Health
Vol.5 No.8B(2013), Article ID:35760,10 pages DOI:10.4236/health.2013.58A2005
Sleep quality, sleep patterns and consumption of energy drinks and other caffeinated beverages among Peruvian college students*
![]()
1Universidad de San Martin de Porres, Lima, Peru
2Asociacion Civil Proyectos en Salud (PROESA), Peru
3Department of Epidemiology, Harvard School of Public Health, Multidisciplinary International Research Training Program, Boston, USA; †Corresponding Author: bgelaye@hsph.harvard.edu
4Department of Biostatistics, University of Washington, Seattle, USA
Copyright © 2013 Sixto E. Sanchez et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received 6 May 2013; revised 6 June 2013; accepted 17 July 2013
Keywords: Sleep; Energy Drinks; College Students; Peru
ABSTRACT
Objectives: To evaluate sleep quality in relation to lifestyle characteristics including consumption of energy drinks and other caffeinated beverages among Peruvian college students. Methods: A total of 2458 college students were invited to complete a self-administered questionnaire that collected information about a variety of behaviors including consumption of energy drinks, caffeinated and alcoholic beverages. The Pittsburgh Sleep Quality Index (PSQI) was used to assess sleep quality. Logistic regression procedures were used to estimate odds ratios (OR) and 95% confidence intervals (95% CI) for poor sleep quality in relation to lifestyle characteristics. Results: A total of 965 males and 1493 female students were enrolled in the study. 52.0% of males and 58.4% of females experienced poor sleep quality (p = 0.002). Females (OR = 1.28; 95% CI 1.08 - 1.51) and those who reported consuming ≥3 stimulant beverages per week (OR = 1.88; 95% CI 1.42 - 2.50) had higher odds of poor sleep quality. Students who consumed 1 - 19 alcoholic beverages monthly (OR = 1.90; 95% CI 1.46 - 2.49) had a higher odds of long sleep latency. Consumption of ≥3 stimulant beverages per week was associated with daytime dysfunction due to sleep loss (OR = 1.45; 95% CI 1.10 - 1.90), short sleep duration (OR = 1.49; 95% CI 1.14 - 1.94), and use of sleep medication (OR = 2.10; 95% CI 1.35 - 3.28). Conclusions: Consumption of energy drinks, other caffeinated beverages and alcoholic beverages are risk factors of poor sleep quality. Increased awareness of these associations should promote interventions to improve students’ lifestyle habits, including consumption of alcoholic and caffeinated beverages, and overall health.
1. INTRODUCTION
As a pivotal modulator of hormone release, cardiovascular activity and glucose regulation, sleep has been observed to have significant effects on a person’s daily life [1]. Insufficient sleep and irregular sleep-wake patterns have been observed at high rates on college campuses, and sleep problems have been associated with lower academic performance, impaired social relationships, more risk-taking behavior and poorer overall health [2,3]. College students tend to keep shorter sleep schedules and have irregular sleep patterns as they attempt to compensate for extended periods of sleep deprivation or sleep debt which are associated with poorer academic achievement and increased symptoms of depression [2-4]. Sleep loss and sleep debt are known to lead to irregular sleep patterns, daytime sleepiness, exhaustion, inattentiveness and increased risks for obesity, diabetes, cardiovascular disease, hypertension, mood disorders, substance abuse and other health issues [5]. Sleep loss (≤7 hours per night) can have lasting negative effects on the cardiovascular, endocrine, immune and nervous systems [5].
To compensate for a lack of sleep, college students today appear to be developing a higher level of dependence on energy drinks and other caffeinated beverages that continue into adulthood [6,7]. Energy drinks contain caffeine as a primary ingredient and other substances such as guarana (containing Guaranine, similar to caffeine), taurine (an amino acid) and sugar derivatives [8]. Caffeine has been shown to have both positive and negative behavioral, cognitive and health effects depending on the amount consumed. When consumed in excess, caffeine can disrupt sleep [9]. Caffeine consumption significantly reduces sleep time, lengthens the perceived onset of sleep, and disturbs sleep quality [10]. Excessive caffeine ingestion has been associated with increases in nocturnal body movements, impairments in the development of deeper stages of non-rapid eye movement (NREM) sleep and changes in the temporal organization of slow wave and rapid eye movement during sleep [6,10]. Disturbed NREM sleep coupled with the accumulation of adenosine and its sleep-inducing effect causes the phenomenon of sleep inertia [11]. Furthermore, investigators have noted that caffeine dependence may develop among individuals who consume caffeine because of a subliminal need to counteract sleep inertia [6].
The amount of caffeine students consume is increasingly considered to be excessive compared with amounts once thought to be compatible with improving cognitive performance and alertness [12]. In light of the increasing prevalence of sleep disorders among college students and the deleterious effects of excessive consumption of caffeinated beverages, we seek to estimate the prevalence of poor sleep quality among Peruvian college students and to examine the extent to which poor sleep quality and altered sleep patterns are associated with consumption of caffeinated beverages including energy drinks and other caffeinated beverages.
2. MATERIALS AND METHODS
2.1. Study Setting and Sample This cross-sectional study was conducted in the Universidad Nacional Mayor de San Marcos and Universidad San Martin de Porres in Lima, Peru from November 2010 through May, 2011. The Universidad Nacional Mayor de San Marcos is one of the oldest universities in the country founded in 1551. It is a university with national leadership and recognized by the Latin American community and world for its academic excellence and scientific research. The Universidad San Martin de Porres is one Peru’s largest universities and ranks among the top three private universities in the country. The university has more than 30,000 students and 2500 faculty and administrative staff. The two universities were selected based on their large number of students and their willingness to participate in the study.
Flyers were posted in each department to invite participants. Students who expressed an interest in participating in the study were invited to meet in a large classroom or an auditorium where they were informed about the purpose of the study and asked to participate in the survey. Students consenting to participate were asked to complete a self-administered individual surveys. There was no set time limit for completing the survey. A total of 2634 undergraduate students participated in the study. For the study described here, we excluded subjects with incomplete questionnaires and missing sleep quality scores (n = 176). The final analyzed sample included 2458 students (965 males and 1493 females).
