 Vol.3, No.7, 467-476 (2011) doi:10.4236/health.2011.37077 Copyright © 2011 SciRes. Openly accessible at http://www.scirp.org/journal/HEALTH/ Health Effect of vitrification procedure on chromosomal s tatus of embryos achieved from vitrified and fresh oocytes Javier Israel García*, Luis Nori ega-Portel la, Luis Noriega-Ho ces Laboratory of Assisted Reproduction, PRANOR Group of Assisted Reproduction, Concebir Clinic, Lima, Peru. *Corresponding Author: jgarciaf@hotmail.com Received 27 April 2011; revised 9 June 2011; accepted 28 June 2011. ABSTRACT background: In order to assess the chromoso- mal status in embryos obtained from vitrified and fresh donated oocytes, preimplantational genetic diagnostic (PGD) was performed after biopsy of one blastomere at day 3. METHODS: A total of 249 oocytes were obtained from 23 oo- cyte donors, 80 oocytes were used in the vitri- fied group and 151 oocytes were used in the fresh group. Nine chromosomes (13, 15, 16, 17, 18, 21, 22, X and Y) were investigated by fluo- rescence in situ hybridization (FISH) analysis in 56 and 121 embryos from vitrified and fresh group respectively. Fertilization, cleavage rate, embryo quality and chromosomal abnormality rate were compared between evaluated groups. Results: Vit rified o ocytes sho wed a su rviv al rate of 97.5%. There was no significant difference in the fertilization rate (82.7% and 91.4%), Day 2 cleavage rate (90.3% and 87.7%) or blastocyst formation ra te ( 31.1% and 44.6% ) for the v i trifie d and fresh groups respectively. Chromosomal abnormality rate (66.1% versus 71.9%), per- centage of abnormal blastocysts (61.1% versus 64.8%) and percen tage o f abnormali ties f or each analyzed chromosome were similar for the vitri- fied group compared with the control group. Conclusions: The rates of chromosomal ab- normalities in embryos from vitrified oocytes are similar to those published previously; and comparable to those observed in embryos from fresh oocytes. These results confirm that the developmental competence and chromosomal status of embryos obtained from vitrified oo- cytes is not affected by the vitrification proce- dure, and they preserve the potential to be fer- tilized and to develop in to blastocyst stage similar to embryos from fresh oocy tes. Keywords: Oocytes; Vitrification; PGD; FISH; ART 1. INTRODUCTION Human oocytes cryopreservation is an attractive choice to the range of fertility treatments presently of- fered. Since the very first frozen oocyte pregnancy was achieved in humans by Chen [1], the slow cooling me- thod has been applied with varying success [2-7]. There are many reports about the cryopreservation of human oocytes with good fertilization and cleavage rates [1,8] but with variable results on pregnancy rates per cycle [9-13]. A recent meta-analysis on slow freezing revealed that the clinical pregnancy rate per transfer with this method was 20.6%, and 2.3% per thawed oocyte [14]. As an alternative to slow freezing, the vitrification procedure has been recently applied for human oocytes and embryos [15,16] allowing to improve the percent- ages of oocyte survival, fertilization, embryo develop- ment rates and clinical outcomes [17-26]. Vitrification is a non-equilibrium method and may be regarded as a radical approach in which ice crystal formation is totally eliminated. Nevertheless, it requires an extremely high cooling rates and high concentrations of cryoprotectants, compared to slow freezing [16], in which a solution/ specimen solidifies to form a glass-like, or vitreous, structure without any ice crystal formation during cool- ing. This state is maintained throughout the whole warming procedure [22]. The difficulties associated with oocyte cryopreserva- tion are mostly related to the special structure and sensi- tivity of this cell, the exposure time to the cryoprotec- tants solutions, the concentration of the cryoprotectants, the equilibrium temperature and the extra and intracellu- lar ice formation factors that affect the viability [10] and physiology of oocytes [27]. Additionally, other biologi- cal characteristics of human oocytes that may be suscep- tible to damage during the cryopreservation procedure are precocious oocyte activation induced by cryoprotec- tants exposures that may disturb future development  J. I. Garc ía et al. / Health 3 (2011) 467-476 Copyright © 2011 SciRes. Openly accessible at http://www.scirp.org/journal/HEALTH/ 468 [27,28]; loss of high mitochondrial polarity associated with a significantly reduced capacity to up-regulate the levels of intracellular free calcium after thawing [29]; microvacuolization in the ooplasm and ultrastructural alterations in specific oocyte microdomains linked to the reduced developmental potential of mature cryopre- served oocytes [30]. Proper organization of the oocyte cytoskeleton, par- ticularly of its microtubular fraction, is essential for normal spindle formation and chromosome segregation [30]. The meiotic spindles are crucial for the events fol- lowing fertilization in the completion of meiosis, second polar body formation, migration of pronuclei, and for- mation of the first mitotic spindle [31]. The meiotic spindle has been shown to be extremely sensitive to temperature variation [32-41], and to depolymerize at low temperatures [42,43]. Subsequent impaired repoly- merization on rewarming may lead to scattering of chromosomes or lesions in the reformed spindle, result- ing in misaggregation of chromatids following resump- tion of meiosis and an increase of aneuploidies incidence in oocytes [44] and later in embryos [45,46]. On the other hand, several studies evaluating the ef- fect of vitrification and slow-freezing on the meiotic spindle integrity and chromosome alignment [47-51], showed less damage in vitrified oocytes (as observed in fresh oocytes without cryopreservation) compared with cryopreserved oocytes by slow-freezing. However, stud- ies of Coticchio et al. [52]; Martinez-Burgos et al. [53] showed that the vitrified-warmed oocytes maintain a metaphase II (MII) spindle with a bipolar organization, but the chromosomal alignment appears to be partly compromised. Additionally, studies of Cobo et al. [19], Chen and Yang, [36] and Ciotti et al. [54] reported that spindle recovery was faster in vitrification than in slow freezing (1-2 hours after thaw procedure). However, most of the available information about