Open Journal of Preventive Medicine
Vol.4 No.4(2014), Article ID:44708,7 pages DOI:10.4236/ojpm.2014.44023
The Burden of Diabetes in a Developing Country
Mohammad Khajedaluee1, Maliheh Dadgarmoghaddam1*, Reza Saeedi1, Zahra Izadi-Mood2, Maryam Abrishami2
1School of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran
2Health Department, Mashhad University of Medical Sciences, Mashhad, Iran
Email: *maliheh_dadgar@yahoo.com
Copyright © 2014 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/


Received 28 January 2014; revised 28 February 2014; accepted 22 March 2014
ABSTRACT
Introduction: People with diabetes often develop diverse microvascular, macrovascular, and neuropathic complications. Diabetes named high disease because of its high prevalence, high incidence, chronicity and high costs. Accurate projections of diabetes burden are essential for health planning so the aim of this study was to calculate the burden of diabetes in Razavikhorasan population, in Iran. Methodology: We used Disability Adjusted Life Years (DALYs) index using computer model (DisMod) for assessment of burden of diabetes and complications in Razavikhorasan province in Iran in year 2010-2011. Results: Burden of diabetes in Razavikhorasan population was 64,733 DALY in year 2010-2011. The total Years Life Lost (YLL) from diabetes mellitus was 62,883 (34,216 in men and 28,667 in women) due to premature death and the total Years Life Disability (YLD) was 1850. Conclusion: Diabetes mellitus and lesser forms of glucose intolerance can now be found in almost every population and epidemiological evidences suggest that, without effective prevention and control programs, diabetes will continue to increase and therefore advances in all levels of prevention may help reduce the number of people with diabetes.
Keywords
Burden of Diabetes; DisMod; YLL; YLD; DALYs; Iran

1. Introduction
Diabetes was first described with the symptoms of polyuria, polydipsia, and polyphagia [1] .
Diabetes mellitus is a metabolic disease characterized by hyperglycemia and classified into four types: type 1diabetes, type 2 diabetes, gestational diabetes, and other specific types [2] [3] . Uniform diagnostic criteria for diabetes were first recommended by the American Diabetes Association and the World Health Organization (WHO) in 1979 and 1980 and were updated in the late 1990s [4] [5] . According to the American Diabetes Association criteria, diabetes is defined as Hb A1C ≥ 6.5%, Fasting Plasma Glucose (FPG) ≥ 126 mg/dl and Oral Glucose Tolerance Test (OGTT) ≥ 200 mg/dl [6] .
People with diabetes often develop different microvascular, macrovascular, and neuropathic complications [7] . Diabetes named high disease because of its high prevalence, high incidence, chronicity and high costs [8] [9] . In 1993, the WHO Diabetes Reporting Group published standardized global estimates for the prevalence of diabetes and impaired glucose tolerance in adults [10] . These results suggest that prevalence of diabetes in adults will increase by 35%, and the number of people with diabetes will increase by 122% in the world from 1995 to 2025.In developed countries, the number of diabetic people will increase by 42% while in developing countries; it will be 170% [11] . Currently the lowand middle-income countries face the greatest burden of diabetes. Diabetes is the fourth or fifth leading cause of death in most high-income countries and it is epidemic in many low and middle income ones [12] .
McCarty et al. estimated that the global burden of diabetes was 110 million in 1994 and it would be 239 million by 2010 [13] . WHO also estimated the global burden at 135 million in 1995, with the number reaching 299 million by the year 2025 [14] . Five recent studies emphasize on the prevalence and national economic burden of diabetes [15] -[20] . Different diseases have different burden of disease (BoD) that we can measure it by some indicators like DALYs. DALYs are the sum of two dimensions: the years life lost (YLL), and the number years of life lived with a disability (YLD) [21] .
Accurate projections of diabetes burden are essential to policymakers to plan health care services while planners are still unaware of the current situation of burden of diabetes in their countries. Therefore, this study was planned to calculate the burden of diabetes for the population of Razavikhorasan province in Iran.
2. Methods
For calculating the burden of disease, we need to know the demographic characteristics of target population such as age, sex, and general mortality rate according to age and sex.