2.2. Ethics Statement
All completed questionnaires were anonymous, and no personal identifiers were used. Given the minimum risk of the study and use of anonymous questionnaire, waiver of documentation of written consent form was approved by the ethics committees. The procedures used in this study were approved by the institutional review boards of Dos de Mayo Hospital and Universidad Nacional Mayor de San Marcos in Lima, Peru and the University of Washington, USA. The Harvard School of Public Health Office of Human Research Administration, USA granted approval to use the de-identified data set for analysis.
2.3. Data Collection and Variables
A self-administered questionnaire was used to collect information for this study. The questionnaire ascertained demographic information including age, sex, and education level. Questions were also included regarding behavioral risk factors such as cigarette smoking, energy drinks, caffeinated beverages, and alcohol consumption. Measurements of the students’ height, weight, waist, and hip circumference were also collected by trained research staff after each questionnaire was completed.
2.4. Use of Energy Drinks and Other Caffeinated Beverages
Participants were first asked if they consumed more than one energy drinks or caffeinated beverages per week each month during the current academic semester/quarter. Participants answering “yes” were further asked to identify the specific type of energy or caffeinated drinks. Energy drinks included international and local brands such as: Red Bull, Evolution Drink, Turbo, Maretazo, Shark, Burn, Liftoff and Vortes. For the purpose of this analysis we grouped Liftoff and Vortes, the two least frequent and similar beverages, (no vs. yes). Other caffeinated beverages included coffee (no vs. yes) and colas such as Coke and Pepsi (no vs. yes). We use the term stimulant drinks to describe both energy drinks as well as other caffeinated beverages consumed per week.
2.5. Pittsburgh Sleep Quality Index (PSQI)
Sleep quality was assessed using the previously validated Pittsburgh Sleep Quality Index (PSQI) [13]. The PSQI is a 19-item self-reported questionnaire that evaluates sleep quality over the past month. The PSQI yields seven sleep components related to sleep habits including duration of sleep, sleep disturbance, sleep latency, habitual sleep efficiency, use of sleeping medicine, daytime dysfunction, and overall sleep quality. The sleep components yield a score ranging from 0 to 3, with three indicating the greatest dysfunction [13]. The sleep component scores were summed to yield a total score ranging from 0 to 21 with higher total scores (referred to as global scores) indicating poor sleep quality. Based on prior literature, participants with a global score of >5 were classified as poor sleepers; while those with a score ≤5 were classified as good sleepers [13].
For sleep quality subscales, subjective sleep efficiency, sleep latency, sleep medication use, and daytime dysfunction due to sleepiness, we computed a dichotomous variable of optimal and suboptimal sleep quality. Specific categories were long sleep latency (≥30 minutes vs. <30 minutes); poor sleep efficiency (<85% vs. ≥85%); days of daytime dysfunction due to sleep loss (< once a week vs. ≥ once per week); and sleep medication use during the past month (< once a week vs. ≥ once per week). Sleep duration was assessed using the PSQI questionnaire that queried how many hours of actual sleep the participants got on average at night during the previous month. Given the lack of prior data on cutoffs for defining “short sleep duration” among college students, we used quartiles. The following quartiles were used to define sleep duration: ≤5.0 hours, 5.1 - 6.0 hours, 6.1 - 7.0 hours, and ≥7.1 hours. The group with the lowest quartile of sleep duration (≤5 hours) was defined as short duration sleepers. This classification is consistent with prior studies of college students [14].
2.6. Other Covariates
We defined alcohol consumption as low (<1 alcoholic beverage a month), moderate (1 - 19 alcoholic beverages a month), and high to excessive consumption (>19 alcoholic beverages a month). We used these cut-points based on prior published literature [15,16]. Other variables were categorized as follows: age (years), sex, smoking history (never, former, current), and engaging in moderate or vigorous physical activity (no vs. yes). Body mass index (BMI) was calculated as weight (kg)/height squared (m2). Different thresholds of BMI were set according to the World Health Organization protocol [17] (underweight: <18.5 kg/m2; normal: 18.5 - 24.9 kg/m2; overweight: 25.0 - 29.9 kg/m2; and obese ≥30 kg/m2) [18].
2.7. Statistical Analysis
We first examined frequency distributions of sociodemographic and behavioral characteristics of study participants. Characteristics were summarized using means (±standard deviation) for continuous variables and counts and percentages for categorical variables. Chi-square test and Student’s t-test were used to determine bivariate differences for categorical and continuous variables, respectively. Next, we calculated the distribution of poor sleep quality across socioeconomic and behavioral groups. The distributions of PSQI scores among male and female students, as well as the sex-specific prevalence of poor sleep quality across age groups were also estimated. We used multivariable logistic regression procedures to estimate odds ratios (OR) and 95% confidence intervals (95% CI) for the associations between poor sleep quality and socio-demographic and behavioral factors. Frequency distribution of PSQI subscales were calculated separately for male and female students. Prevalence estimates were also determined for suboptimal dichotomous sleep quality subscales in relation to stimulant drinks and lifestyle characteristics. Confounding variables were considered a priori on the basis of their hypothesized relationship with sleep quality and lifestyle characteristics. Logistic regression procedures with change-in-estimate approach were used to adjust for covariates [19]. Variables of a priori interest (e.g., age) were forced into final models. Linear trends were estimated for smoking status, alcohol consumption and number of stimulant use by modeling each as an ordinal continuous variable. All analyses were performed using IBM’s SPSS Statistical Software for Windows (IBM SPSS Version 19, Chicago, Illinois, USA). All reported p-values are two-sided and deemed statistically signifycant at α = 0.05.
