Open Journal of Stomatology
Vol.07 No.09(2017), Article ID:79034,9 pages
10.4236/ojst.2017.79036
Peripheral Complex Odontoma in the Gingiva: A Case Report of an 11 Year Old Boy and Review of Literature
Gunnar Ingi Jóhannsson1,2*, Steen Bærentzen3, Johan Blomlöf1
1Department of Oral and Maxillofacial Surgery, Aarhus University Hospital, Aarhus, Denmark
2Department of Oral and Maxillofacial Surgery, Aalborg University Hospital, Aalborg, Denmark
3Department of Pathology, Aarhus University Hospital, Aarhus, Denmark

Copyright © 2017 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY 4.0).
http://creativecommons.org/licenses/by/4.0/



Received: August 8, 2017; Accepted: September 10, 2017; Published: September 13, 2017
ABSTRACT
According to the WHO histological classification of odontogenic tumours, odontomas originate from odontogenic epithelium and odontogenic ectomesenchyme, with or without hard tissue formation. They are generally classified into two types: complex and compound. Odontomas are usually intraosseous and often associated with delayed eruption of teeth. However, they can be extraosseous and are then referred to as either peripheral complex or compound odontoma. Peripheral odontomas are rare entities. We report a case of an 11 year old boy referred to the Department of Oral and Maxillofacial Surgery, Aarhus University Hospital by the boy’s dentist due to fibrous mass in the marginal gingiva in the anterior lower mandible. Removal of the mass revealed a peripheral complex odontoma and at the final 5-month postoperative inspection there was satisfying healing observed, a small, elevated, hyperplastic fibrous marginal gingiva.
Keywords:
Odontogenic Tumour, Odontoma, Hamartoma, Complex, Extraosseous, Peripheral

1. Introduction
Odontomas fall within the category of mixed epithelial and mesenchymal odontogenic tumours. The epithelial part gives rise to enamel and the mesenchymal part produces dentin via odontoblast differentiation. They are hamartomas of aborted tooth formation, the definition of a hamartoma is: a tumorlike dysmorphic proliferations of cells native to the organ in which they arise. They gain a certain size before ceasing their proliferation. They may be expansile but do not invade tissue [1] [2] .
Odontomas are classified into: complex and compound. Complex odontomas form an amorphous mass which is unrecognizable as dental tissues compared to the compound type which forms multiple small tooth-like structures which show three separate dental tissues (enamel, dentin and cementum) [1] [2] . Odontomas are one of the most common odontogenic tumours, and usually occur in children and young adults [1] [2] [3] . Odontomas are usually incidental radiographic findings and also found in relation to delayed tooth eruption. They can also cause bone expansion, however they show limited slow growth and are usually asymptomatic [2] . Compound odontomas occur most often in the anterior maxilla while the complex type is more common in the posterior maxilla or mandible [1] [2] [4] . Radiographically, complex odontomas appear with a amorphous mass of calcified material with the radiodensity of a tooth structure, which bears no anatomical resemblance to a tooth surrounded by a narrow radiolucent rim. However, the radiographic appearance depends on the development stage. Three stages exist based on the degree of mineralization [2] .
2. Case Report
The patient, an 11-year old boy was referred to the Department of Oral and Maxillofacial Surgery at the University Hospital in Aarhus, Denmark due to a fibrous mass in the labial marginal gingiva of the lower right lateral incisor. The patient was of African ethnicity. He reported that he had been aware of the fibrous mass for at least 2 years and that it had slowly grown in size in that period. He had not noticed any particular bleeding or pain, however it was starting to cause him discomfort during food intake. In regard to his general health and medical history there was nothing specific to report.