Our target population in this study was the total population of Razavikhorasan province in 2010-2011which was 5,865,866 (2,919,443 females and 2,946,423 males). Although the disease burden is calculated at a national level, but due to the high population in Razavikhorasan province, the diabetes burden was calculated separately for this province.
Also, we should access to disease morbidity (incidence, prevalence, disease duration, remission rate) and mortality (disease specific death rate, fatality rate, and relative death rate) data. We used Disease Modeling (Dismode) software version II for analyzing data. This software is capable to calculate the intended parameters by at least three out of seven main indicators of morbidity and mortality that mentioned above. Then, The software outputs are entered to the Template designed by the World Health Organization and burden indicators (YLL and YLD) are calculated. To calculate the burden of diabetes three indicators were used: prevalence, Cause Specific Mortality, and Remission Rate.
To determine the prevalence rate, available data in the three population based study in Mashhad, Razavikhorasan Province were used. The first study was surveillance of risk factors for noncommunicable diseases in 2007, which data were analyzed by SPSS software and the prevalence of diabetes were calculated by age and sex. The second study was investigating the prevalence of diabetes in Mashhad population and prevalence of diabetes was calculated by age and sex using SPSS software. Another source of data was diabetes surveillance system in urban and rural area in Razavikhorasan province which was collected and recorded by noncommunicable and communicable diseases health department. Ultimately based on these studies, the prevalence of diabetes was estimated by age and sex.
Disease-specific mortality was obtained from cause of death registry in statistics unit at the Health Department. In reviewing the records, the number of registered deaths due to diabetes appeared to be invalid. Therefore, for a more accurate calculation of diabetic deaths, the World Health Organization estimation of the relative risk of mortality in diabetic patients by sex was replaced. Considering that diabetes is not curable disease, the Remission Rate was zero for both sexes and all ages. Baseline population information was based on census data collected by statistics unit at Health department. Three mentioned parameters data entered to DisMod version II software according to sex and age and output indicators, including 7 disease morbidity and mortality indicators were extracted.
The DisMod output data entered in to the YLD and YLL Template and these two indicators for burden of diabetes are calculated. DALYs presented in this study are age weighted (β = 0.04) and are discounted for time preference (r = 0.03). For calculating the YLL, the life expectancy is considered 82.5 years for females and 80 years for males. In this study the diagnosis of diabetes made with a fasting plasma glucose level of 7.0 mmol/L (126 mg/dl) and higher or impaired glucose tolerance test 100 - 125 mg/dl.
3. Results
Prevalence of diabetes and impaired glucose tolerance in the studied population are presented in Figure 1 and Figure 2 according to sex. The prevalence was, 8.9% in men and 9.1% in women, which is equivalent to the
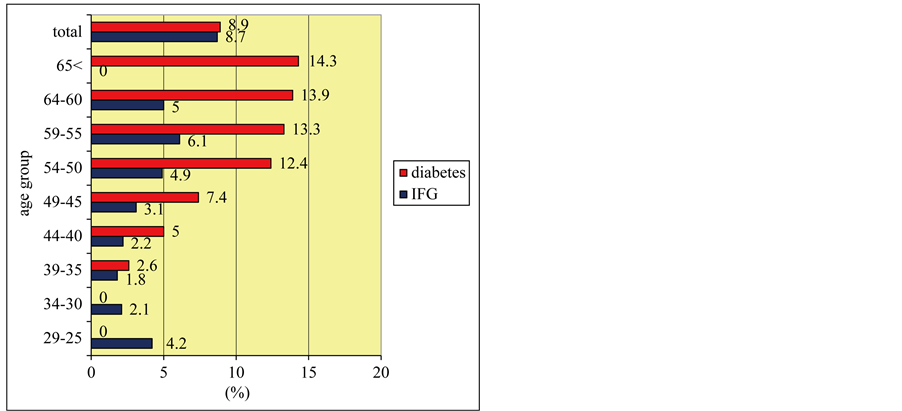
Figure 1. Prevalence of diabetes and impaired glucose tolerance in men according to age group in Razavikhorasan province, 2010-2011.