3. RESULTS
The socio-demographic and selected behavioral characteristics of study participants are summarized in Table 1. A total of 2458 students participated in the study. The mean age of study participants was 20.9 years (standard deviation = 2.6); and the majority of participants were females (60.7%). Approximately 17% of the students reported that they were current smokers and 40.1% were
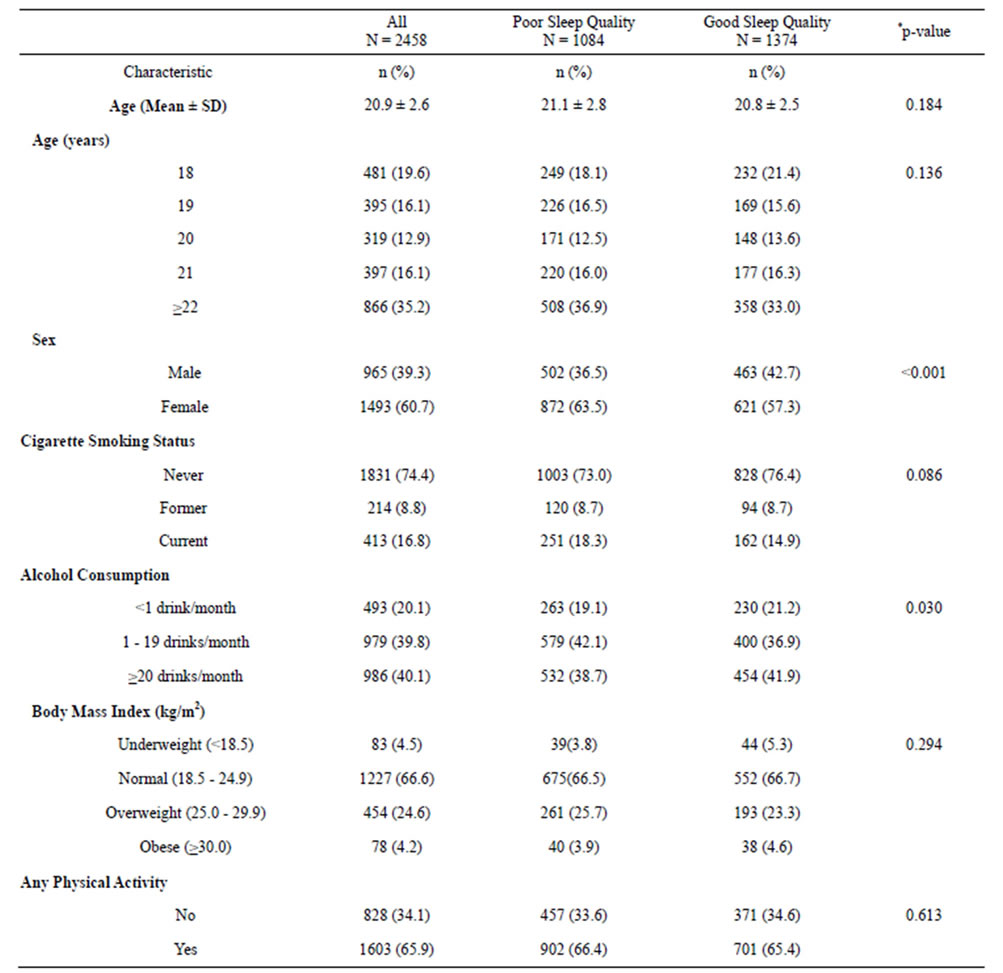
Table 1. Characteristics of the study population.
*p-value from Chi-Square test for categorical variables or from Student’s t-test for continuous variables. **Numbers may not add up due to missing.
classified as heavy consumers of alcoholic beverages (≥20 alcoholic beverages per month). Approximately 28.8% of participants were overweight or obese (BMI > 25 kg/m2) and 34.1% reported to be physically inactive. Overall, 55.9% of study participants were found to have poor sleep quality.
Bivariate associations between sleep quality (poor and good) and students’ demographic and selected lifestyle characteristics are also presented in Table 1. The age distribution was not statistically significantly different across the two sleep quality groups, although poor sleepers tended to be slightly older (p = 0.136) than their counterparts who were classified as good sleepers. A higher proportion of females had poor sleep quality (63.5%) as compared with males (57.3%) (p < 0.001). A higher proportion of current smokers were had poor sleep quality as compared with never smokers, although this difference did not reach statistical significance (p = 0.086). Students who reported consuming 1 - 19 alcoholic beverages per month were more likely to be poor sleepers than those who reported consuming <1 alcoholic beverage per month (p = 0.030). No significant difference was observed between sleep quality and BMI (p = 0.294) or physical activity (p = 0.613).
Table 2 shows the distribution of the six sleep quality subscales by gender. Approximately 39% of students reported short sleep duration (≤5 hours). Long sleep latency (>30 minutes) was reported by 24.4% of participants; and frequent (≥1 per week) complaints of daytime dysfunction due to sleep loss were also common in this cohort (32.1%). Approximately 2% of students reported using sleep medications at ≥1 per week during the month prior to the study, and 19.3% of participants were classified as having poor sleep efficiency. Female students were more likely to have short sleep duration (p ≤ 0.001), long sleep latency (p ≤ 0.001), poor sleep efficiency (p ≤ 0.001), and more day time dysfunction due to sleep loss (p = 0.013) than their male counterparts. Female students were more likely (≥3 per week) to use sleep medications (p = 0.012) as compared with males.