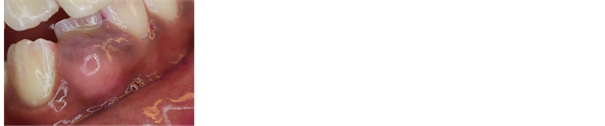
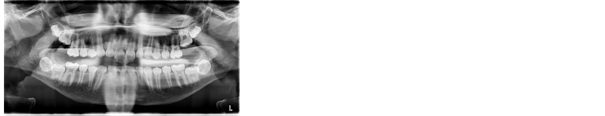
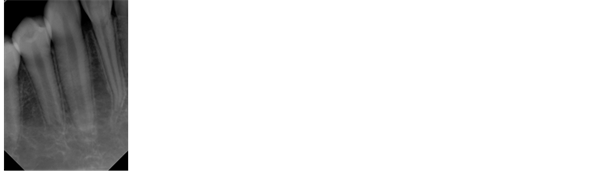
Extraoral clinical examination did not reveal any asymmetry. The intraoral examination revealed that the patient was at dental age stage DS4 M1 according to Björk et al. 1964 classification [5] . During examination of the patient’s soft tissue the fibrous mass in the facial marginal gingiva (Figure 1) in relation to the lower right lateral incisor could easily been seen. The mass was broad-based with a firm consistency and the gingival soft tissue showed normal color as well as marginal gingival pocket probing depth of 3 mm. Panoramic and periapical radiographs showed a slight radiopaque, demarcated mass located in relation to the tooth (Figure 2 and Figure 3).
The differential diagnosis according to the clinical and radiographic examination was either a peripheral giant cell granuloma or a peripheral ossifying fibroma.
It was decided to perform an excisional biopsy to determine the definitive diagnosis. There was no suspicion of malignancy. Under local anesthesia, the fibrous mass was removed in whole. It had underlying relation to the facial alveolar bone. The area was left to heal by secondary intention. At follow-up 2
Figure 1. Fibrous mass in the labial marginal gingiva of the lower right lateral incisor at initial examination.
Figure 2. Panoramic radiograph at initial examination.
Figure 3. Periapical radiograph at initial examination.
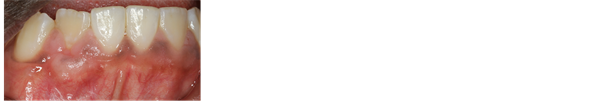
Figure 4. A small, elevated, hyperplastic fibrous marginal gingiva at 5-months postoperatively.
weeks later, the patient described a uneventful postoperative period. A small tooth fragment was found peripherally and was removed, otherwise uneventful healing was seen. At 3-months postoperatively a small area of exposed bone (3 × 2 mm) was described and finally at 5-months postoperatively a small, elevated, hyperplastic fibrous marginal gingiva was observed (Figure 4). The boy was referred back to his own dentist for regular observation.
3. Histology
Macroscopic examination of the specimen showed soft tissue covered by mucosa measuring at 9.0 × 8.0 × 4.0 mm in size. It had a half-spherical form, which was divided longitudinally and revealed bone like material on the cut surface. The specimen was hard as bone prior to decalcification and moderately indurated after.
Microscopic examination showed at low power view a complex odontoma encapsulated by slightly chronically inflamed dense connective tissue superficially covered by well differentiated slightly parakeratotic squamous epithelium of the oral mucosa (Figure 5). The odontoma was made up of dentin with irregularly oriented pools of enamel matrix and connective tissue (Figure 6). At higher magnification, pulp-like connective tissue with islands of odontogenic epithelium and basophilic cementum-like matrix could easily be detected (Figure 7), as well as dentin with irregular tubule formation and enamel matrix with a few ameloblast-like cells (Figure 8). There were no signs of malignancy and the histological diagnosis was a peripheral complex odontoma.
The histological slides were made after decalcification, where the red dentin and bone/cement matrix (collagen component) were preserved while most of the enamel was dissolved (shown as empty spaces) with a few small rests of enamel which are shown with arrows on the histological slides.
Figure 5. HE stain, 20 × magnification.
Figure 6. HE stain, 100 × magnification.
Figure 7. HE stain, 200 × magnification.
Figure 8. HE stain, 200 × magnification.