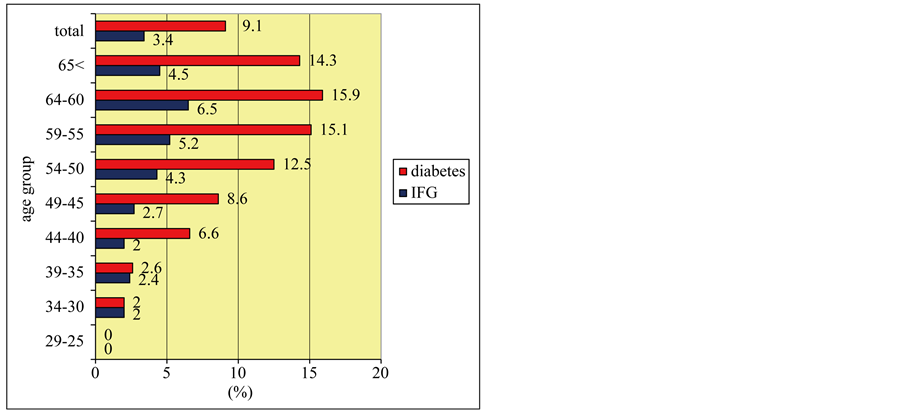
Figure 2. Prevalence of diabetes and impaired glucose tolerance in women according to age group in Razavikhorasan province, 2010-2011.
global estimated prevalence for 2030.
Number of years life lost because of premature death from diabetes according to age group is shown in Figure 3.
The numbers of years lost to disability are presented in Figure 4. The total YLD was 1850 .The highest YLD was in the 45 - 59 age-group.
The total burden of diabetes is presented in Figure 5 according to the sex. The number of years life lost due to premature death or disability from diabetes was 64733 DALY which the highest proportion burden of disease was in the 45 - 59 age-group.
4. Discussion
Two important points should be noted. First, the prevalence of diabetes in Razavikhorasan population is higher than the global and regional estimates (14% - 16% in the age 50 - 60). Secondly, it seems that the age of onset of diabetes was reduced to 30s. The prevalence estimates of diabetes mellitus in Iran in 2030, is 9.3% at national level [20] . The prevalence of diabetes varies between ethnic groups [22] -[25] and is influenced by genetic, environmental, social, and cultural factors [26] -[31] .
In this study, the total YLL from diabetes was 62,883 (34,216 in men and 28,667 in women) because of premature death. It is highly important to notice that the most of the YLL (27%) has occurred between the ages of 45 to 59 that is an active age. In Abolhasani et al. study in Iran, burden of diabetes was 306,440 years in 2000. Burden of diabetic retinopathy, nephropathy, neuropathy, diabetic foot and lower limb amputation were 20,532, 20,532, 33,286, 5848 and 1573 years, respectively [32] .
Diabetes is already recognized as a public health problem of pandemic proportions [33] . In a study about projection of diabetes burden in the US indicated that the situation may be more alarming than previously believed [34] . In 2007, diabetes cost the US in excess of $174 billion [35] .
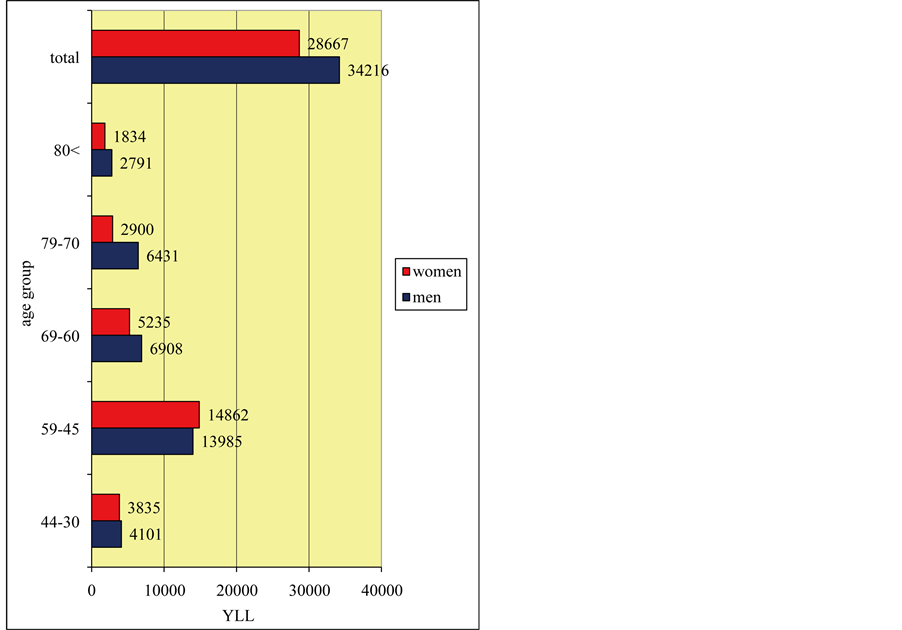
Figure 3. Number of years life lost due to premature death from diabetes, by sex and age group in Razavikhorasan province, 2010-2011.

