diagnosis of infantile myofibroma revealing whorls of spindle shaped cells of
myofibrob lastic origin. Subtotal r esection was performe d. Care was t aken no t to avo id damage to the lower cra-
nial nerves, and resection was not extended into the carotid sheath or internal jugular vein.
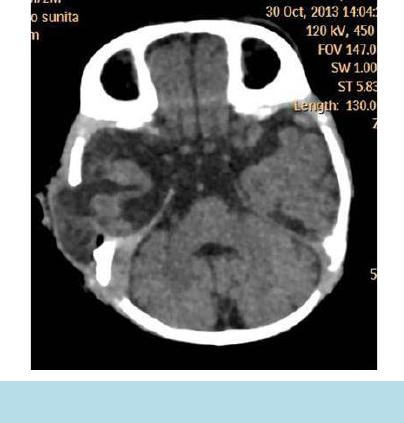
Follo w-up i maging (Figure 6) at 3 months after resection revealed significant reductio n in size of the lesio n,
consi stent wi t h the natural history of this rare entity.
3. Discussion
Infantile myofibromatosis which is the most common fibrous disorder of infancy and early childhood was first
described by Stout in 1954 [2]. It is more commonly seen in males. However, exact incidence is not known due
to variable and unpredictable natural course of the disease. It is a disease with variable prognosis depending on
type and extent of involvement. It can present in three forms-solitary lesion, multicentric lesions with visceral
involvement and multicenteric lesions without visceral involvement. Multicenteric lesions can occur in skin,
musc le, bone, subcutaneous tissue and viscera. More the visceral involvement worse is the outcome. The com-
mon sites with visceral i nvolv e ment were lu ng, hear t, gastr ointes tinal tar ct, p ancreas a nd liver . Ho wever, lesio ns
have rarely been noted in intracranial compartment which are usually due to extension of the extracranial proc-
ess [3]. They are typically seen arising from dura and less frequently may show intrapaenchymal or spine in-
volve me nt.
The etiology of infantile fibromatosis is unknown so far. However, effects of maternal estrogen and familial
association have been hypothesized [4].
Radiological studies are not characteristic due to variable appearances but it is very important in assessing the
extent of the disease [5]. It usually appears as enhancing extra axial lesion with calci fications. It does not s how
restriction on diffusion weighted imaging in contrast due to highly cellular tumors like atypical terato id rhabdo id
tumor and primitive neuroectodermal tumors. Since the condition is not commonly known it may mimic ma lig-
nant tumors. Definite diagnosis depends on histology.
The current is unique due to isolated posterior fossa involvement with minimal transjugular extension. Al-
Figure 6 . Follow-up plain CT head reveals significant
reduction in size of lesion with post operative changes.