Neuroscience & Medicine
Vol.4 No.2(2013), Article ID:33248,2 pages DOI:10.4236/nm.2013.42014
A Rare Case of Isolated Left Medial Midbrain Stroke
![]()
Department of Medicine, Faculty of Medicine, University of Malaya, Kuala Lumpur, Malaysia.
Email: *sharont1990@gmail.com
Copyright © 2013 Mei-Ling Sharon Tai, Vijayan P. Panirselvam. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received March 16th, 2013; revised April 20th, 2013; accepted May 7th, 2013
Keywords: Stroke; Midbrain; Cranial Nerve
ABSTRACT
Midbrain stroke is uncommon. We are presenting an interesting case of a patient with rare isolated left midbrain stroke. The patient had third cranial nerve palsy. Magnetic resonance imaging (MRI) brain showed acute stroke at the medial part of left midbrain. Magnetic resonance angiography (MRA) was normal.
1. Introduction
Midbrain stroke consists of 3% of all posterior circulation strokes [1]. Isolated, midbrain ischaemic strokes are uncommon because arterial blood supplying to mesencephalon is complex [1]. We are presenting an interesting case of a patient with rare isolated left midbrain stroke.
2. Case Report
The patient was a 52 years old lady with history of hypertension for a year. She presented on 20th December 2012 with three days’ history of headache at parietal and occipital areas of moderate severity. She had visual blurring at left eye, which was of sudden onset at 8 pm on the day of admission. She noticed that her left eye was deviated outwards and downwards. She had double vision and dizziness. She also had numbness at the right palm and sole. She was a chronic smoker.
On examination, BP was 212/112. Pulse rate was 85 and she was afebrile. She was alert and conscious. There was reduction in visual acuity at the left eye (finger counting). The left pupil was 3 mm (bigger) and was reactive to light. The right pupil was 2 mm and was reactive to light. She had partial ptosis on the left eye. The left eye was deviated downwards and outwards. There was weakness of adduction and elevation of the left eye. There was diplopia on looking to the left horizontally. She had loss of nasolabial fold on right face.
On examination of upper and lower limbs, tone and reflexes were normal. Power was 5/5. Plantar response was downgoing bilaterally. There were no cerebellar signs. Speech and swallowing was normal.
Computed Tomography (CT) scan of the brain done on the 20th December 2012 showed old lacunar stroke at the left basal ganglia area.ECG and chest X-ray was normal. CT angiography done on the 21st December 2012 was normal. She was started on aspirin and simvastatin.
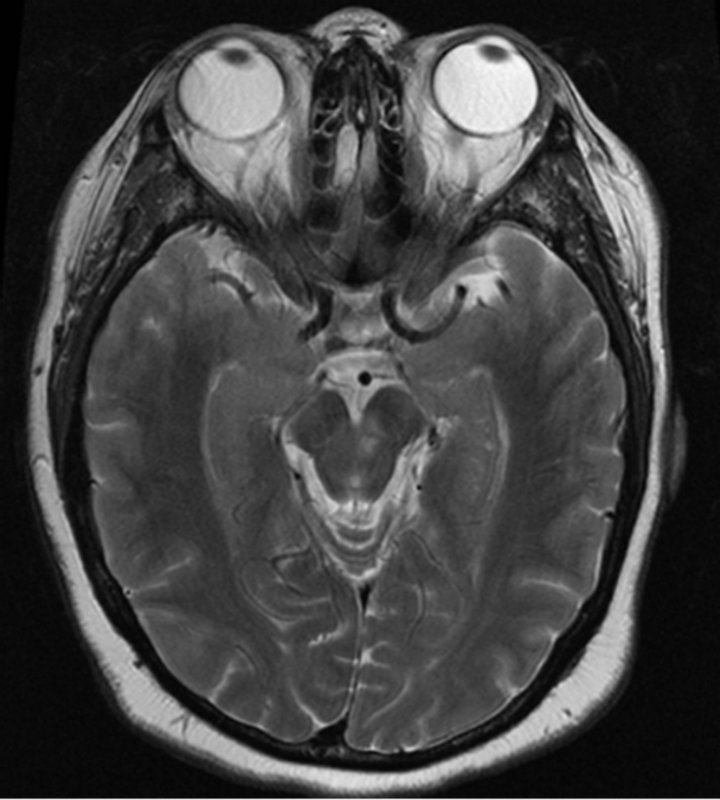
On 24th December 2012, the third cranial nerve palsy was still present. The right facial deviation was not present anymore. The Magnetic Resonance Imaging (MRI) of the brain on 26th December 2012 showed acute stroke at the medial aspect of the left midbrain (Refer to Figures 1(a) and (b)). The MR angiography was normal (Refer to Figure 2).The patent was discharged on 27th December 2012.
On the 11th January 2013, she was reviewed at clinic. Left eye adduction was normal. Pupils were 3 mm bilaterally. The rest of signs were still present. On the next follow-up on 25th January 2013, the left eye adduction and elevation was normal. The ptosis had resolved.
3. Discussion
We are presenting an interesting case of a patient with stroke at the medial aspect of the left midbrain, in the absence of stenosis or occlusion at the basilar artery or vertebral arteries on MRA.
