Open Journal of Psychiatry
Vol.3 No.1A(2013), Article ID:28064,5 pages DOI:10.4236/ojpsych.2013.31A014
Depression profiles in skin disorders*
![]()
1Department of Human and Social Sciences, University of Messina, Messina, Italy
2Department of Experimental Clinical Medicine, University of Messina, Messina, Italy
3Department of Neurosciences, University of Messina, Messina, Italy
Email: #cmento@unime.it
Received 24 October 2012; revised 26 November 2012; accepted 5 December 2012
Keywords: Depression Profile; Seborrheic Dermatitis; Psoriasis; Emotions
ABSTRACT
Introduction: Dermatological problems often present mood disorders, depression, anxiety disorders and psychological conditions relevant to psychosomatic conditions. Seborrheic dermatitis and psoriasis, both characterized by chronic inflammation of skin, have been linked to emotional states. The aim of our study was to compare the two emotional profiles of patients with seborrheic dermatitis and psoriasis, in order to evaluate, quantitatively and qualitatively, the emotional picture in the two groups of disease. Methods: The study group included 33 patients affected by seborrheic dermatitis (21 males and 12 females, age range 18 - 67 years, mean age 39.85 ± 15.45 years) and 36 other patients affected by psoriasis (22 males and 14 females, age range 18 - 67 years, mean age 41.11 ± 13.72 years). The protocol included clinical assessment of the skin disorder and psychological assessment of emotional profile using the test Profile of Mood States (POMS) and the Toronto Alexithymia Scale TAS-20. An exploratory factorial analysis was carried out for the POMS factor D (depression) to evaluate the composition of the items found in the two types of skin disorders. Results: The comparison between patients with psoriasis and patients with seborrheic dermatitis in relation to the TAS score and the different aspects of mood and showed a significant difference concerning factor D (depression) of the POMS. Conclusions: This study shows the correlation between depression and two skin disorders, seborrhoeic dermatitis and psoriasis. In both cases, the clinical picture falls under the definition of “depression due to a general medical condition”. However, qualitative differences make the psychologic frame of psoriatic patients close to that of “major depression”, while in patients affected by seborrheic dermatitis the psychologic frame is more similar to that of “minor depression” (DSM IV).
1. INTRODUCTION
Psychosomatic skin disorders are those in which the etiopathogenesis of cutaneous alterations can be traced to a substantial extent to psychological factors [1].
Patients with dermatological problems often present mood disorders (mainly depression), anxiety disorders and psychological conditions relevant to psychosomatic conditions such as demoralisation, irritability and type A behaviour. Many studies have highlighted the comorbidity of skin disorders and depression, occurring in 25% - 30% of the cases examined, a considerably higher rate than that found in the general population [2-4].
The literature suggests that depression is one of the most common psychiatric disorders in dermatological diseases, but that it is diagnosed in a purely generic sense. Indeed, all previous studies investigated only the presence or absence of depression, or, at best, evaluated this disorder quantitatively [5,6]. In contrast, the organization of emotions is qualitatively different, in the composition of the clinical framework, between groups of skin disorders, and the difference in this organization appears even if subjects do not manifest a specific clinical disease, as in cases of “subthreshold depression” [7].
Seborrheic dermatitis and psoriasis, both characterized by chronic inflammation of skin with erythema and desquamation, have been linked to emotional states [8,9].
A few studies have investigated seborrheic dermatitis from a psychological perspective, showing that 76% of patients report stress, depression and fatigue to be the factors triggering the onset of the disease [10].
Some studies have focused on the causal link between inflammation and emotional stress [11,12]. Evidence supporting the correlation between mood and seborrheic dermatitis is provided by studies that show a high incidence of this disease in psychiatric patients suffering from depression or other diagnostic frames, e.g. anxiety, hostility and somatization [13]. Psoriasis has also been found to be correlated with emotional state. Recent research has confirmed that about half of psoriatic patients report a stressful event in the six months prior to the onset of the disease, and have high levels of anxiety [14- 16].
Data from literature show that psoriasis has a significant impact on the emotional state of patients, particularly for which concerns self-esteem and body image, resulting in feelings of shame and embarrassment [9]. A significant correlation was found between psoriasis and depressive disorders [8]; however, no correlation was found between the severity of depressive disorders (present in about 20% of patients) and the PASI (Psoriasis Area and Severity Index) score or the intensity of the stressful experience [17-20].