of chromosomal status comes from studies performed on cryopreserved oocytes, but not on the embryos derived from those oocytes. The introduction of preimplantation genetic diagnosis (PGD) to the field of reproductive medicine and the analysis of a single blastomere from a day 3 embryo using multicolor fluorescence in-situ hybridization (FISH), permit to detect chromosomal abnormalities and inherited diseases without adversely affecting the de- velopmental [55] or implantation potential of the embryo [56,57]. Routinely, up to 9 to 12 chromosomes can be analyzed on a single fixed nucleus by FISH, in which DNA probes labeled with fluorochromes hybridize to their respective chromosome, allowing for the identifica- tion of ploidy status. The indications for PGD during an IVF cycle are advanced maternal age, repeated implant- tation failure, recurrent pregnancy loss and, previous trisomic conception [58]. The relationship between chromosome abnormalities, embryo morphology and maternal age has been studied extensively [50-62]. Approximately 30% of human em- bryos generated from IVF treatments have an abnormal chromosome constitution [63,64], and this percentage may increase to 60% - 70% in embryos that come from poor prognosis IVF patients such as low responders, older women [65-67], IVF failure [56,68,69], or women with a history of recurrent miscarriage [63,69-73]. In a recent study, involving an examination of nine chromo- somes at the cleavage stage via FISH, 60% of all ana- lyzed embryos derived from women younger than 35 years were found to carry cytogenetic anomalies. The observed abnormality rate increased to 80% for embryos of women 41 years of age and older [74]. On the other hand, young egg donors are traditionally assumed to have low rates chromosome abnormalities, and young donors less than infertile patients, even those with comparable ages. The scanty published PGD data on embryos derived from oocytes donors indicate unex- pectedly high rates of chromosome anomalies (56% - 57%) [50,75]. According to Reis Soares et al. [75] the reason for the observed abnormalities, could be that do- nors are frequently subject to more aggressive stimula- tion, compared with other women of similar age, in order to guarantee the production of a large cohort of oocytes. Nevertheless, the effect of cryopreservation proce- dures on chromosomal status of embryos achieved from cryopreserved oocytes has been little studied. Cobo et al. [76] analyzed the effect the cryopreservation by slow freezing on the chromosomal status of embryos obtained from frozen-thawed oocytes. They showed 28.6% and 26% of aneuploidies in embryos obtained from cryopre- served and fresh oocytes respectively. This study was designed to compare the rates of chro- mosome abnormalities observed in embryos obtained from vitrified and fresh donated oocytes and to evaluate whether the vitrification procedure increase significantly more chromosome abnormalities. 2. MATERIALS AND METHODS 2.1. Patients This study is based on secondary analysis of data ob- tained from procedure of Preimplantational Genetic Di- agnostic (PGD) program in the Laboratory of Assisted Reproduction at the Concebir Clinic (Lima, Peru) carried out over 2009. This study was approved by the Institu- tional Review Board (IRB) and the corresponding Ethics Committee. Written informed consent forms were ob- tained from donors, recipients and their partners in- cluded in this study. The PGD indications were because  J. I. Garc ía et al. / Health 3 (2011) 467-476 Copyright © 2011 SciRes. Openly accessible at http://www.scirp.org/journal/HEALTH/ 469 all patients wish to avoid a pregnancy with trisomic dis- ease. The age of the oocyte donors ranged from 20 - 29-ye- ar-old in both evaluated groups. They were subjected a physical, gynecological and psychological examination and there were no family history of hereditary or chro- mosomal diseases. All participants had a normal karyo- type and tested negative in a screening for sexually transmitted diseases. From the 23 oocyte donors included, 8 were assigned to the vitrified oocytes group and; 15, to the fresh oo- cytes group. A total of 82 and 167 oocytes were obtained from vitrified and fresh oocytes groups respectively. Recruitment of oocyte donors was done based on recommendations given by other donors and the dona- tion of their gametes was merely by altruistic reasons. The donors and their oocytes were random and consecu- tively assigned each evaluated group. They were matched with their recipients according to phenotype and blood groups; and the recipients were not aware not of the ori- gin of oocyte received (vitrified or fresh). 2.2. Controlled Ovarian Stimulation and Oocyte Collection The menstrual cycles of oocyte donors were stimu- lated using recombinant FSH (rFSH) (Puregon®, Or- ganon laboratories, Peru) and GnRH antagonist (Or- galutran® Organon Laboratories, Peru) according to the stimulation protocols previously established and starting on Day 2 of the menstrual cycle until when at least three follicles reached ~18 mm in diameter. The oocyte re- trieval was performed by vaginal ultrasound 36 h after the i.m application of Human Chorionic Gonadotropin, hCG (Ovidrel® 250 µg, Serono Laboratories, Peru). For the procedure, the patient was under general anesthesia with 200 mg of Propofol iv (Diprivan® 1% P/V; Astra- Zeneca Laboratories, UK). During follicular aspiration procedure the oocytes were recovered in Global®-HEPES-buffered medium (IVFonline, Canada) supplemented with 10% vol/vol Serum Substitute Supplement (SSS; Irvine Scientific, USA). After retrieval, cumulus-oocyte complexes were trimmed of excess cumulus cells and maintained in ~200 µL drops of Global®-Fertilization medium (IVFonline, Canada) plus 10% SSS under oil at 37˚C and an atmos- phere containing 5.6% CO2, 5% O2 and 89.4% N2, for 2 hours until when the oocytes recovered were cryopre- served (vitrified group) or 5 hours until when the oo- cytes recovered were inseminated (fresh group). All collected oocytes were denuded enzymatically of cumulus cells with hyaluronidase (80 IU/mL; IVFonline, Canada) to assess nuclear maturity. Only metaphase II (MII) oocytes were vitrified with Cryotop minimum volume vitrification methods [21,48,77] using comer- cial cryoprotectant solutions (Cecolfes, Colombia) and the Cryolock device (Biodiseño-Colombia), for a maxi- mum period of 3 hours after of retrieval. 