The infarct at the medial aspect of left midbrain is caused by occlusion of interpeduncular branches of left posterior cerebral artery [2,3]. The interpeduncular branches arise from just above the basilar bifurcation at
 (a)
(a)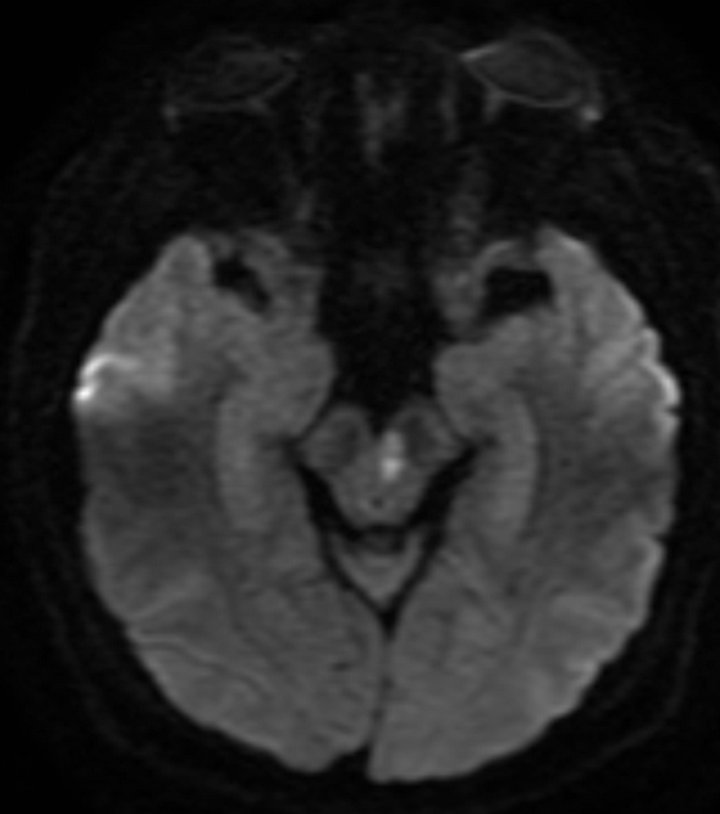 (b)
(b)
Figure 1. (a) MRI brain T2 weighted image; (b) MRI brain diffusion weighted image (DWI).
the region between the bifurcation of basilar artery and ostium of posterior communicating artery [3]. These branches are also called mesencephalic artery and are paramedian arteries [3]. The interpeduncular branches supply oculomotor nucleus and nerves [3].
This case is a rare case of midbrain stroke in isolation [2]. Stroke at the midbrain area is ten times more likely
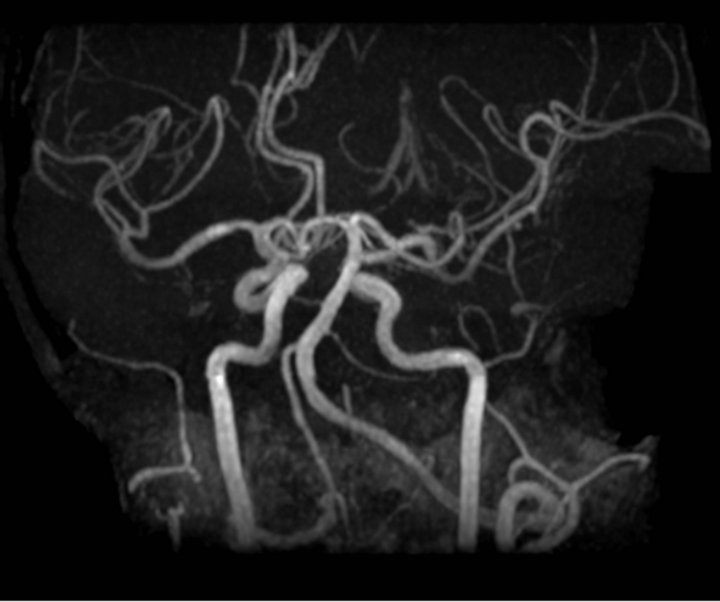
Figure 2. MR angiography.
to be associated with ischaemia of neighbouring structures than to occur in isolation [1,2]. The middle mesencephalon is involved more frequently than other regions [1].
Isolated midbrain stroke consists of 8% of all midbrain strokes [2]. The symptoms are dizziness and unsteadiness [1]. The signs are oculomotor abnormalities including vertical palsy (with or without horizontal gaze palsy), hemiataxia and motor signs (mild hemiparesis) [2,4,5]. The paramedian midbrain strokes are more prone to cause nuclear third cranial nerve paralysis [2].
4. Conclusion
We are presenting an interesting case of a patient with rare isolated left midbrain stroke with third cranial nerve palsy with normal MRA.
REFERENCES
- E. Kumral, G. Bayalkem, A. Akyol, N. Yunten, H. Sirin and A. Sagduyu, “Mesencephalic and Associated Posterior Circulation Infarcts,” Stroke, Vol. 33, No. 9, 2002, pp. 2224-2231. doi:10.1161/01.STR.0000027438.93029.87
- P. J. Martin, H. M. Chang, R. Wityk and L. R. Caplan, “Midbrain Infraction: Association and Aetiologies in the New England Medicine Centre Posterior Circulation Registry,” Journal of Neurology, Neurosurgery & Psychiatry, Vol. 64, 1998, pp. 392-395. doi:10.1136/jnnp.64.3.392
- A. H. Ropper and R. H. Brown, “Adams and Victor’s Principles of Neurology,” 8th Edition, McGraw Hill, Boston, 2005.
- J. Bogousslavsky, Ph. Maeder, F. Regli, R. Mauli, “Pure Midbrain Infraction: Clinical Syndrome, MRI and Etiology Pattern,” Neurology, Vol. 44, No. 11, 1994, pp. 2032- 2040. doi:10.1212/WNL.44.11.2032
- J. Bogousslavsky, “Oculomotor Syndromes Resulting from Mesencephalic Lesions in Man,” Revue Neurologique (Paris), Vol. 145, No. 8-9, 1989, pp. 546-59.
NOTES
*Corresponding author.