The aim of our study was to compare the emotional profile of patients with seborrheic dermatitis and patients with psoriasis, in order to evaluate, not only quantitatively but also qualitatively, the emotional picture in the two groups.
2. MATERIALS AND METHODS
2.1. Study Population
Outpatients of the Dermatology Unit of the University Hospital of Messina aged 18 years or more and diagnosed with either seborrheic dermatitis or psoriasis were enrolled in the study. Exclusion criteria were other relevant cutaneous or systemic diseases. Each subject was briefed on the procedure and about the aim of the study, and gave consent to take part in it.
The study group included 33 patients affected by seborrheic dermatitis (21 males and 12 females, age range 18 - 67 years, mean age 39.85 ± 15.45 years) and 36 other patients affected by psoriasis (22 males and 14 females, age range 18 - 67 years, mean age 41.11 ± 13.72 years).
2.2. Assessment Instruments
The protocol included clinical assessment of the skin disorder carried out by a dermatologist and psychological assessment of emotional profile using the test Profile of Mood States (POMS) and the Toronto Alexithymia Scale TAS-20 [21,22].
Severity of psoriasis was evaluated using the PASI score, which gives an overall estimate of the extent and intensity of lesions over the entire skin surface. The severity of seborrheic dermatitis was assessed using an ad hoc score for erythema, desquamation and itching. In detail, a score from 0 (absent) to 3 (severe) was given for erythema, desquamation or itching involving seven areas: scalp, upper, middle and lower third of face, retroauricular area, sternal area, interscapular area. The final severity score for seborrheic dermatitis was the sum of all the above partial scores. Since different score ranges were used in the assessment scales for psoriasis and seborrheic dermatitis (0 - 72 for PASI, and 0 - 63 for seborrheic dermatitis), the results were converted onto a scale from 0 to 100 prior to statistical analysis.
POMS is a test which identifies and quantifies affective states. Respondents are asked to indicate their mood over the previous week by rating each of the 58 items on a score from 0 to 4. The result is a profile containing six factors: T (Tension-Anxiety), D (Depression-Dejection), A (Anger-Hostility), V (Vigour-Activity), F (FatigueInertia), C (Confusion-Bewilderment).
TAS-20 is a self-assessment scale containing 20 items scored from 1 to 5. A total score of 61 or more indicates the presence of alexithymia. The study protocol was approved by the Ethics Committee of the University Hospital of Messina.
2.3. Statistical Analysis
Data were analyzed using the SPSS software version 16.0 (SPSS Inc. Chicago, USA). All variables were subject to descriptive analysis and the averages (due to the non homogeneity of variances) were subjected to the non parametric Mann-Whitney test.
An exploratory factorial analysis was carried out for the POMS factor D (depression) to evaluate the composition of the items found in the two types of skin disorders. A KMO (Kaiser-Meyer-Olkin) test was carried out beforehand to assess sampling adequacy (best >0.600).
3. RESULTS
Table 1 presents the socio-demographic characteristics of the patients in the two groups.
The comparison between patients with psoriasis and patients with seborrheic dermatitis in relation to the TAS score and the different aspects of mood (tension, depression, anger, vigour, fatigue and confusion) showed a significant difference concerning factor D (depression), which is more frequently accentuated and, on average, higher in the group of patients with psoriasis than in the other group (Table 2).
We therefore wished to examine the items making up the factor “depression” in POMS (i.e. Unhappy, Discontent, Melancholy, Sad, Without hope, Unworthy, Discouraged, Lonely, Dejected, Very bad mood, Disheartened, Without help, Worthless, Terrified, Sorry for things done) to delineate the composition of this factor in each of the two groups. We decided to use factorial analysis to achieve this goal [23]. The KMO test for the measure of sampling adequacy was 0.644 (best >0.600) The results proved the adequacy of the distribution, allowing us to proceed with the exploratory factorial analysis. The comparison of the answers given to the items under POMS D between the two groups showed significant
Table 1. Socio-demographic characteristics of the study population.