2.3. Oocyte Vitrification A total of 80 MII oocytes were vitrified which corre- sponding to the vitrified group by minimum volume methods, which minimize the volume of vitrification solution containing oocytes increasing the cooling and warming rates and decreasing the chance of ice crystal nucleation/formation in the small sample [16,78]. The vitrification procedure was performed at room tempera- ture (24˚C). The oocytes were equilibrated in 7.5% vol/vol ethylene glycol (EG) plus 7.5% dimethylsulfox- ide (DMSO) in TCM199 medium for 15 minutes (equi- librium solution, ES) and then placed in 15% EG plus 15% DMSO plus 0.5 mmol/L sucrose (vitrification solu- tion, VS) for a maximum 1 minute. The oocytes were loaded quickly onto the Cryolock in a minimum drop size of <0.1 µL of VS and immediately immersed di- rectly in liquid nitrogen, at a cooling rate of approxi- mately –23,000˚C /min [21]. A maximum three oocytes were placed by Cryolock. All cryoprotectant solutions were supplemented with 20% vol/vol SSS. 2.4. Oocyte Warming Oocytes were warmed at fast warming rates of –12,000˚C/min [21]. The Cryolock was taken out of liquid nitrogen and quickly placed in 1.0 mol/L sucrose in TCM199 medium (thawing solution-TS) for 1 minute at 37˚C. The oocytes were then placed in 0.5 mol/l su- crose in TCM199 medium (diluent solution-DS) for 3 minutes and at room temperature (24˚C), followed by two consecutive 5-min flushes in TCM199 medium (wa- shing solution-WS). Oocytes were then immediately pla- ced in Global®-Fertilization medium plus 10% SSS un- der oil at 37˚C and an atmosphere containing 5.6% CO2, 5% O2 and 89.4% N2 for 2 hours before ICSI. All warm solutions were supplemented with 20% vol/vol SSS. 2.5. Insemination, Fertilization and Embryo Culture In the vitrified group, 2 h after warming the viability of oocytes was evaluated microscopically based on the morphology of the oocyte membrane integrity. All viable oocytes were inseminated by intracytoplasmic sperm injection (ICSI) with spermatozoa from recipient’s hus- band. After ICSI procedure (Day 0), all injected oocytes were cultures at 37˚C in an atmosphere of 5.6% CO2, 5% O2 and 89.4% N2. In the fresh group, ~5 h after of oocyte retrieval, all  J. I. Garc ía et al. / Health 3 (2011) 467-476 Copyright © 2011 SciRes. Openly accessible at http://www.scirp.org/journal/HEALTH/ 470 MII oocytes were inseminated or injected, depending about seminal characteristics, with spermatozoa from recipient’s husband. In both groups, the fertilization was evaluated 16 - 18 hours after insemination by presence of two pronuclei (Day 1). The zygotes were individually cultured under mineral oil, in 10 µL droplets of Global® medium (IV- Fonline, Canada) supplemented with 10% vol/vol SSS from Day 1 to Day 3. On Day 3, the embryos were biop- sied when they had seven-eight blastomeres. After em- bryo biopsy, the embryos were moved to fresh 10 µl droplets of Global® medium +10% SSS. On Day 2 and 3 the embryos were evaluated for cell number and fragmentation; and on Day 5 for develop- ment to blastocyst and expansion. 2.6. Embryo Biopsy, Fixation, and FISH Analysis Embryo biopsies were performed on the third day af- ter insemination, at the 7 - 8 blastomeres stage following a protocol described elsewhere [57]. Individual embryos were placed into calcium/magnesium-free media (PGD Biopsy Medium; IVFonline, Canada). The hole of the zone pellucida was opened with Tyrode's acid solution and one nucleated blastomere was removed mechanic- cally. Blastomeres were fixed individually following a protocol to minimize signal overlap and loss of micro- nuclei [79]. After biopsy all biopsied embryos were rinsed thoroughly and individually cultured under oil in 10-µl droplets of Global® medium +10% SSS at 37˚C and an atmosphere containing 5.6% CO2, 5% O2 and 89.4% N2. PGD analysis was performed by FISH using probes specific for nine chromosome types X, Y, 13, 15, 16, 17, 18, 21 and 22. These probes were used because in the past their use has shown improvements in implantation rates after PGD (56, 57). The FISH analysis consisted of two consecutive hybridizations following previously published protocols [80]. The first hybridization was performed with probes for chromosomes 13, 16, 18, 21 and 22 (Multivysion PB; Vysis, Downer’Grove, IL, USA). The second hybridization consisted of a home- made combination of probes for chromosomes X, Y, 15 and 17 [80]. Scoring was performed by eye without the need of any software. If the specific signals for a chro- mosome were not clearly diagnosable, a third hybridiza- tion using a probe binding to a different locus for that chromosome was used [81]. 2.7. Embryo Quality On Day 2 and 3 the embryos were evaluated for cell number, fragmentation, and multinucleation. Good qual- ity Day 2 embryos were defined as those with 2 - 4 cells and ≤10% of fragmentation and absence of multinuclea- tion. Good-quality Day 3 embryos were defined as those with 6 - 8 cells and ≤10% of fragmentation. Good-quality blastocysts were defined as having an inner cell mass (ICM) and trophoectoderm type A or B [82]. The ICM score was evaluated as follow: type A = compact area, many cells present; type B = cells are loosely grouped. The trophoectoderm was scored as follows: type A = many cells forming a tight epithelial network of cells; type B = few cells forming a loose network of cells. 2.8. Sperm Collection The semen samples were collected by masturbation from the recipients’ partners. Motile spermatozoa were separated from the seminal plasma by centrifugation through 1.0 mL 95% and 45% Isolate gradients (Irvine Scientific, USA). For oligospermic samples the sperm were washed and resuspended in varying amounts of sperm washing medium depending on initial concentra- tion and motility and then placed into 10 µL drops of HEPES-buffered Global medium + 10% SSS for ICSI. 2.9. Statistical Analysis Data were statistically analyzed using the χ2 test and Student’s t-test as appropriate and differences were con- sidered to be significant at P < 0.05. All statistical analy- sis was carried out using the statistic package Stata 10 (StataCorp, College Station, TX, USA). 