4. Discussion
Intraosseous odontomas are among the most common odontogenic tumours together with ameloblastomas [3] [4] . The peripheral type however, is very rare. That applies both to the compound and complex types, although it seems that the compound type is a bit more common [6] . This makes it quite challenging to make the correct clinical diagnosis. There are many differential diagnoses in relation to an exophytic fibrous mass on the gingiva as in this case report, e.g. peripheral giant cell tumour, peripheral ossifying fibroma, periodontal abscess, gingival hyperplasia etc. [4] . Due to the rarity of extraosseous odontomas, the diagnosis is usually not considered as a differential diagnosis. According to the literature, intraosseous complex odontomas usually arise in the posterior mandible or maxilla [7] . According to previously reported cases [8] - [16] peripheral odontomas have been described to be most prevalent in the incisor/canine region of the maxilla. Table 1 shows a short review of previous case reports. Another factor that can make it difficult to diagnose is that these entities can be at different stages when it comes to calcification. Three stages have been described [2] . It is not until the third stage that it shows the classical radiographic
Table 1. Summary of clinical and radiological features of previously reported cases of peripheral odontomas, including the present case.
features of the calcified dental tissues. This can make it extremely difficult to identify on a radiographic examination, especially the peripheral type. There also seems to be a lack of consensus in regard to histogenesis of extraosseous odontomas. There are also different theories regarding the specific etiological factors causing the development of extraosseous odontomas, including infection, trauma and genetic factors [17] . In theory, peripheral odontomas may mature over time; eventually erupting into the oral cavity [18] . The clinical characteristics in this case report did not give a lot of information in regards to a definitive diagnosis other than that it was a slow growing fibrous mass and the radiographic examination did not add further information of any value. Therefore, the need for a biopsy is evident since the differential diagnosis according to the primary clinical and radiographic examination was either a peripheral giant cell granuloma or a peripheral ossifying fibroma.
5. Conclusion
The fact that peripheral odontomas are relatively uncommon, as well the fact that the complex type occurs more seldom than the compound type, makes it hard to diagnose clinically. It can appear as in this case, as a fibrous mass in the marginal gingiva where the thought of a peripheral odontoma does not come first to mind as a differential diagnosis. The fact that they can also arise at different stages of calcification can make it hard to diagnose them on a radiographic examination, as it was in this case report. It was very radiolucent and even hard to detect at a closer look. In light of the aforementioned information, the need for biopsy is clear, since you can only gain so much information from the clinical and radiographical aspects.
Funding
None.
Conflict of Interest
Author 1, Gunnar Ingi Jóhannsson declares that he has no conflict of interest. Author 2, Steen Bærentzen declares that he has no conflict of interest. Author 3, Johan Blomlöf declares that he has no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
In relation to publication of this case report and any additional related information, informed consent was given by the patient’s parents.
Pubmed Search
Search text: (((gingiva[Text Word]) OR “Gingiva” [Mesh])) AND ((((hamartoma*[Text Word]) OR “Hamartoma”[Mesh:NoExp]) OR odontoma*[Text Word]) OR “Odontoma”[Mesh]).
This search resulted in 70 articles whereof 5 articles were included. Other case report articles were collected via hand search on the internet and via other references in those articles. This is the base for the making of Table 1.
Cite this paper
Jóhannsson, G.I., Bærentzen, S. and Blomlöf, J. (2017) Peripheral Complex Odontoma in the Gingiva: A Case Report of an 11 Year Old Boy and Review of Literature. Open Journal of Stomatology, 7, 419-427. https://doi.org/10.4236/ojst.2017.79036
References
- 1. Barnes, L., Eveson, J.W., Reichart, P. and Sidransky, D. (2005) World Health Organization Classification of Tumours. Pathology and Genetics of Head and Neck Tumours. IARC Press, Lyon, 310 p.
- 2. Reichart, P.A. and Philipsen, H.P. (2004) Odontogenic Tumors and Allied Lesions. Quintessence Publishing, New Malden, 141-153.