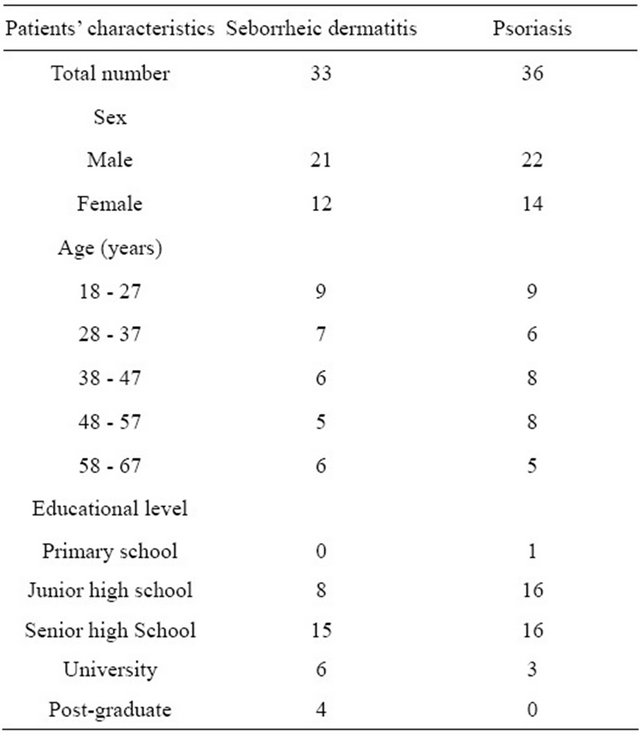
Table 2. Results of the Mann-Whitney U test on TAS-20 and POMS scores of patients affected by seborrheic dermatitis or psoriasis.
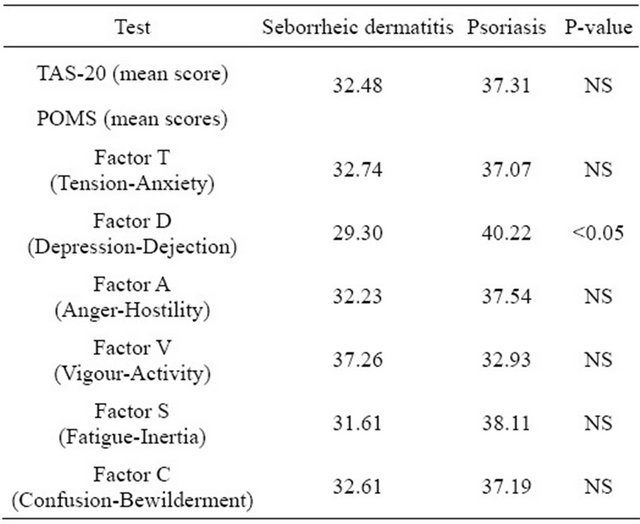
NS = not significant.
difference as regards item 18 (“without hope”) and a slightly smaller although still significant difference regarding item 42 (“without help”): in both cases, scores of psoriatic patients were higher than those of patients with seborrheic dermatitis (Table 3).
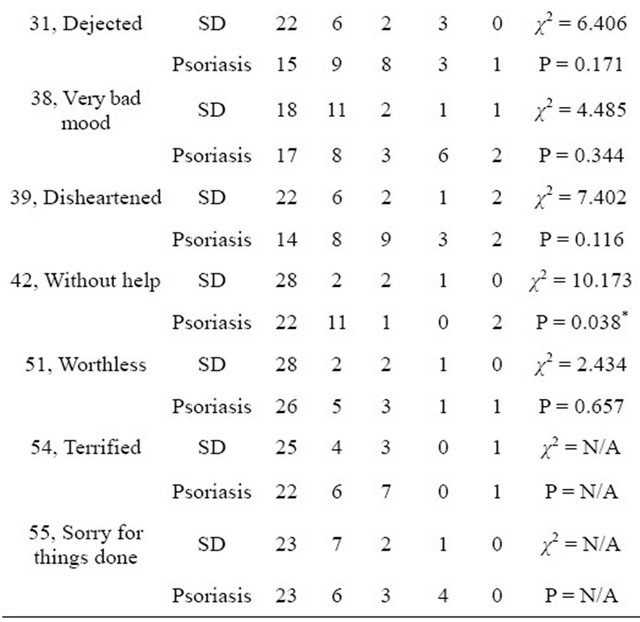
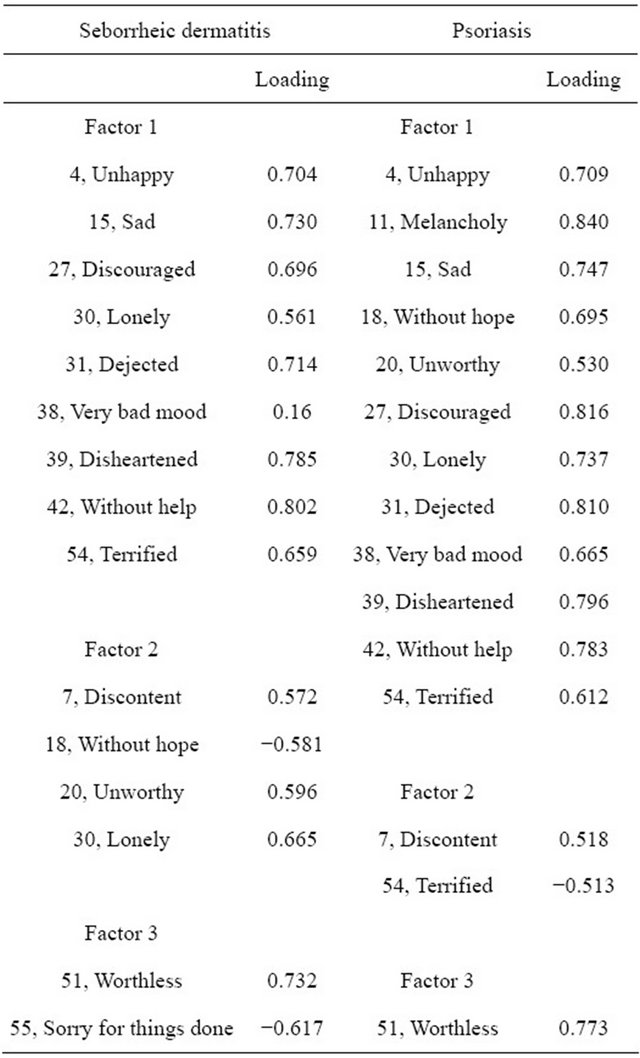
Examination of the three main factors emerging from patients affected by seborrheic dermatitis or psoriasis revealed that the two depression profiles were different (Table 4).