3. RESULTS The ages of oocyte donors were similar in both evalu- ated groups (24.6 ± 3.5 vs. 24.9 ± 2.7 years; P:NS). The mean days of stimulation (9.4 ± 0.9 vs. 9.1 ± 0.8), mean days of antag-GnRH (1.6 ± 0.7 vs. 1.5 ± 0.7) and rFSH treatment (1825 ± 291.6 vs. 1801.7 ± 261.1 IU/L) were similar between vitrified and fresh groups (data no shown). Results obtained from vitrified and fresh group are shown in Table 1. A total of 82 and 167 oocytes were collected from donors of vitrified and fresh groups, re- spectively. In the vitrified group, there were 80 MII oo- cytes vitrified, resulting in the survival of 78 oocytes (97.5%). Seventy five and 151 oocytes from vitrified and fresh groups, respectively, were inseminated. The normal fertilization (2PN) was similar in both evaluated groups (Vitrified group: 82.7% vs. Fresh group: 91.4%). In the vitrified group, 90.3% of zygotes underwent cleavage on Day 2, whereas for zygotes from fresh group, the cleav- age rate was 87.7%. Mean cell numbers at Days 2 and 3 were similar in both groups. Embryo quality from vitri- fied oocytes was similar to those derived from fresh oo-  J. I. Garc ía et al. / Health 3 (2011) 467-476 Copyright © 2011 SciRes. Openly accessible at http://www.scirp.org/journal/HEALTH/ 471 Table 1. Laboratory results in the vitrified and the fresh group. Vitrified group Fresh group No. total oocytes No. total MII oocytes No. total vitrified oocytes No. total oocytes survival (%) No. total injected oocytes No. total fertilized oocytes (2PN) (%) Cleavage rate by embryo at Day 2 (%) No. cell/embryo at Day 2 (Mean ± SD) Good quality embryos at Day 2 (%) No. cell/embryo at Day 3 (Mean ± SD) Good quality embryos at Day 3 (%) No. total blastocyst (%) Good quality blastocyst (%) Early blastocyst (%) Full blastocyst (%) Expanded blastocyst (%) Hatching blastocyst (%) 82 80 80 78 (97.5) 75 62 (82.7) 90.3 3.63 ± 0.40 91.1 7.11 ± 1.01 80.4 18 (32.1) 66.7 33.3 44.4 16.7 5.6 167 151 - - 151 138 (91.4) 87.7 3.89 ± 0.46 92.6 7.43 ± 0.97 86.8 54 (44.6) 75.9 24.1 59.3 14.8 1.8 P:NS cytes on Day 2 (91.1% vs. 92.6%) and Day 3 (80.4% vs. 86.8%). Blastocyst development rates were similar (32.1% and 44.6%, respectively) for the vitrified and the fresh groups. In addition, embryos reaching the blasto- cyst stage were morphologically similar in both groups. Table 2 shows the results obtained after FISH analysis. A total of 61 (98.4%) and 129 (93.5%) embryos were biopsied from vitrified and fresh groups respectively. A hundred percent of blastomeres biopsied were fixed in both evaluated groups. 91.8% and 93.8% of fixed blas- tomeres were analyzed for both the vitrified and the fresh groups. The proportion of abnormal embryos ob- tained from vitrified oocytes was similar to those ob- served embryos obtained from fresh oocytes (66.1% vs. 71.9%; respectively). Additionally, from those embryos that reached the blastocyst stage, 61.1% and 64.8% in the vitrified and fresh groups respectively, showed chromosomal abnormalities to nine analyzed chromo- somes. The percentage of abnormalities for each chromosome analyzed in both analyzed groups is shown in Table 3. The proportion of abnormalities according to the differ- ent chromosomes analyzed was similar between em- bryos obtained from vitrified and fresh oocytes. 4. DISCUSSION Since the first pregnancy achieved with a vitri- fied/warmed human oocyte [83] and the first birth of a healthy baby [84], vitrification results have improved Table 2. Results of fluorescence in situ hybridization analy- sis in embryos obtained from vitrified and fresh oocytes. Vitrified group Fresh group No. total zygotes (2PN) No. total biopsied embryos (%) No. total fixed embryos (%) No. total analyzed embryos (%) No. total abnormal embryos (%) No. total blastocyst No. total abnormal blastocysts (%) 62 61 (98.4) 61 (100) 56 (91.8) 37 (66.1) 18 11 (61.1) 138 129 (93.5) 129 (100) 121 (93.8) 87 (71.9) 54 35 (64.8) P:NS. Table 3. Percentage of abnormalities for each chromosome analyzed in the vitrified and the fresh group. Chromosome analyzed Vitrified Group Fresh Group 13 15 16 17 18 21 22 XY 34.8% 28.3% 21.7% 19.6% 28.3% 45.7% 19.6% 26.1% 36.2% 40.8% 27.7% 21.5% 29.2% 33.1% 31.5% 23.1% P:NS. significantly during the last decade [17-26,85-88]. Vitrification is the glass-like solidification of a solu- tion at low temperature, without ice crystal formation. This is possible through the extreme elevation in viscos- ity during freezing. This can be achieved by increasing the freezing and warming rates and/or increasing the concentration of the cryoprotectants [89]. Unlike slow freezing, vitrification results in the total elimination of ice crystal formation, within the cells being vitrified and outside the cells in the surrounding solution [78]. Oocyte vitrification avoids meiotic spindle damage and has re- sulted in survival rates of over 80% [19-21,23,48,90]. Additionally, pronuclear zygotes [91], cleavage-stage embryos [82], and blastocysts [92-94] have been suc- cessfully vitrified. During the present study has shown the feasibility and efficiency of oocyte vitrification. We have showed high recovery and post warm survival in vitrified oocytes, and similar fertilization rates and preimplantational devel- opment embryo with vitrified and fresh oocytes, results that confirm data showed previously by others investi- gators [19,20,23]. In the present study, the vitrification procedures were all carried out using the Cryolock de- vice, which has a similar design and handle to those of Cryotop. The Cryolock has been designed and developed specifically for use in vitrification procedures with slots  J. I. Garc ía et al. / Health 3 (2011) 467-476 Copyright © 2011 SciRes. Openly accessible at http://www.scirp.org/journal/HEALTH/ 472 in the ends and top for better manipulation, avoiding the risk that these loosen or fall during their use or storage (Biodiseño-Colombia). Moreover, the vitrification pro- cedure, cryoprotectants and warming media (Cecolfes, Colombia) and the Cryolock device (Biodiseño, Colom- bia) used during oocytes vitrification procedure has been showed previously to be efficient, safety and don’t affect the viability and physiology of oocytes [20]. In recent years PGD technology has been increasingly used by infertile patients undergoing IVF treatment, in order to screen their embryos for chromosomal abnor- malities. Aneuploidy is extremely common in human embryos and leads to developmental arrest, implantation failure and spontaneous abortion. The inadvertent trans- fer of chromosomally abnormal embryos is believed to