Figure 4. Number of years lost to disability from diabetes, by sex and age group in the Razavikhorasan province, 2010-2011.
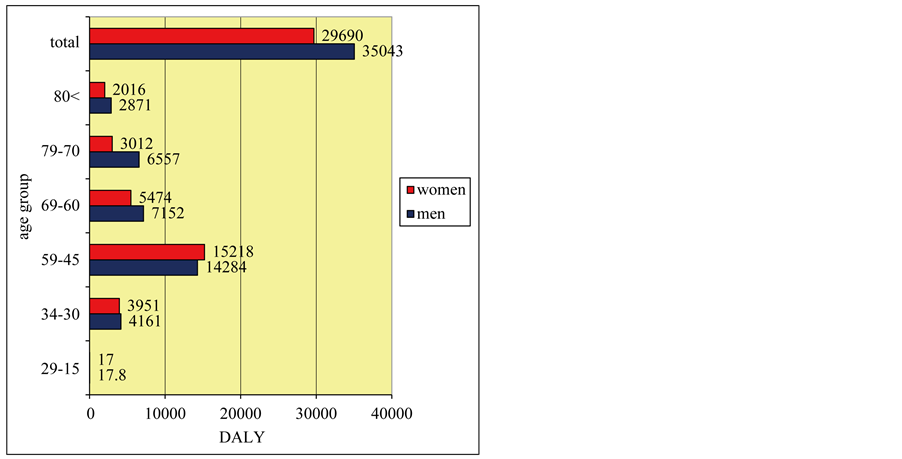
Figure 5. Disability adjusted life years according to age and sex in Razavikhorasan province, 2010-2011.
5. Conclusions
Trend data suggest that the burden will continue to increase and diabetes is certainly one of the most challenging health problems in the 21st century. Advances in primary prevention may help reduce the number of people with diabetes [36] .
It will be important to utilize available data to monitor changes in incidence, prevalence, burden of disease and economic outcomes. It was suggested that through regular analysis of available data sources, interventions can be better designed such as essential, primary, secondary and tertiary prevention. So it is recommended that population based data registry should be constructed and improved to specify health care priorities to decrease the burden of diabetes in Iran and other developing countries.
Acknowledgements
With special thanks to, Maziar Moradi-Lakeh, Majid Ghayour Mobarhan, Mohammad Reza joya, Gholam Hossein Khodaee, Babak Eghbali and Mohammad Hossein Ghoorchi.
Conflict of Interest Statement
The authors declare that there are no conflicts of interest.
Limitations
The population based data registry did not have comprehensive information resulted in difficulties to extract accurate data which was explained previously.
References
- Hazlett, B.E. (2000) Historical Perspective: The Discovery of Insulin. In: Davidson, J.K., Ed., Clinical Diabetes Mellitus: A Problem-Oriented Approach, Thieme, New York, 3-11.
- American Diabetes Association (2008) Standards of Medical Care in Diabete. Diabetes Care, 31, S12-S54. http://dx.doi.org/10.2337/dc08-S012
- World Health Organization (1994) Prevention of Diabetes Mellitus. Technical Report Series No. 844. World Health Organization, Geneva.