Table 3. Answers given by patients with seborrheic dermatitis or psoriasis to POMS D items (items of POMS pertaining to the “depression” factor).
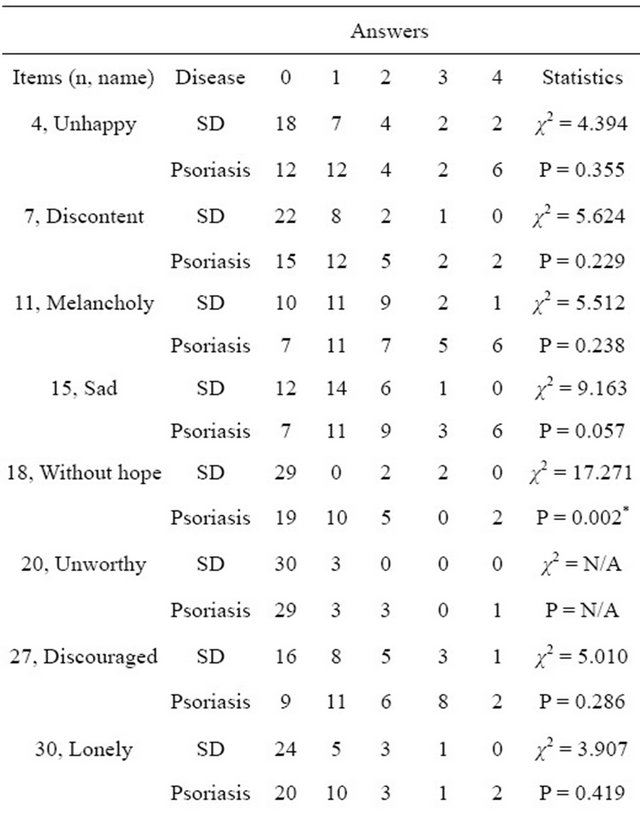
* = statistically significant difference (p < 0.05); SD = seborrheic dermatitis; N/A = non-significant difference, exact calculation is not possible because, in at least one case in the contingency table, matching cells of the two groups (SD and psoriasis) contain both zero.
No correlation was found between the severity of the patients’ clinical picture and level of depression (POMS D), other POMS factors or the scores on the TAS-20 test.