explain a significant proportion of failed IVF cycles. By screening for aneuploidy and ensuring the transfer of chromosomally normal embryos it has been suggested that a variety of IVF outcomes (including implantation and pregnancy rates) can be improved. Advances in vitrification methods have led to egg sur- vival rate over 85% and the pregnancy rates comparable to those achieved with autogenous and donated fresh oocytes [17,19-21,23,25,26,48,89,95,96]. Additionally, has been demonstrated that vitrification of in-vitro ma- turated oocytes results in high survival rates, normal meiotic spindle and chromosome alignment and no in- creased incidence of aneuploidy compared to those cryopreserved by slow freezing [97]. However, no infor- mation is available about the chromosomal status of hu- man embryos resulting from vitrification and warming procedure, fertilization and preimplantational develop- ment embryo. In the present study, hasn’t been observed deleterious effect of vitrification procedure on the oocyte viability from fertilization to blastocyst stage and principally the morphological characteristics of blastocyst at day 5, similar results to observed by García et al. [20]. On the other hand, has been showed similar aneup- loidy rates in embryos at day 3 (66.1% vs. 71.9%) and in those embryos that achieved the blastocyst stages (66.1% vs. 64.8%) from vitrified and fresh oocytes re- spectively. Similar results were obtained by Baart et al. [98] and Munné et al. [50] when analyzed 196 and 1800 embryos from oocyte donation cycles respectively. They observed that 66% and 57% of embryos were abnormal for 10 and 8 chromosomes analyzed including X, Y, 1, 7, 13, 15, 16, 18, 21 and 22. These results are direct evi- dence that oocytes conserve intact their capability of fertilization and potential the reach the blastocyst stage after being vitrified similar to that observed with fresh oocytes. This study shown that a correct repolymeriza- tion of the spindle may occur during the restoration of the physiological conditions after warming, leading to the right sequence of events involved in the completion of meiosis and fertilization., Finally, our results suggest that vitrification procedure has a lower impact on oocyte physiology, does not affect the normal preimplantational embryo development or increase the aneuploidies inci- dences compared to those observed in embryos from fresh oocytes. Additionally, Chian et al. [18] analyzed the obstetric and perinatal outcomes in 165 pregnancies and 200 infants conceived following oocytes vitrification cycles in three reproductive centers. The results indicate that the mean birth weight and incidence of congenital anomalies are comparable to that of spontaneous con- ceptions in fertile women or infertile women undergoing in-vitro fertilization treatment. These results confirm that oocytes conserve their capability of fertilization and po- tential to reach the blastocyst stage after being vitrified, similar to the data obtained with fresh oocytes. On the other hand, the vitrification of human oocytes solves the legal restrictions and ethical problems [99] associated with the cryopreservation of embryos in pa- tients undergoing in vitro fertilization procedures. Also, it may offer the possibility of extending the reproductive capability of young women with malignant diseases in cases where the treatment by surgery, chemotherapy or radiotherapy may compromise the ovarian reserve [100-103]. Moreover, it also provides alternatives for infertile patients who are subject to ovarian hyperstimu- lation syndrome, poor responder to ovarian stimulation, premature ovarian failure or who require oocyte dona- tion [100]. In conclusion, our observations demonstrate that vitri- fication is an efficient procedure for oocyte cryopreser- vation, the developmental competence of vitrified MII oocytes to rich the blastocyst stage and the chromosomal status are similar to those observed with fresh oocytes. In conclusion, the vitrification procedure represents the best current choice for creation of reliable egg banks. REFERENCES [1] Chen, C. (1986) Pregnancy after human oocytes cryopre- servation. Lancet, 1, 884-886. doi:10.1016/S0140-6736(86)90989-X [2] Allan J. (2004) Pregnancy from intracytoplasmic injec- tion of a frozen-thawed oocyte. The Australian and New Zealand Journal of Obstetrics and Gynaecology, 44, 588. doi:10.1111/j.1479-828X.2004.00317.x [3] Levi Setti, P.E., Albani, E., Novara, P.V., Cesana, A. and Morreale, G. (2006) Cryopreservation of supernumerary oocytes in IVF/ ICSI cycles. Human Reproduction, 21, 370-375. doi:10.1093/humrep/dei347 [4] Nawroth, F. and Kissing, K. (1998) Pregnancy after in- tracytoplasmic sperm injection (ICSI) of cryopreserved human oocytes. Acta Obstet Gynecol Scand, 77, 462-463. 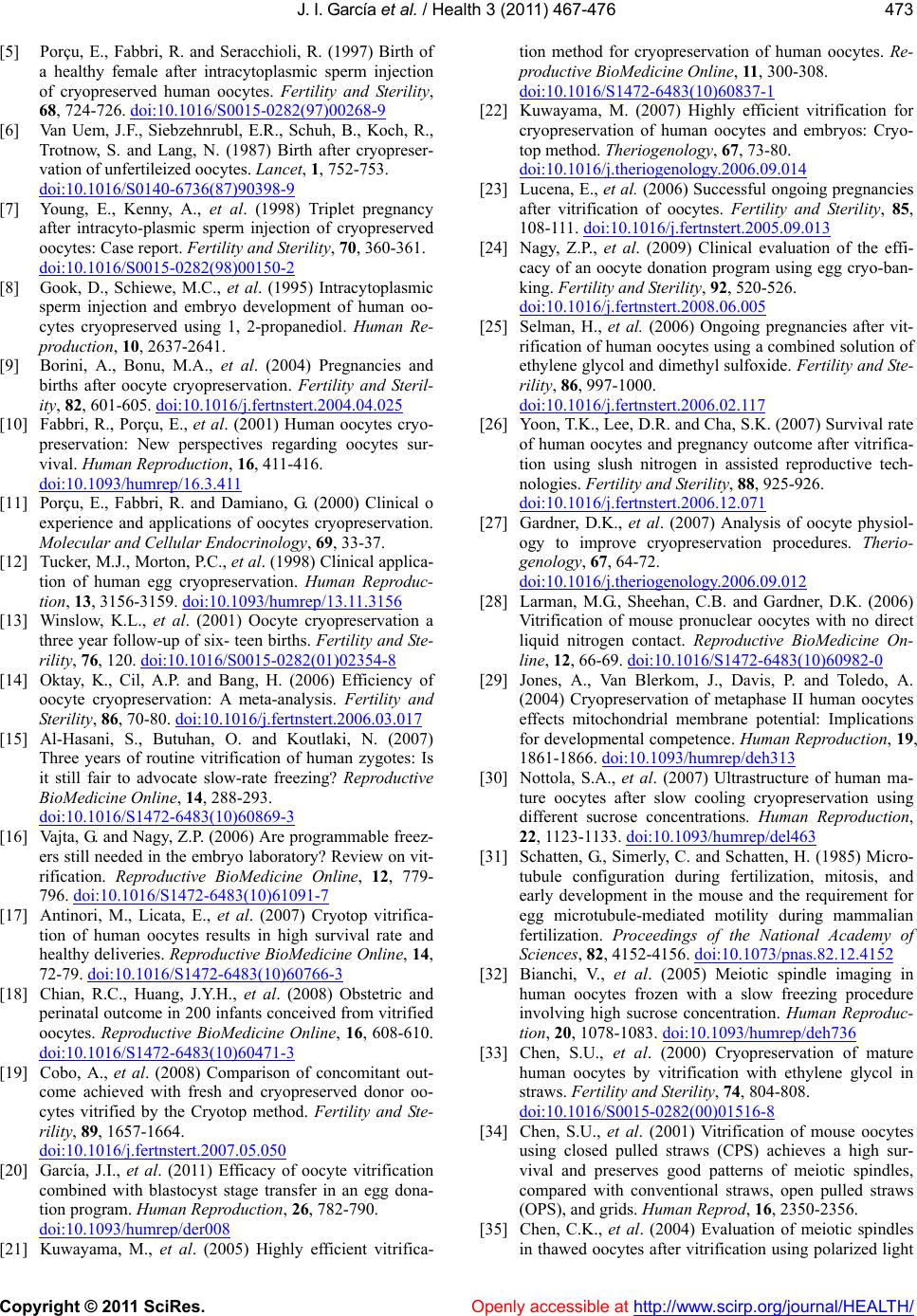 J. I. Garc ía et al. / Health 3 (2011) 467-476 Copyright © 2011 SciRes. Openly accessible at http://www.scirp.org/journal/HEALTH/ 473 [5] Porçu, E., Fabbri, R. and Seracchioli, R. (1997) Birth of a healthy female after intracytoplasmic sperm injection of cryopreserved human oocytes. Fertility and Sterility, 68, 724-726. doi:10.1016/S0015-0282(97)00268-9 [6] Van Uem, J.F., Siebzehnrubl, E.R., Schuh, B., Koch, R., Trotnow, S. and Lang, N. (1987) Birth after cryopreser- vation of unfertileized oocytes. Lancet, 1, 752-753. doi:10.1016/S0140-6736(87)90398-9 [7] Young, E., Kenny, A., et al. (1998) Triplet pregnancy after intracyto-plasmic sperm injection of cryopreserved oocytes: Case report. Fertility and Sterility, 70, 360-361. doi:10.1016/S0015-0282(98)00150-2 [8] Gook, D., Schiewe, M.C., et al. (1995) Intracytoplasmic sperm injection and embryo development of human oo- cytes cryopreserved using 1, 2-propanediol. Human Re- production, 10, 2637-2641. [9] Borini, A., Bonu, M.A., et al. (2004) Pregnancies and births after oocyte cryopreservation. Fertility and Steril- ity, 82, 601-605. doi:10.1016/j.fertnstert.2004.04.025 [10] Fabbri, R., Porçu, E., et al. (2001) Human oocytes cryo- preservation: New perspectives regarding oocytes sur- vival. Human Reproduction, 16, 411-416. doi:10.1093/humrep/16.3.411 [11] Porçu, E., Fabbri, R. and Damiano, G. (2000) Clinical o experience and applications of oocytes cryopreservation. Molecular and Cell u l a r E n d o c ri n o l o g y, 69, 33-37. [12] Tucker, M.J., Morton, P.C., et al. (1998) Clinical