Open Journal of Modern Neurosurgery
Vol.4 No.3(2014), Article ID:48330,6 pages
DOI:10.4236/ojmn.2014.43023
Obstructive Hydrocephalus Caused by Pituitary Adenoma: A Case Report
O. Rezaee1, R. Salar1*, R. Jabari1, A. Shams Akhtari2
1Neurosugery Department, Shahid Beheshti University of Medical Sciences, Tehran, Iran
2Emergency Department, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Email: *amin.may1981@gmail.com
Copyright © 2014 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/
![]()
![]()

Received 9 May 2014; revised 9 June 2014; accepted 9 July 2014
ABSTRACT
Among pituitary tumors, prolactin (PRL)-secreting pituitary adenomas are by far the most frequent ones. The development of symptomatic hydrocephalus due to a pituitary adenoma is an exceptional event. The authors describe a 37-year-old man who had a pituitary adenoma associated with obstructive hydrocephalus that was managed by endoscopic transnasal transsphenoidal surgery. Postoperative CT and MRI scans showed resolution of the obstructive hydrocephalus and the foramen of Monro was open. Postoperatively, the patient had visual and headache improvement. Subsequently, the patient is a candidate for cranial surgery or medical therapy to complete the treatment. The present case highlights the fact that pituitary adenomas with obstructive hydrocephalus should be distinguished from other tumors especially colloid cysts.
Keywords: PRL-Secreting Pituitary Adenomas, Transnasal Transsphenoidal Surgery, Obstructive Hydrocephalus, Cranial Surgery

1. Introduction
Sellar tumours have a large histological variability and represent approximately 10% - 15% of all intracranial neoplasms; from them pituitary adenomas represent 95% of lesions [1] . Depending on the population surveyed, their reported annual incidence varies from 1.0 to 7.6 per 100,000 populations [2] [3] . Among pituitary tumors, prolactin (PRL)-secreting pituitary adenomas are by far the most frequent ones. Patients with prolactinoma usually present with endocrinological symptoms and, less commonly, with visual defects due to compression of the optic chiasm [4] . The development of symptomatic hydrocephalus due to a pituitary adenoma is an exceptional event. Transnasal surgery for transsphenoidal access to the pituitary and adjacent skull base has undergone rapid evolution in recent years. Surgical approaches through the nose without sublabial incisions have become the norm in many centers throughout the world [5] -[7] . However, the transsphenoidal approach for pituitary adenomas may be complicated by incomplete resection because of limited visualization and inability to maintain free circulation of cerebrospinal fluid [8] . In this report, we describe a patient who had a pituitary adenoma associated with obstructive hydrocephalus treated by endoscopic transnasal transsphenoidal surgery.
2. Case Report
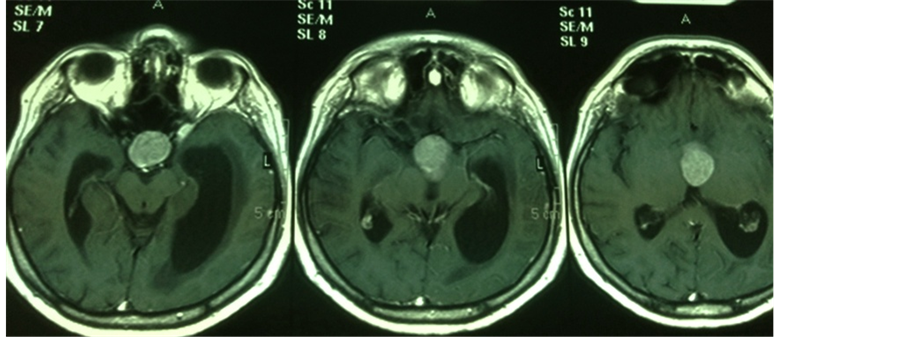
A 37-year-old man presented to us with hairless, headache and visual disturbance in both eyes for three months. Physical examination showed bitemporal hemianopsia. Computerized tomography (CT) scan showed a tumor situated in third ventricle near to the foramen of Monro (Figure 1, Figure 2). A colloid cyst of the third ventricle was initially diagnosed in the patient. Subsequent magnetic resonance imaging (MRI) demonstrated a pituitary macroadenoma (38 × 23 × 21 mm) located mainly outside the sella turcica with suprasellar extension and there was hydrocephalus on the left side of the third ventricle (Figure 3).
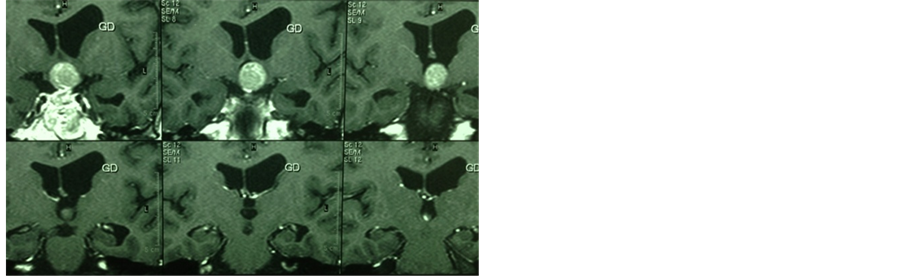
We received the laboratory report that showed a clearly elevated PRL level of 1600 IU/mL (normal level 86 - 324), thus establishing the diagnosis of macroprolactinoma. Low level of testosterone 0.2 ng/mL (normal level 2.49 - 8.36) and high levels of LH 13.9 mU/mL (normal level 1.7 - 8.6) and FSH30.7 mU/mL (normal level 1.5 - 12.4) were observed. Pathological levels of other hormones were: T4: 9.8 mcg/mL (normal level 5.1 - 14), TSH: 1.12 IU/mL (normal level 0.27 - 4.2), Cortisol: 190 ng/mL (normal level 54.9 - 287.5), GH: 0.03 ng/mL (normal level 0 - 4), ACTH: 35.85 pg/mL (normal level 3.6 - 60.5), IGS1: 132.3 pg/mL (normal level 88.3 - 209.9). In a first stage the acutely symptomatic obstructive hydrocephalus was treated with endoscopic transnasal transsphenoidal approach. But there was still a residual tumor mass, which could not be removed by this treatment. Postoperative CT and MRI scans showed resolution of the obstructive hydrocephalus and the foramen of Monro was open (Figures 4-6). Postoperatively, the patient had visual and headache improvement. Subsequently, the patient is a candidate for cranial surgery or medical therapy to complete the treatment.
3. Discussion
The present case was unusual because the patient had a pituitary macroadenoma secreting prolactin with ob-