As shown in Table 3, the odds of poor sleep quality was 1.28-fold higher among females as compared with
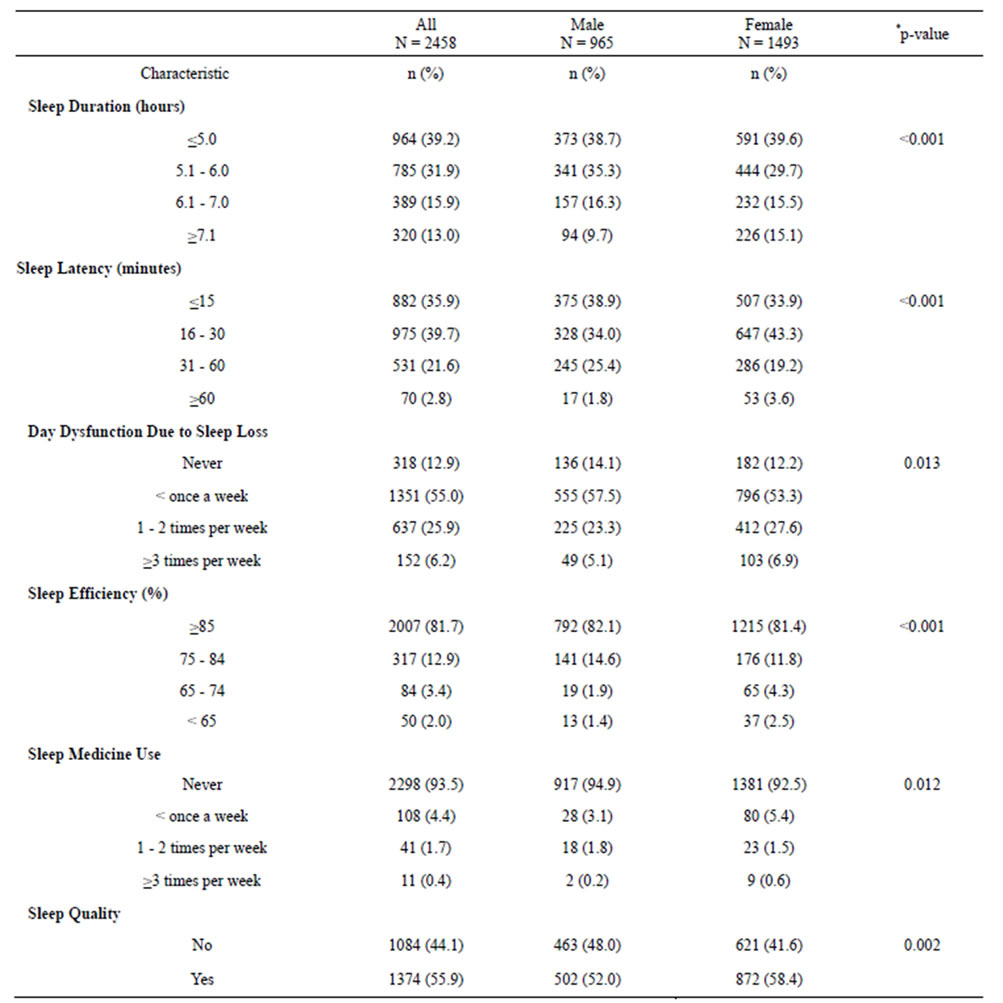
Table 2. PSQI sleep quality subscale by sex.
*p-value from Chi-Square test. **Numbers may not add up due to missing.
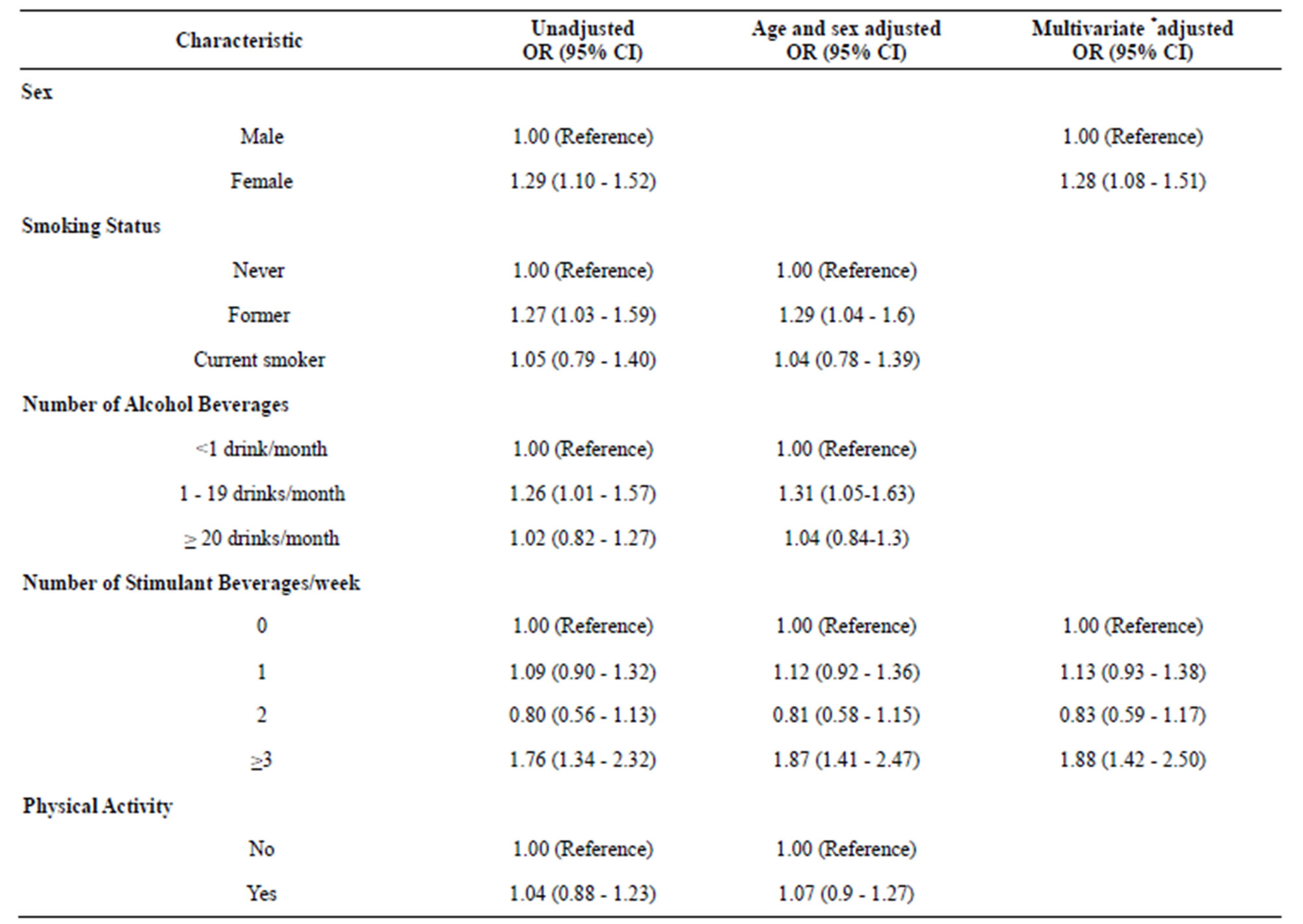
Table 3. Odds ratio (OR) and 95% confidence intervals (CI) for poor sleep quality.