applica- tion of human egg cryopreservation. Human Reproduc- tion, 13, 3156-3159. doi:10.1093/humrep/13.11.3156 [13] Winslow, K.L., et al. (2001) Oocyte cryopreservation a three year follow-up of six- teen births. Fertility and Ste- rility, 76, 120. doi:10.1016/S0015-0282(01)02354-8 [14] Oktay, K., Cil, A.P. and Bang, H. (2006) Efficiency of oocyte cryopreservation: A meta-analysis. Fertility and Sterility, 86, 70-80. doi:10.1016/j.fertnstert.2006.03.017 [15] Al-Hasani, S., Butuhan, O. and Koutlaki, N. (2007) Three years of routine vitrification of human zygotes: Is it still fair to advocate slow-rate freezing? Reproductive BioMedicine Online, 14, 288-293. doi:10.1016/S1472-6483(10)60869-3 [16] Vajta, G. and Nagy, Z.P. (2006) Are programmable freez- ers still needed in the embryo laboratory? Review on vit- rification. Reproductive BioMedicine Online, 12, 779- 796. doi:10.1016/S1472-6483(10)61091-7 [17] Antinori, M., Licata, E., et al. (2007) Cryotop vitrifica- tion of human oocytes results in high survival rate and healthy deliveries. Reproductive BioMedicine Online, 14, 72-79. doi:10.1016/S1472-6483(10)60766-3 [18] Chian, R.C., Huang, J.Y.H., et al. (2008) Obstetric and perinatal outcome in 200 infants conceived from vitrified oocytes. Reproductive BioMedicine Online, 16, 608-610. doi:10.1016/S1472-6483(10)60471-3 [19] Cobo, A., et al. (2008) Comparison of concomitant out- come achieved with fresh and cryopreserved donor oo- cytes vitrified by the Cryotop method. Fertility and Ste- rility, 89, 1657-1664. doi:10.1016/j.fertnstert.2007.05.050 [20] García, J.I., et al. (2011) Efficacy of oocyte vitrification combined with blastocyst stage transfer in an egg dona- tion program. Human Reproduction, 26, 782-790. doi:10.1093/humrep/der008 [21] Kuwayama, M., et al. (2005) Highly efficient vitrifica- tion method for cryopreservation of human oocytes. Re- productive BioMedicine Online, 11, 300-308. doi:10.1016/S1472-6483(10)60837-1 [22] Kuwayama, M. (2007) Highly efficient vitrification for cryopreservation of human oocytes and embryos: Cryo- top method. Theriogenology, 67, 73-80. doi:10.1016/j.theriogenology.2006.09.014 [23] Lucena, E., et al. (2006) Successful ongoing pregnancies after vitrification of oocytes. Fertility and Sterility, 85, 108-111. doi:10.1016/j.fertnstert.2005.09.013 [24] Nagy, Z.P., et al. (2009) Clinical evaluation of the effi- cacy of an oocyte donation program using egg cryo-ban- king. Fertility and Sterility, 92, 520-526. doi:10.1016/j.fertnstert.2008.06.005 [25] Selman, H., et al. (2006) Ongoing pregnancies after vit- rification of human oocytes using a combined solution of ethylene glycol and dimethyl sulfoxide. Fertility and Ste- rility, 86, 997-1000. doi:10.1016/j.fertnstert.2006.02.117 [26] Yoon, T.K., Lee, D.R. and Cha, S.K. (2007) Survival rate of human oocytes and pregnancy outcome after vitrifica- tion using slush nitrogen in assisted reproductive tech- nologies. Fertility and Sterility, 88 , 925-926. doi:10.1016/j.fertnstert.2006.12.071 [27] Gardner, D.K., et al. (2007) Analysis of oocyte physiol- ogy to improve cryopreservation procedures. Therio- genology, 67, 64-72. doi:10.1016/j.theriogenology.2006.09.012 [28] Larman, M.G., Sheehan, C.B. and Gardner, D.K. (2006) Vitrification of mouse pronuclear oocytes with no direct liquid nitrogen contact. Reproductive BioMedicine On- line, 12, 66-69. doi:10.1016/S1472-6483(10)60982-0 [29] Jones, A., Van Blerkom, J., Davis, P. and Toledo, A. (2004) Cryopreservation of metaphase II human oocytes effects mitochondrial membrane potential: Implications for developmental competence. Human Reproduction, 19, 1861-1866. doi:10.1093/humrep/deh313 [30] Nottola, S.A., et al. (2007) Ultrastructure of human ma- ture oocytes after slow cooling cryopreservation using different sucrose concentrations. Human Reproduction, 22, 1123-1133. doi:10.1093/humrep/del463 [31] Schatten, G., Simerly, C. and Schatten, H. (1985) Micro- tubule configuration during fertilization, mitosis, and early development in the mouse and the requirement for egg microtubule-mediated motility during mammalian fertilization. Proceedings of the National Academy of Sciences, 82, 4152-4156. doi:10.1073/pnas.82.12.4152 [32] Bianchi, V., et al. (2005) Meiotic spindle imaging in human oocytes frozen with a slow freezing procedure involving high sucrose concentration. Human Reproduc- tion, 20, 1078-1083. doi:10.1093/humrep/deh736 [33] Chen, S.U., et al. (2000) Cryopreservation of mature human oocytes by vitrification with ethylene glycol in straws. Fertility and Sterility, 74, 804-808. doi:10.1016/S0015-0282(00)01516-8 [34] Chen, S.U., et al. (2001) Vitrification of mouse oocytes using closed pulled straws (CPS) achieves a high sur- vival and preserves good patterns of meiotic spindles, compared with conventional straws, open pulled straws (OPS), and grids. Human Reprod, 16, 2350-2356. [35] Chen, C.K., et al. (2004) Evaluation of meiotic spindles in thawed oocytes after vitrification using polarized light  J. I. Garc ía et al. / Health 3 (2011) 467-476 Copyright © 2011 SciRes. Openly accessible at http://www.scirp.org/journal/HEALTH/ 474 microscopy. Fertility and Sterility, 82, 666-672. doi:10.1016/j.fertnstert.2003.12.053 [36] Chen, S.U. and Yang, Y.S. (2009) Slow freezing or vitri- fication of oocytes: Their effects on survival and meiotic spindles, and the time schedule for clinical practice. Taiwanese Journal of Obstetrics and Gynecology, 48, 15- 22. doi:10.1016/S1028-4559(09)60030-9 [37] Coticchio, G., et al. (2005) Criteria to assess human oo- cyte quality after cryopreservation. Reproductive Bio- Medicine Online, 11, 421-427. doi:10.1016/S1472-6483(10)61133-9 [38] De Santis, L., et al. (2007) Objective evaluation of the viability of cryopreserved oocytes. Reprod Biomed Online, 15, 338-345. doi:10.1016/S1472-6483(10)60348-3 [39] Eroglu, A., et al. (1998) Alterations of the cytoskeleton and polyploidy induced by cryopreservation of meta- phase II mouse oocytes. Fertility and Sterility, 69, 944- ocytes. 00. 