- (1997) Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care, 20, 1183-1197.
- Alberti, K.G. and Zimmet, P.Z. (1998) Definition, Diagnosis and Classification of Diabetesmellitus and Its Complications. Part 1: Diagnosis and Classification of Diabetes Mellitus Provisional Report of a WHO Consultation. Diabetic Medicine, 15, 539-553. http://dx.doi.org/10.1002/(SICI)1096-9136(199807)15:7<539::AID-DIA668>3.0.CO;2-S
- American Diabetes Association (2010) Diagnosis and Classification of Diabetes Mellitus. Diabetes Care, 33, S62-S69.
- Wallace, R. (2008) Public Health & Preventive Medicine.15 Edition, McGrawHill, USA, 10.
- Engelgau, M.M., Geiss, L.S., Saaddine, J.B., Boyle, J.P., Benjamin, J.M., Gregg, E.W., Tierney, E.F., Rios-Burrows, N., Mokdad, A.H., Ford, E.S., Imperatore, G. and Narayan, K.M.V. (2004) The Evolving Diabetes Burden in the United States. Annals of Internal Medicine, 140, 945-950. http://dx.doi.org/10.7326/0003-4819-140-11-200406010-00035
- Zimmet, P.Z., Alberti, K.G. and Shaw, J.E. (2001) Global and Societal Implications of the Diabetes Epidemic. Nature, 414, 782-787. http://dx.doi.org/10.1038/414782a
- King, H. and Rewers, M. (1993) WHO Ad Hoc Diabetes Reporting Group: Global estimates for Prevalence of Diabetes and Impaired Glucose Tolerance in Adults. Diabetes Care, 16, 157-177. http://dx.doi.org/10.2337/diacare.16.1.157
- King, H., Aubert, R.E. and Herman, W.H. (1996) Global Burden of Diabetes, 1995-2025 Prevalence, Numerical Estimates, and Projections. Diabetes Care, 21, 1414-1431.
- Sicree, R., Shaw, J. and Zimmet, P. (2009) The Global Burden, Diabetes and Impaired Glucose Tolerance. IDF Diabetes Atlas Fourth Edition, Baker IDI Heart and Diabetes Institute.
- McCarty, D. and Zimmet, P. (1994) Diabetes 1994 to 2010: Global Estimates and Projections. International Diabetes Institute, Melbourne.
- King, H., Aubert, R. and Herman, W. (1998) Global Burden of Diabetes, 1995-2025: Prevalence, Numerical Estimates and Projections. Diabetes Care, 21, 1414-1431. http://dx.doi.org/10.2337/diacare.21.9.1414
- American Diabetes Association (2008) Economic Costs of Diabetes in the US in 2007. Diabetes Care, 31,576-615.
- Dall, T.M., Mann, S.E., Zhang, Y., Quick, W.W., Seifert, R.F., Martin, J., et al. (2009) Distinguishing the Economic Costs Associated with Type 1 and Type 2 Diabetes. Population Health Management, 12, 103-110. http://dx.doi.org/10.1089/pop.2009.12203
- Zhang, Y., Dall, T.M., Mann, S.E., Chen, Y., Martin, J., Moore, V., et al. (2009) The Economic Costs of Undiagnosed Diabetes. Population Health Management, 12, 95-101. http://dx.doi.org/10.1089/pop.2009.12202
- Zhang, Y., Dall, T.M., Chen, Y., Baldwin, A., Yang, W., Mann, S., et al. (2009) Medical Cost Associated with Prediabetes. Popul Health Manag, 12, 157-163. http://dx.doi.org/10.1089/pop.2009.12302
- Chen, Y., Quick, W.W., Yang, W., Zhang, Y., Baldwin, A., Moran, J., et al. (2009) Cost of Gestational Diabetes Mellitus in the United States in 2007. Population Health Management, 12, 165-174. http://dx.doi.org/10.1089/pop.2009.12303
- Shaw, J.E., Sicree, R.A. and Zimmet, P.Z. (2009) Global Estimates of the Prevalence of Diabetes for 2010 and 2030. Diabetes Research and Clinical Practice, 87, 4-14. http://dx.doi.org/10.1016/j.diabres.2009.10.007