*Each odds ratio is adjusted for all other covariates listed in the table. **Poor sleep quality: PSQI Global score > 5.
males (OR = 1.28, 95% CI 1.08 - 1.51). After adjusting for age and gender, those who reported moderate alcohol consumption (1 - 19 drinks per month) had a 1.31-fold increased odds of poor sleep quality (OR = 1.31; 95% CI 1.05 - 1.63) compared to low alcohol consumers (<1 alcoholic beverage a month). Similar increased odds of poor sleep quality was observed for former smokers (OR = 1.29; 95% CI 1.04 - 1.60) compared to non-smokers. No significant associations were observed for current smokers or heavy drinkers. In multivariate adjusted models, students who reported consumption of ≥3 different types of caffeinated beverages per week had a 1.88-fold increased odds of poor sleep quality (OR = 1.88; 95% CI 1.42 - 2.50) as compared with non-consumers.
Table 4 displays bivariate associations between the different types of stimulant beverages students reported consuming. Red Bull and Burn were consumed by more than one quarter (26.1%) of study participants. Students who consumed Red Bull and Burn were significantly more likely to experience poor sleep quality (p ≤ 0.001). Approximately 27% of students reported consuming caffeinated cola products (Pepsi/Coke). Of the students who regularly consumed cola products, a higher percentage was classified as having poor sleep quality (p ≤ 0.001). However, no significant association was observed between coffee drinking and poor sleep quality (0.193). Table 5 shows the odds ratios for sleep quality parameters in relation to lifestyle characteristics including stimulant beverage consumption. Former (OR = 1.42; 95% CI 1.04 - 1.95) and current smokers (OR = 1.33; 95% CI 1.04 - 1.69) were more likely to have long sleep latency (>30 minutes) compared to never smokers. Current smokers were also more than twice as likely to use sleep medications (OR = 2.11; 95% CI 1.45 - 3.07) as compared with never smokers. Alcohol consumption was significantly associated with short sleep duration and sleep medication use. Students who reported heavy alcohol consumption (≥20 drinks per month), as compared with those who consumed <1 drink per month, had 1.28-fold higher odds (OR = 1.28; 95% CI 1.02 - 1.59) of short sleep duration and a 1.26-fold increased odds of long sleep latency (OR = 1.26; 95% CI 0.96 - 1.67), though the latter association did not reach statistical sig-
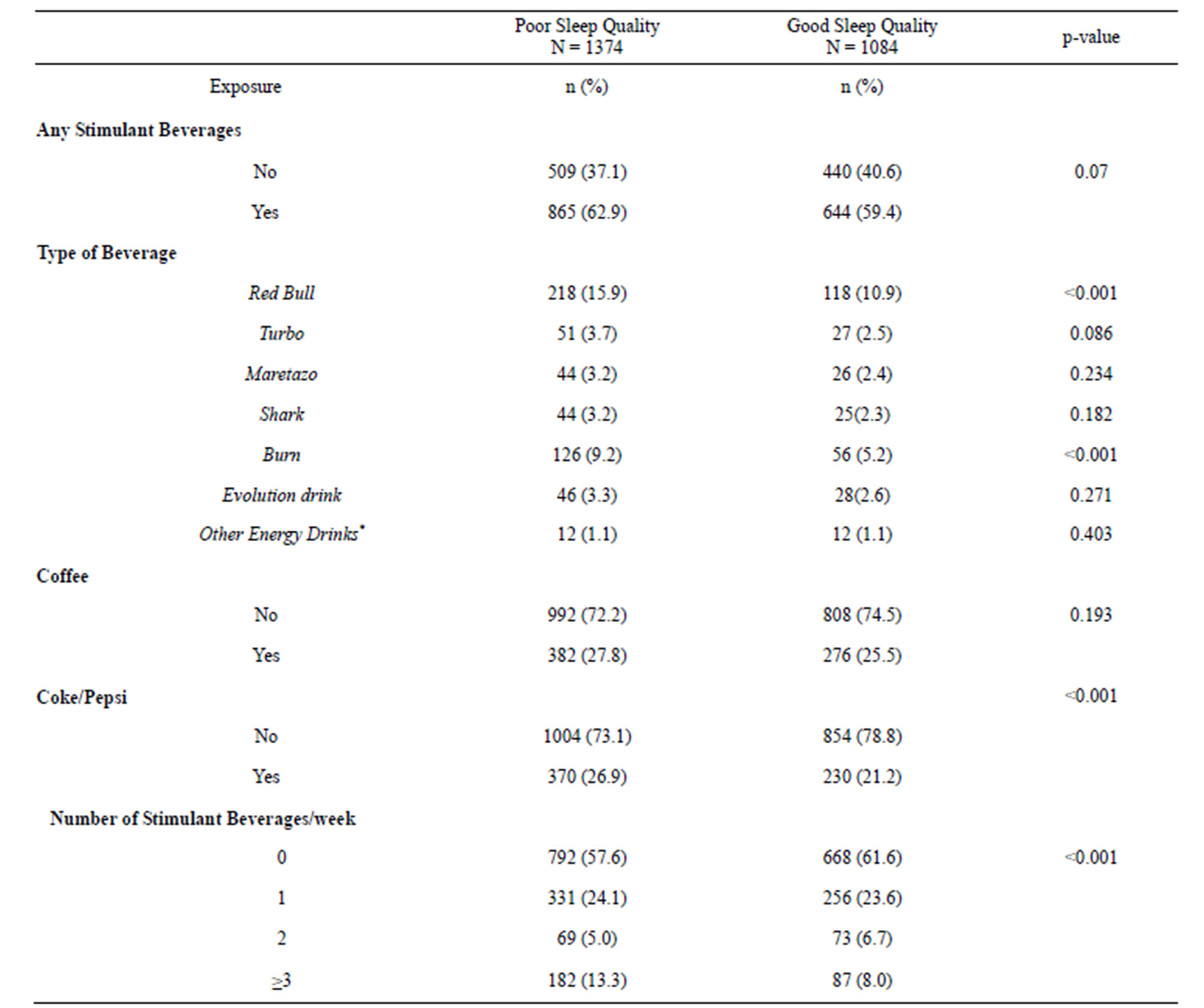
Table 4. Consumption of energy drinks and caffeinated beverages according to sleep quality.