Table 4. Factor analysis of the items of the factor depression of POMS in patients affected by seborrheic dermatitis or psoriasis.
4. DISCUSSION
The results of the analysis of the variables showed a statistically significant result in relation to POMS factor D (depression) for both the skin disorders examined. In detail, the analysis of the variables making up factor D of POMS revealed a difference between the two groups in relation to items 18 (“without hope”) and 42 (“without help”). This highlights the difference between the two groups as regards the intensity of feelings of depression, that were found to be more severe in the case of psoriasis.
The factorial analysis of factor D of POMS allowed to detect qualitative differences in the composition of the items between the two skin disorders, in particular in relation to the variables “melancholy”, “without hope” and “unworthy” that occur together in the case of psoriasis. This underlines that in this disease the expression of depression contains many of the core symptoms of depression and thus is clinically closer to that of “major depression” [24]. In contrast, the depression manifested by seborrheic dermatitis patients is closer to the clinical frame of “minor depression” (see Factor 1 in Table 4).
The other two factors shown in Table 4 strenghten this line of reasoning, because the feeling of “without hope”, which lies at the core of depressive conditions, is found in the psoriasis group (see composition of Factor 1) but not in the seborrheic dermatitis group.
The feeling of being “without hope” is inversely correlated to the variables “discontent” and “unworthy” in patients affected by seborrhoeic dermatitis (Factor 2, Table 4). Conversely, in psoriatic patients “discontent” is inversely correlated to “terrified”, that indicates, by definition, an emotional state that is more archaic and more severe than the feeling of being “without hope” found in the clinical picture of seborrhoeic dermatitis.
This study shows the correlation between depression and two skin disorders, seborrhoeic dermatitis and psoriasis. In both cases, the clinical picture falls under the definition of “depression due to a general medical condition”. However, qualitative differences make the psychologic frame of psoriatic patients close to that of “major depression”, while in patients affected by seborrheic dermatitis the psychologic frame is more similar to that of “minor depression” [24]. Furthermore, the findings of this preliminary study prompt some considerations regarding the different composition of the depression manifested by patients suffering from two dermatological conditions.
This evaluation is clearly epidemiologic, and does not consider the etiopathogenesis of the two cutaneous diseases. Based on the criteria of clinical epidemiology, our study suggests that, in a therapeutic perspective, psychopharmacological support could be useful in the treatment of psoriasis, psychological support for patients affected by seborrheic dermatitis.
![]()
![]()
REFERENCES
- Consoli, S.G. (1995) La dermatologie psychosomatique. Revue Française d’Allergologie et d’Immunologie Clinique, 35, 621-624.
- Picardi, A., Pasquini, P., Abeni, D., Fassone, G., Mazzotti, E. and Fava, G.A. (2005) Psychosomaticassessment of skin diseases in clinical practice. Psychotherapy and Psychosomatics, 74, 315-322. doi:10.1159/000086323
- Picardi, A., Mazzotti, E., Gaetano, P., Cattaruzza, M.S.,. Baliva, G., Melchi, C.F., Biondi, M. and Pasquini, P. (2005) Stress, social support, emotional regulation, and exacerbation of diffuse plaque psoriasis. Psychosomatics, 46, 556-564. doi:10.1176/appi.psy.46.6.556
- Filakovic, P., Petek, A., Koic, O., Radanovic-Grguric, L. and Degmecic, D. (2009) Comorbidity of depressive and dermatologic disorders: Therapeutic aspects. Psychiabtria Danubina, 21, 401-410.