- 3. Buchner, A., Merrell, P.W. and Carpenter, W.M. (2017) Relative Frequency of Central Odontogenic Tumors: A Study of 1088 Cases from Northern California and Comparison to Studies from Other Parts of the World. Journal of Oral and Maxillofacial Surgery, 64, 1343-1352.
- 4. Kintarak, S., Kumplanont, P., Kietthubthew, S. and, Chungpanich, S. (2006) A Nodular Mass of the Anterior Palatal Gingiva. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, 102, 3-6.
- 5. Björk, A., Krebs, A. and Solow, B. (1964) A Method for Epidemiological Registration of Malocclusion. Acta Odontologica Scandinavica, 22, 27-41.
- 6. Lee, C.H. and Park, G.J. (2008) Complex and Compound Odontomas Are Clinico-Pathological Entities. Basic and Applied Pathology, 1, 30-33.
- 7. Gedik, R., Müftüoglu, S., Gedik, R. and Müftüoglu, S. (2014) Compound Odontoma: Differential Diagnosis and Review of the Literature. West Indian Medical Journal, 63, 793-795.
- 8. Ide, F., Mishima, K. and Saito, I. (2008) Rare Peripheral Odontogenic Tumors: Report of 5 Cases and Comprehensive Review of the Literature. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, 106, 22-28.
- 9. Friedrich, R.E., Fuhrmann, A., Scheuer, H.A. and Zustin, J. (2010) Small Peripheral Developing Odontoma of the Maxilla in a 3-Year-Old Patient Depicted on Cone-Beam Tomograms. In Vivo, 24, 895-898.
- 10. Ledesma-Montes, C., Perez-Bache, A. and Garcés-Ortíz, M. (1996) Gingival Compound Odontoma. International Journal of Oral and Maxillofacial Surgery, 25, 296-297.
- 11. Giunta, J. and Kaplan, M. (1990) Peripheral, Soft Tissue Odontomas. Two Case
Reports. Oral Surgery, Oral Medicine, Oral Pathology, 69, 406-411.
https://doi.org/10.1016/0030-4220(90)90312-G - 12. Castro, G., Houston, G. and Weyrauch, C. (1994) Peripheral Odontoma: Report of Case and Review of Literature. American Society of Dentistry for Children, 61, 209-213.
- 13. Koneru, A., Vanishree, M., Surekha, R., Hamsini, A. and Hunasgi, S. (2014) Rare Gingival Odontoma: Report of a Case and Review of Literature. Journal of Dr. NTR University of Health Sciences, 3, 133-135.
https://doi.org/10.4103/2277-8632.134889 - 14. Silva, A.S., Carlos-Bregni, R., Vargas, P. and De Almeida, O. (2009) Peripheral Developing Odontoma in Newborn. Report of Two Cases and Literature Review, 14, 612-615.
- 15. Ide, F., Shimoyama, T. and Horie, N. (2000) Gingival Peripheral Odontoma in an Adult: Case Report. Journal of Periodontology, 71, 830-832.
https://doi.org/10.1902/jop.2000.71.5.830 - 16. Bernardes, V.D.F., Otávio, L., Cota, D.M., Costa, F.D.O., Mesquita, R.A., Gomez, R.S., et al. (2008) Gingival Peripheral Odontoma in a Child: Case Report of an Uncommon Lesion. Brazilian Journal of Oral Sciences, 7, 1624-1626.
- 17. De Oliveira, B.H., Campos, V. and Marcal, S. (2001) Compound Odontoma—Diagnosis and Treatment: Three Case Reports. Pediatric Dentistry, 23, 151-157.
- 18. Hanemann, J.A.C., Oliveira, D.T., Garcia, N.G., Santos, M.R.G. and Pereira, A.A.C. (2013) Peripheral Compound Odontoma Erupting in the Gingiva. Head & Face Medicine, 9, 15.
https://doi.org/10.1186/1746-160X-9-15