*p-value from Chi-Square test for categorical variables or from Student’s t-test for continuous variables. **Numbers may not add up due to missing. ***Other energy drinks includes the following (Liftoff, Vortes).
nificance. Students who reported moderate alcohol consumption (1 - 19 drinks per month), compared with those who consumed <1 drink per month were more likely to report having long sleep latency (OR = 1.90; 95% CI 1.46 - 2.49) and use sleep medications (OR = 2.08; 95% CI 1.22 - 3.99). Consumption of ≥3 types of stimulant beverages per week, as compared to no consumption, was associated with a: 1.49-fold higher odds of short sleep duration (< 5 hours) (95% CI 1.14 - 1.94), a 1.93-fold higher odds of longer sleep latency (95% CI 1.45-2.57), a 1.45-fold higher odds of report day dysfunction due to sleep loss (95% CI 1.10 - 1.90), and 2.10-fold higher odds of using sleep medications (95% CI 1.35 - 3.28). Physical activity was associated with a modest, though statistically significant increase in odds of long sleep latency (OR = 1.34; 95% CI 1.09 - 1.64).
4. DISCUSSION
We found a high prevalence of poor sleep quality (55.9%) among Peruvian college students with a higher frequency among females (58.4%) than males (52%). Students who consumed different types of caffeinated beverages including popular energy drinks had higher odds of poor sleep quality compared with those who abstained from. Our study extends the existing literature by documenting associations of the consumption of different types of energy drinks with overall sleep quality.
Our findings are largely consistent with other studies that have reported the higher prevalence of poor sleep
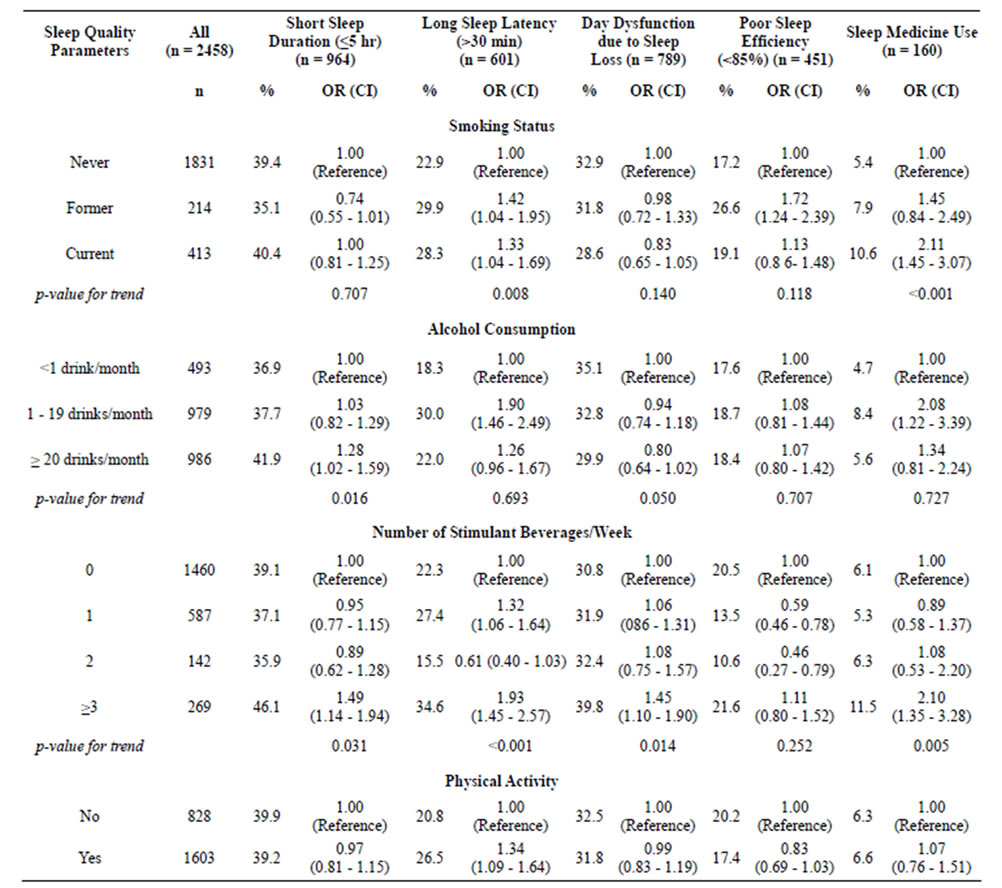
Table 5. Prevalence and odds ratios for sleep quality parameters in relation to lifestyle characteristics.
*Adjusted for age and gender.
quality among college students [7,20] and associations of caffeine intake with sleep disruption [7,10,20]. Additionally, our findings of poorer sleep quality among female versus male participants are similar to reports from Marco et al. 2011 [21]. Some investigators have noted that menstrual cycle may influence sleep-wake activity [22]. The menstrual cycle of young healthy women is characterized by fluctuations of hormone levels and temperature control [23]. Changes in hormonal levels such as gonadal steroids, pituitary hormones, melatonin and cortisol are likely to affect sleep quality. Although there is an emerging literature suggesting the effect of the menstrual cycle phase on sleep quality, results have been inconsistent due to methodological challenges [23].