957. [40] Larman, M.G., et al. (2007) Maintenance of the meiotic spindle during vitrification in human and mouse o Reproductive BioMedicine Online, 15, 692-7 doi:10.1016/S1472-6483(10)60537-8 [41] Rienzi, L., et al. (2004) Polscope analysis of meiotic spindle changes in living metaphase II oocytes during the freezing and thawing procedures. Human Reproduction, 19, 655-659. doi:10.1093/humrep/deh101 [42] Magistrini, M. and Szollosi, D. (1980) Effects of cold and of isopropyl-N-phenylcarbamate on the second mei- otic spindle of mouse oocytes. European Journal of Cell ion and Biology, 22, 699-707. [43] Sathananthan, A.H., et al. (1992) The effects of cooling mouse oocytes. Journal of Assisted Reproduct Genetics, 9, 139-148. doi:10.1007/BF01203754 [44] Wang, W.H., et al. (2001) Limited recovery of meiotic spindle in living human oocytes after cooling-rewarming observed using polarized light microscopy. Human Re- oling of the ility, 92, production, 16, 2374-2378. [45] Sathananthan, A.H., et al. (1988) The effects of co human oocytes. Human Reproduction, 3, 968-977. [46] Van der Elst, J., et al. (1988) Effect of 1,2-propanediol and di- methylsulphoxide on the meiotic spindle mouse oocyte. Human Reproduction, 3, 960-967. [47] Cao, Y.X., et al. (2009) Comparison of survival and em- bryonic development in human oocytes cryopreserved by slowfreezing and vitrification. Fertility and Ster 1306-1311. doi:10.1016/j.fertnstert.2008.08.069 [48] Katayama, P., et al. (2003) High survival rate of vitrified human oocytes results in Sterility, 80, 223-224. clinical pregnancy. Fertility and doi:10.1016/S0015-0282(03)00551-X [49] Kuwayama, M. (2001) Vitrification of human oocytes and embryos. In: Suzuki, S. Ed., IVF Update, Medical ng egg donors. Re- View Co., Tokyo, 230-234. [50] Munné, S., et al. (2006) Wide range of chromosome abnormalities in the embryos of you prod Biomed Online, 12, 340-346. doi:10.1016/S1472-6483(10)61007-3 [51] Silber, S., et al. (2003) Chromosomal abnormalities in embryos derived from TESE. Fertility and Sterility, 79, 30-38. doi:10.1016/S0015-0282(02)04407-2 [52] Coticchio, G., et al. (2009) Vitrification may increase the rate chromosome misalignment in the metaphase II spin- dle of human mature oocytes. Reproductive BioMedicine Online, 19, 29-34. doi:10.1016/S1472-6483(10)60281-7 [53] Martínez-Burgos, M., et al. (2011) Vitrification versus slow freezing of oocytes: effects on morphologic ap- pearance, meiotic spindle configuration, a age. Fertility and Sterility, 95, 374-377 nd DNA dam- . doi:10.1016/j.fertnstert.2010.07.1089 [54] Ciotti, P.M., et al. (2009) Meiotic spindle recovery is faster in vitrification of human oocytes compared to slow freezing. Fertility and St erility, 91, 23 99-2407. doi:10.1016/j.fertnstert.2008.03.013 [55] Hardy, K., et al. (1990) Human preimplantation devel- opment in vitro is not adversely affected by biopsy at the rility, 72, 8-cell stage. Human Reproduction, 5,708-714. [56] Gianaroli, L., et al. (1999) Preimplantation diagnosis for aneuploidies in patients undergoing in vitro fertilization with poor prognosis: Identification of the categories for which it should be proposed. Fertility and Ste 837-844. doi:10.1016/S0015-0282(99)00377-5 [57] Munné, S., et al. (2003) Improved implantation after Preimplantation genetic of an BioMedicine Online, 7, 91-97. euploidy. Reproductive doi:10.1016/S1472-6483(10)61735-X [58] Munné, S., et al. (2004b) Increased rate of aneuploid embryos in young women with previous ane ceptions. Prenatal Duploid con- iagnosis, 24, 638-647. doi:10.1002/pd.957 [59] Gianaroli, L., et al. (2007) Oocyte aneuploidy, pronu- clear zygote morphology and embryo chr complement. Human Reproduomosomal ction, 22, 241-249. doi:10.1093/humrep/del334 [60] Magli, M.C., et al. (2001) Double locus analysis of chromosome 21 for Preimplantation genetic diag aneuploidy. Prenatal nosis of Diagnosis, 21, 1080-1085. doi:10.1002/pd.248 [61] Márquez, C., et al. (2000) Chromosome abnormalities in 1255 cleavage-stage human e Medicine Online, 1, 17-27. mbryos. Reproductive Bio- doi:10.1016/S1472-6483(10)61988-8 [62] Munné, S., et al. (2004a) Differences in chromosome susceptibility to aneuploidy and survival to fir Reproductive BioMedicine Online, 8, 8 st trimester. 1-90. doi:10.1016/S1472-6483(10)60501-9 [63] Rubio, C., et al. (2003) Chromosomal abnormalities and embryo development in recurrent m Human Reproduction, 18, 182 iscarriage couples. -188. doi:10.1093/humrep/deg015 [64] Rubio, C., et al. (2005) FISH screening of aneuploidies in preimplantation embryos to improve IVF ou Reproductive BioMedicine Online, 11, 497-506. tcome. doi:10.1016/S1472-6483(10)61146-7 [65] Kahraman, S., et al. (2000) Healthy births and ongoing pregnancies by preimplantation genetic diagnosis in pa- tients with advanced maternal age and recurrent impl tation failure. Human Reproductan- ion, 15, 2003-2007. doi:10.1093/humrep/15.9.2003 [66] Munné, S., et al. (1995) Embryo morphology, develop- mental rates, and maternal age are correlated with chro- mosomal abnormalities. Fertility and Sterility, 64, 382- 391. [67] Munné, S., et al. (2002) Preimplantation genetic diagno-  J. I. Garc ía et al. / Health 3 (2011) 467-476 Copyright © 2011 SciRes. Openly accessible at http://www.scirp.org/journal/HEALTH/ 475 er indications. Fer-sis for advanced maternal age and oth tility and Sterility, 78, 234-236. doi:10.1016/S0015-0282(02)03239-9 [68] Pehlivan, T., et al. (2003) Impact of preimplantation genetic diagnosis on IVF outcome in implanttation fail- ure patients. Reproductive BioMedicine Online, 6, 232- 237. doi:10.1016/S1472-6483(10)61715-4 [69] Wilding, M., et al. (2004) Preimplantation genetic diag- nosis for treatment of failed in vitro fertilization embryo transfer and habitual abortion. Fertility and Sterility, 81, 1302-1307. doi:10.1016/j.fertnstert.2003.10.028 [70] Pellicer, A., et al. (1999) In vitro fertilization plus preim- plantation genetic diagnosis in patients with recurrent miscarriage: an analysis of chromosome abnormalities in human preimplantation embryos. Fertility and Sterility, 71, 1033-1039. doi:10.1016/S0015-0282(99)00143-0 [71] Simón, C., et al. (1998) Increased chromosome abnor- malities in human Preimplantation embryo after in vitro fertilization in patients with recurrent miscarriage production, Fertility a. Re- nd Development, 10, 87-92. doi:10.1071/R98030 [72] Vidal, F., et al. (1998) FISH preimplantation diagnosis of chromosome aneuploidy in recurrent pregnancy wastage. Journal of Assisted Reproduction and Genetics, 15, 309- 312. doi:10.1023/A:1022552713015 [73] Werlin, L., et al. (2003) Preimplantation genetic diagno- sis as both a therapeutic and diagnosis tool in assisted re- productive technology. Fertility and Sterility, 80, 467- 