- Akay, A., Pekcanlar, A., Bozdag, K.E., Altintas, L. and Karaman, A. (2002) Assessment of depression in subject with psoriasis vulgaris and lichen planus. Journal of the European Academy of Dermatology and Venereology, 16, 347-352. doi:10.1046/j.1468-3083.2002.00467.x
- Consoli, S.M., Rolhion, S., Martin, C., Ruel, K., Cambazard, F., Pellet, J. and Misery, L. (2006) Low levels of emotional awareness predict a better response to dermatological treatment in patients with psoriasis. Dermatology, 212, 128-136. doi:10.1159/000090653
- Geiselmann, B. and Bauer, M. (2000) Subthreshold depression in the elderly: Qualitative or quantitative distinction? Comprensive Psychiatry, 41, 32-38. doi:10.1016/S0010-440X(00)80006-1
- Gupta, A.K. and Bluhm, R. (2004) Seborrheic dermatitis. Journal of the European Academy of Dermatology and Venereology, 18, 13-26. doi:10.1111/j.1468-3083.2004.00693.x
- Fortune, D.G., Main, C.J., O’ Sullivan, M.O. and Griffiths, C.E. (1997) Assessing illness-related stress in psoriasis: The psychometric properties of the psoriasis life stress inventory. Journal of Psychosomatic Research, 42, 467-475. doi:10.1016/S0022-3999(97)00036-6
- Peyrì, J., Lleonart, M., Grupoespañol del Estudio SEBDERM. (2007) Clinical and therapeutic profile and quality of life of patients with seborrheic dermatitis. Actas Dermo-Sifiliográficas, 98, 476-482.
- Schwartz, R.A., Janusz, C.A. and Janniger, C.K. (2006) Seborrheic dermatitis: An overview. American Family Physician, 74, 125-130.
- Maietta, G., Fornaro, P., Rongioletti, F. and Rebora, A. (1990) Patients with mood depression have a high prevalence of seborrhoeic dermatitis. Acta Dermato Venereologica, 70, 432-434.
- Oztas, P., Calikoglu, E. and Cetin, I. (2005) Psychiatric tests in seborrhoeic dermatitis. Acta Dermatologica Venereologica, 85, 68-69.
- O’Leary, C.J., Creamer, D., Higgins, E. and Weinman, J. (2004) Perceived stress, stress attributions and psychological distress in psoriasis. Journal of Psychosomatic Research, 57, 465-471. doi:10.1016/j.jpsychores.2004.03.012
- Vargas Laguna, E., Peña Payero, M.L. and Vargas Màrquez, A. (2006) Influence of anxiety in diverse cutaneous diseases. Actas Dermosifiliogr, 97, 637-643.
- Gupta, M.A., Schork, N.J., Gupta, A.K., Kirkby, S. and Ellis, C.N. (1993) Suicidal ideation in psoriasis. International Journal of Dermatology, 32, 188-190.
- Pacan, P., Szepietowski, J.C. and Kiejna, A. (2003) Stressful life events and depression in patients suffering from psoriasis vulgaris. Dermatology and Psychosomatics, 4, 142-145. doi:10.1159/000073990
- Richards, H.L., Fortune, D.G., Griffiths, C.E. and Main, C.J. (2005) Alexithymia in patients with psoriasis: Clinical correlates and psychometric properties of the Toronto Alexithymia Scale-20. Journal of Psychosomatic Research, 58, 89-96. doi:10.1016/j.jpsychores.2004.03.009
- Fortune, D.G., Richards, H.L. and Griffiths, C.E. (2005) Psychologic factors in psoriasis: Consequences, mechanisms and interventions. Dermatologic Clinics, 24, 681- 694. doi:10.1016/j.det.2005.05.022
- McNair, D.M., Lorr, M. and Droppleman, L.F. (1981) Manual for the profile of mood states. EdITS Educational and Industrial Testing Service, San Diego.
- Bagby, R.M., Parker, J.D. and Taylor, G.J. (1994) The twenty-item Toronto Alexithymia Scale-I: Item selection and cross-validation of the factor structure. Journal of Psychosomatic Research, 38, 23-32. doi:10.1016/0022-3999(94)90005-1
- Bressi, C., Taylor, G.J., Parker, J.D., Bressi, S., Brambilla G., Aguglia, E., Bucca, M., Todarello, O., Callegari C., Vender, S., Gala C. and Invernizzi, G. (1996) Cross validation of the factor structure of the 20-item Toronto Alexithymia Scale: An Italian multicenter study. Journal of Psychosomatic Research, 41, 551-559. doi:10.1016/S0022-3999(96)00228-0
- Benazzi, F. (2001) Factor analysis of the Montgomery Asberg depression rating scale in 251 bipolar II and 306 unipolar depressed outpatients. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 25, 1369- 1376. doi:10.1016/S0278-5846(01)00190-7
- AA.VV. Diagnostic and statistical manual (DSM) version IV TR. (1994) American Psychiatric Association.
NOTES
*Funding sources: None.
Conflict of interest: All authors declare that they have no conflict of interest.
#Corresponding author.