A 1998 study conducted by Sherrill et al. [24] found that physical activity was associated with improved sleep quality. However, we observed no evidence of an association between overall sleep quality and physical activity in our study cohort. However, we observed a modest increased odds of long sleep latency (≥30 minutes) (OR = 1.34; 95% CI 1.09 - 1.64) among students reporting physical activity as compared with their more sedentary counterparts. Our finding of an increased odds of poor sleep quality among students reporting modest quantities of alcohol on a monthly basis is generally consistent with reports by others [7,25]. In addition, students who reported moderate alcohol consumption were more likely to report having long sleep latency and use sleep medications. However, we noted no clear pattern of a linear trend in the odds of poor sleep quality with heavy alcohol consumption. Our observations are in agreement with the results of most prior studies that showed alcohol drinking as a risk factor to poor sleep quality [2]. It is also important to note that there is a growing body of evidence that shows the popularity of alcohol mixed with energy drinks among college students, especially while partying, that warrants further among our study population [8,12].
Our study had several notable strengths. These include the large sample size of 2458 participants, the fact that anthropometric measures (e.g., weight and height) were directly measured by trained research personnel, and the instruments we used have been widely used in large population based survey settings. However, the results of our study should be interpreted in the context of some limitations. First, we did not use random sampling, but instead considered subjects who were willing to participate in the study, thus our findings may be subject to volunteer bias. Second, there may be substantial heterogeneity among poor sleepers (PSQI total scores among those classified as poor sleepers), which could mask the association between sleep quality and some of the lifestyle characteristics considered. Third, although we adjusted for several potential confounders, we cannot exclude the possibility of residual confounding due to misclassification of adjusted variables or confounding by other unmeasured variables. Fourth, we did not have information concerning the frequency and dose of energy drinks consumption in the present study. As a result, it is possible that the binary grouping of energy drinks consumption attenuated the magnitude of association towards null. Lastly, as this study followed a cross-sectional data collection design, the temporal relationship between poor sleep quality and energy drinks, alcohol consumption, and/or cigarette smoking could not be determined. A longitudinal study design would better allow determination of the prospective relationship between stimulant use and altered sleep quality.
Observed associations of poor sleep quality with consumption of caffeinated beverages are biologically plausible. Briefly, caffeine is a methylxanthine and adenosine receptor antagonist that has potent psychoactive properties [26]. The concentration of adenosine in the brain determines the depth and duration of sleep because it is a physiologic sleep factor [27]. Furthermore, adenosine is an essential component of homeostatic sleep regulation [28]. Adenosine increases drowsiness, decreases electroencephalogram arousal, and enhances slow wave activity during sleep [26]. As a result of sleep, adenosine levels decrease slowly [29]. When caffeine is consumed, it acts as an adenosine receptor antagonist by binding to G protein coupled receptors in the brain that mediate the cellular effects of adenosine [26]. Additionally, investigators have reported that caffeine reduces homeostatic sleep pressure and decreases slow wave power in the frontal, central and parietal regions [30]. Taken together research documenting diverse mechanisms through which caffeine acts on, the central nervous system [26,31] reinforces epidemiological evidence linking sleep disturbances and poor sleep quality with higher frequencies and doses of consumption.
Energy drinks, especially those containing high caffeine concentrations, are targeted to young adult consumers. Moreover, college students are increasingly reporting use energy drinks and other stimulants as a means of avoiding sleep or compensating for insufficient sleep and enhancing academic performance. Given these behavioral patterns, and given known adverse health effects of excessive caffeine use and sleep deprivation, parents, young adults and educators should also be made more aware and perhaps be encouraged to develop and implement wellness programs and policies that promote the avoidance of excessive use of caffeine and other stimulants (e.g., discourage consumption of energy drink by prohibiting sale of energy drinks in campus stores). Research that elucidates independent and joint effects of such wellness programs and policies will give public health professionals and educators the information and impetus needing for investing and promoting campaigns to address poor sleep quality in young adults.
5. ACKNOWLEDGEMENTS
C.M. and R.O. were research training fellows with the Multidisciplinary International Research Training (MIRT) Program of the Harvard University School of Public Health when this research study was completed. The Multidisciplinary International Research Program is supported by an award from the National Institutes of Health, National Institute on Minority Health and Health Disparities (T37-MD000149).
REFERENCES
- Cheng, S.H., Shih, C.C., Lee, I.H., Hou, Y.W., Chen, K.C., et al. (2012) A study on the sleep quality of incoming university students. Psychiatry Research, 197, 270-274. doi:10.1016/j.psychres.2011.08.011
- Lund, H.G., Reider, B.D., Whiting, A.B. and Prichard, J.R. (2010) Sleep patterns and predictors of disturbed sleep in a large population of college students. Journal of Adolescent Health, 46, 124-132. doi:10.1016/j.jadohealth.2009.06.016
- Gaultney, J.F. (2011) The prevalence of sleep disorders in college students: Impact on academic performance. The Journal of American College Health, 59, 91-97. doi:10.1080/07448481.2010.483708
- Thacher, P.V. (2008) University students and “the all nighter”: Correlates and patterns of students’ engagement in a single night of total sleep deprivation. Behavioral Sleep Medicine, 6, 16-31. doi:10.1080/15402000701796114
- IOM (2006) Institute of Medicine, Committee on Sleep Medicine and Research. In: Harvey R.C. and Bruce M.A., Eds., Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem, National Academy of Sciences Press, Washington DC.
- Pollak, C.P. and Bright, D. (2003) Caffeine consumption and weekly sleep patterns in US seventh-, eighth-, and ninth-graders. Pediatrics, 111, 42-46. doi:10.1542/peds.111.1.42
- Lohsoonthorn, V., Khidir, H., Casillas, G., Lertmaharit, S., Tadesse, M.G., Pensuksan, W.C., Rattananupong, T., Gelaye, B. and Williams, M.A. (2012) Sleep quality and sleep patterns in relation to consumption of energy drinks, caffeinated beverages, and other stimulants among Thai college students. Sleep Breath (Epub ahead of print). doi:10.1007/s11325-012-0792-1
- Howland, J. and Rohsenow, D.J. (2013) Risks of energy drinks mixed with alcohol. JAMA, 309, 245-246. doi:10.1001/jama.2012.187978
- Březinová, V. (1974) Effect of caffeine on sleep: EEG study in late middle age people. British Journal of Clinical Pharmacology, 1, 203-208.