- World Health Organization. Global Burden of Disease (2004) Update. Geneva: World Health Organization. http://www.who.int/healthinfo/global_burden_disease/GBD_report_2004update_full.pdF
- Khattar, R.S., Swales, J.D., Senior, R. and Lahiri, A. (2000) Racial Variation in Cardiovascular Morbidity and Mortality in Essential Hypertension. Heart, 83, 267-271. http://dx.doi.org/10.1136/heart.83.3.267
- Chaturvedi, N., Jarrett, J., Morrish, N., Keen, H. and Fuller, J.H. (1996) Differences in Mortality and Morbidity in African Caribbean and European People with Non-Insulin-Dependent Diabetes Mellitus: Result of 20-Year Follow-Up of a London Cohort of a Multinational Study. BMJ, 313, 848-852. http://dx.doi.org/10.1136/bmj.313.7061.848
- U.K. Prospective Diabetes Study Group (1998) The Incidence of Myocardial Infarction in White, South Asian, and Afro-Caribbean Patients with Type 2 Diabetes (U.K. Prospective Diabetes Study 32). Diabetes Care, 21, 1271-1277. http://dx.doi.org/10.2337/diacare.21.8.1271
- Balarajan, R. (1996) Ethnicity and Variations in Mortality from Coronary Heart Disease. Health Trends, 28, 45-51.
- Joffe, B. and Zimmet, P. (1998) The Thrifty Genotype in Type 2 Diabetes: An Unfinished Symphony Moving to Its Finale? Endocrine, 9, 139-141. http://dx.doi.org/10.1385/ENDO:9:2:139
- Bhopal, R., Unwin, N., White, M., et al. (1999) Heterogeneity of Coronary Heart Disease Risk Factors in Indian, Pakistani, Bangladeshi, and European Origin Populations: Cross-Sectional Study. BMJ, 319, 215-220. http://dx.doi.org/10.1136/bmj.319.7204.215
- Sundquist, J. and Winkleby, M. (2000) Country of Birth, Acculturation Status and Abdominal Obesity in a National Sample of Mexican-American Women and Men. International Journal of Epidemiology, 29, 470-477. http://dx.doi.org/10.1093/ije/29.3.470
- Zimmet, P. (1982) Type 2 (Non-Insulin-Dependent) Diabetes—An Epidemiological Overview. Diabetologica, 22, 399-411. http://dx.doi.org/10.1007/BF00282581
- Cappucio, F.P., Cook, D.G., Atkinson, R.W. and Strazullo, P. (1997) Prevalence, Detection, and Management of Cardiovascular Risk Factors in Different Ethnic Groups in South London. Heart, 78, 555-563.
- Abate, N. and Chandalia, M. (2003) The Impact of Ethnicity on Type 2 Diabetes. Journal of Diabetes and Its Complications, 17, 39-58. http://dx.doi.org/10.1016/S1056-8727(02)00190-3
- Abolhasani, F., Tehrani, M.R.M., Tabatabaei, O. and Larijani, B. (2005) Burden of Diabetes and Its Complications in Iran in Year 2000. JDMD, 5, 130.
- Narayan, K.M.V., Gregg, E.W., Fagot-Campagna, A., Engelgau, M.M. and Vinicor, F. (2000) Diabetes—A Common, Growing, Serious, Costly, and Potentially Preventable Public Health Problem. Diabetes Research and Clinical Practice, 50, Suppl. 2, 77-84. http://dx.doi.org/10.1016/S0168-8227(00)00183-2
- Boyle, J.P., Thompson, T.J., Gregg, E.W., Barker, L.E. and Williamson, D.F. (2010) Projection of the Year 2050 Burden of Diabetes in the US Adult Population: Dynamic Modeling of Incidence, Mortality, and Prediabetes Prevalence. Population Health Metrics, 8, 29. http://dx.doi.org/10.1186/1478-7954-8-29
- American Diabetes Association (2008) Economic Costs of Diabetes in the U.S. in 2007. Diabetes Care, 32, 596-615.
NOTES

*Corresponding author.