468. doi:10.1016/S0015-0282(03)00605-8 [74] Munné, S., et al. (2007) Maternal age, morphology, de- velopment and chromosome abnormalities in over 6000 cleavage-stage embryo. Reproductive BioMedicine Online, 14, 628-634. doi:10.1016/S1472-6483(10)61057-7 [75] Reis Soares, S., et al. (2003) High frequency of chro somal abnormalities in embryo obta mo- ined from oocyte donation cycle. Fertility and Sterility, 80, 656-657. doi:10.1016/S0015-0282(03)00787-8 [76] Cobo, A., et al. (2001) Use of fluorescence in situ hy- bridization to assess the chromosomal status of embryos obtained from cryopreserved oocytes. Fertility and Ste- rility, 75, 354-360. doi:10.1016/S0015-0282(00)01725-8 [77] Kuleshova LL, Lopata A. (2002) Vitrification can be more fa- vorable than slow cooling. Fertility and Steril- ity,; 78, 449-454. doi:10.1016/S0015-0282(02)03305-8 [78] Rall, W.F. (1987) Factors affecting the survival of mouse em- bryos cryopreserved by vitrification. Cryobiology, 24, 387-402. doi:10.1016/0011-2240(87)90042-3 [79] Velilla, E., Escudero, T. and Munné, S. (2002) Blas- tomere fixation technique and risk of misdiagnosis for PGD of aneuploidy. Reproductive BioMedicine Online, 4, 210- 217. doi:10.1016/S1472-6483(10)61808-1 [80] Munné, S., et al. (1998) Preimplantation diagnosis of the aneuploidies most commonly found tions and live births: X, 13, 14, 15, 16, 18, 21, 22. Preg- nancy Diagnosis, 18, 1 in spontaneous abor- 459-1466. doi:10.1002/(SICI)1097-0223(199812)18:13<1459::AID -PD514>3.0.CO;2-V [81] Colls, P., et al. (2004) PGD analysis for aneup patient heterozygous loidy in a for a polymorphism of chromosome 16 (16qh-). Prenatal Diagnosis, 24, 741-744. doi:10.1002/pd.887 [82] El-Danasouri, I. and Selman, H. (2001) Successful preg- nancies and deliveries after a simple vitrification protocol for day 3 human embryos. Fertility and Sterility, 76, 400- 402. doi:10.1016/S0015-0282(01)01907-0 [83] Hong, S.W., et al. (1999) Improved human o velopment after vitrification: A comp ocytes de- arison of thawing methods. Fertility and Sterility, 72, 142-146. doi:10.1016/S0015-0282(99)00199-5 [84] Yoon, T.K., et al. (2000) Pregnancy and delivery of healthy infants developed from vitr stimulated in vitro fertilization-embryo ified oocytes in a transfer program. Fertility and Sterility, 74, 180-181. doi:10.1016/S0015-0282(00)00572-0 [85] Kim, T.J., et al. (2010) Vitrification of oocy dures high pregnancy rates when c tes proce- arried out in fertile women. Fertility and Sterility, 93, 467-474. doi:10.1016/j.fertnstert.2008.12.094 [86] Rienzi, L., et al. (2010) Embryo development of fresh “versus” vitrified metaphase II oocytes after ICSI: A s survival, fertilization and oductive BioMedi- prospective randomized sibling-oocyte study. Reproduc- tive BioMedicine Online, 25, 66-73. [87] Sher, G., et al. (2008) Selective vitrification of euploid oocytes markedly improve pregnancy-generating potential. Repr cine Online, 17, 524-529. doi:10.1016/S1472-6483(10)60240-4 [88] Ubaldi, F., et al. (2010) Cumulative ongoing pregnancy rate achieved with oocyte vitrification and cleavag transfer without embryo selec e stage tion in a standard infertility program. Human Reproduction, 25, 1199-1205. doi:10.1093/humrep/deq046 [89] Fahy, G.M., et al. (1984) Vitrification as an approach to cryopreservation. Cryobiology, 21, 407-426. doi:10.1016/0011-2240(84)90079-8 [90] Chian, R.C., et al. (2005) High survival rates a nancies of human oocytes followin nd preg- g vitrification: Pre- liminary report. Fertility and Sterility, 80, 36. doi:10.1016/j.fertnstert.2005.07.086 [91] Isachenko, V., et al. (2005) Aseptic technolog cation of human pronuclear y of vitrifi- oocytes using open-pulled straws. Human Reproduction, 20, 492-496. doi:10.1093/humrep/deh605 [92] Lane, M., et al. (1999) Containerless vitrification of mammalian oocytes and embryos. Nat Biotechnol, 17, 1232-1236. doi:10.1038/70795 [93] Lieberman, J., et al. (2002) Blastocyst development after vitrification of multipronuclear zygotes using the flexipet denuding pipette. Reproductive BioMedicine Online, 4, 146-150. doi:10.1016/S1472-6483(10)61932-3 [94] Mukaida, T., et al. (2003) Vitrificatio cysts using cryoloops: Clinic n of human blasto- al outcome of 223 cycles. Human Reproduction, 18, 384-391. doi:10.1093/humrep/deg047 [95] Cobo, A., et al. (2010) Use of cryo-banked oocytes in an ovum donation programme: A prospective, randomized, controlled, clinical trial. Human Reproduction, 25, 2239- 2246. doi:10.1093/humrep/deq146 [96] Yoon, T.K., et al. (2003) Live births after vitrification oocytes in a stimulated in vitro fertiliz of ation-embryo tran- sfer program. Fertility and Sterility, 79, 1323-1326. doi:10.1016/S0015-0282(03)00258-9 [97] Huang, J.Y., et al. (2007) Comparison of spindle and  J. I. Garc ía et al. / Health 3 (2011) 467-476 Copyright © 2011 SciRes. http://www.scirp.org/journal/HEALTH/Openly accessible at 476 red chromosome configuration in vitro and in vivo matu mouse oocytes after vitrification. Fertility and Sterility, 90, 1424-1432. doi:10.1016/j.fertnstert.2007.07.1335 [98] Baart, E.B., et al. (2006) Preimplantation genetic screening reveals a high incidence of a mosaicism in embryos from neuploidy and young women undergoing IVF. Human Reproduction, 21, 223-233. doi:10.1093/humrep/dei291 [99] Parmegiani, L., et al. (2008) Freezing within 2 h from oocyte retrieval increases the efficiency of human oocyte cryopreservation when using slow freezing/rapid thawing protocol with high sucrose concentration. Human Re- production, 23, 1771-1777. doi:10.1093/humrep/den119 [100] Gidoni, Y., et al. (2008) Fert cine Online, 16, 792-800. ility presservation in patients with non-oncological conditions. Reproductive BioMedi- doi:10.1016/S1472-6483(10)60144-7 [101] Li, X.H., et al. (2005) Cryopreserved oocytes of infertile couples undergoing assisted reproductive technology could be an important source of oocyte donation: A clini- cal report of successful pregnancies. Human Reproduc- tion, 20, 3390-3394. doi:10.1093/humrep/dei262 [102] Porçu, E., et al. (2008) Healthy twins delivered after oocyte cryopreservation and bilateral ovariectomy for ovarian cancer. Reproductive BioMedicine Online, 17, ed before cancer treatment. Fertility and Sterility, 87, 4. 265-267. [103] Yang, D., et al. (2007) Live birth after the transfer of human embryos developed from cryopreserved oocytes harvest
|