- Hindmarch, I., Rigney, U., Stanley, N., Quinlan, P., Rycroft, J., et al. (2000) A naturalistic investigation of the effects of day-long consumption of tea, coffee and water on alertness, sleep onset and sleep quality. Psychopharmacology, 149, 203-216. doi:10.1007/s002130000383
- Van Dongen, H.P., Price, N.J., Mullington, J.M., Szuba, M.P., Kapoor, S.C., et al. (2001) Caffeine eliminates psychomotor vigilance deficits from sleep inertia. Sleep, 24, 813-819.
- Malinauskas, B.M., Aeby, V.G., Overton, R.F., CarpenterAeby, T. and Barber-Heidal, K. (2007) A survey of energy drink consumption patterns among college students. Nutrition Journal, 6, 35. doi:10.1186/1475-2891-6-35
- Buysse, D.J., Reynolds, C.F., Monk, T.H., Berman, S.R. and Kupfer, D.J. (1989) The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Research, 28, 193-213. doi:10.1016/0165-1781(89)90047-4
- Carney, C.E., Edinger, J.D., Meyer, B., Lindman, L. and Istre, T. (2006) Daily activities and sleep quality in college students. Chronobiology International, 23, 623-637. doi:10.1080/07420520600650695
- WHO (2004) Global status report on alcohol. World Health Organization. Department of Mental Health and Substance Abuse, Geneva.
- Freiberg, M.S., Cabral, H.J., Heeren, T.C., Vasan, R.S. and Curtis Ellison, R. (2004) Alcohol consumption and the prevalence of the metabolic syndrome in the US: A cross-sectional analysis of data from the third national health and nutrition examination survey. Diabetes Care, 27, 2954-2959. doi:10.2337/diacare.27.12.2954
- WHO (1995) Physical status: The use and interpretation of anthropometry. Report of a WHO Expert Committee, WHO, Geneva.
- Lowe, B., Spitzer, R.L., Grafe, K., Kroenke, K., Quenter, A., et al. (2004) Comparative validity of three screening questionnaires for DSM-IV depressive disorders and physicians’ diagnoses. Journal of Affective Disorders, 78, 131-140. doi:10.1016/S0165-0327(02)00237-9
- Rothman, K.J. and Greenland, S. (1998) Modern epidemiology. Lippincott-Raven, Philadelphia.
- Lemma, S., Patel, S.V., Tarekegn, Y.A., Tadesse, M.G., Berhane, Y., et al. (2012) The epidemiology of sleep quality, sleep patterns, consumption of caffeinated beverages, and khat use among Ethiopian college students. Sleep Disorders, 2012, 11. doi:10.1155/2012/583510
- Marco, C.A., Wolfson, A.R., Sparling, M. and Azuaje, A. (2011) Family socioeconomic status and sleep patterns of young adolescents. Behavioral Sleep Medicine, 10, 70-80. doi:10.1080/15402002.2012.636298
- Leibenluft, E., Fiero, P.L. and Rubinow, D.R. (1994) Effects of the menstrual cycle on dependent variables in mood disorder research. Archives of General Psychiatry, 51, 761-781. doi:10.1001/archpsyc.1994.03950100009002
- Krishnan, V. and Collop, N.A. (2006) Gender differences in sleep disorders. Current Opinion in Pulmonary Medicine, 12, 383-389. doi:10.1097/01.mcp.0000245705.69440.6a
- Sherrill, D.L., Kotchou, K. and Quan, S.F. (1998) Association of physical activity and human sleep disorders. Archives of Internal Medicine, 158, 1894-1898. doi:10.1001/archinte.158.17.1894
- Roehrs, T. and Roth, T. (2001) Sleep, sleepiness, sleep disorders and alcohol use and abuse. Sleep Medicine Reviews, 5, 287-297. doi:10.1053/smrv.2001.0162
- Nehlig, A. and Boyet, S. (2000) Dose-response study of caffeine effects on cerebral functional activity with a specific focus on dependence. Brain Research, 858, 71-77. doi:10.1016/S0006-8993(99)02480-4
- Calamaro, C.J., Mason, T.B. and Ratcliffe, S.J. (2009) Adolescents living the 24/7 lifestyle: Effects of caffeine and technology on sleep duration and daytime functioning. Pediatrics, 123, e1005-e1010. doi:10.1542/peds.2008-3641
- Benington, J.H. and Heller, H.C. (1995) Restoration of brain energy metabolism as the function of sleep. Progress in Neurobiology, 45, 347-360. doi:10.1016/0301-0082(94)00057-O
- Porkka-Heiskanen, T., Alanko, L., Kalinchuk, A. and Stenberg, D. (2002) Adenosine and sleep. Sleep Medicine Reviews, 6, 321-332. doi:10.1053/smrv.2001.0201
- Drapeau, C., Hamel-Hebert, I., Robillard, R., Selmaoui, B., Filipini, D., et al. (2006) Challenging sleep in aging: The effects of 200 mg of caffeine during the evening in young and middle-aged moderate caffeine consumers. Sleep Medicine Reviews, 15, 133-141. doi:10.1111/j.1365-2869.2006.00518.x
- Landolt, H.P., Retey, J.V., Tonz, K., Gottselig, J.M., Khatami, R., et al. (2004) Caffeine attenuates waking and sleep electroencephalographic markers of sleep homeostasis in humans. Neuropsychopharmacology, 29, 1933- 1939. doi:10.1038/sj.npp.1300526
NOTES
*Conflict of Interest: The authors have no competing interests to declare.
#These authors contributed equally to this work.