Figure 1. CT image showing a mass in the foramina of Monro regionthat based on a colloid cyst of the third ventricle is initially diagnosed.

Figure 2. CT image clearly shows hydrocephalus toward the left.
 (a)
(a)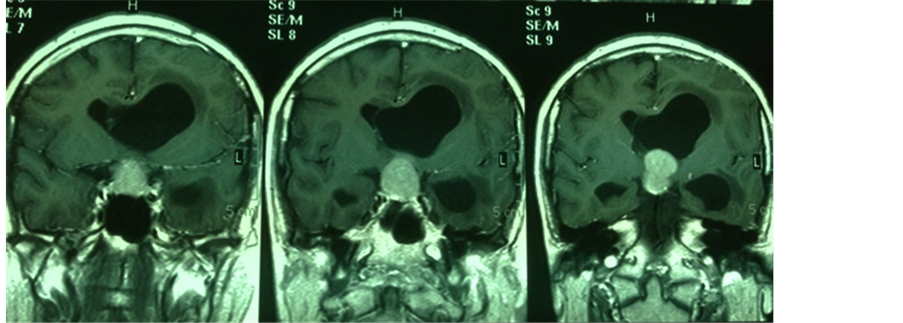 (b)
(b)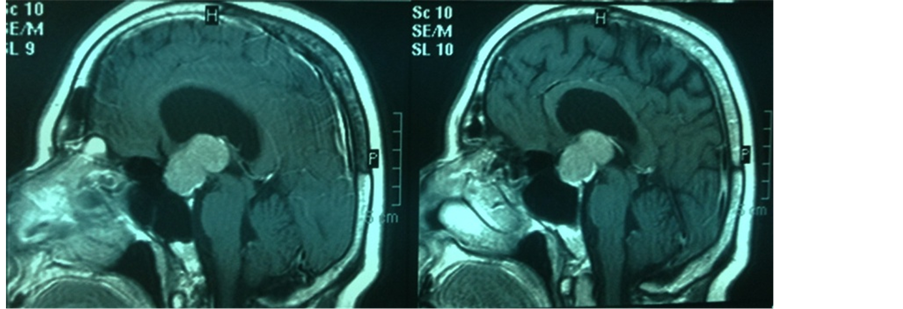 (c)
(c)
Figure 3. Axial (a), coronal (b) and sagittal (c) MRI images showinga isointense lesion in the suprasellar region with pressure effect on thethird ventricle. Hydrocephalusis seen.

Figure 4. Postoperative CT image showing residual pituitary mass in the suprasellar region.
structive hydrocephalus. Clinical presentation of a pituitary macroadenoma with obstructive hydrocephalus is extremely rare [8] . Therapy of PRL-secreting adenomas is circumscribed to medical therapy with dopamine agonists and surgery, whereas radiation therapy is recommended to the few patients not controlled by both medical and surgical treatments [9] [10] . However, some drawbacks of medical therapy, such as the need for life-long treatment in the majority of patients, side effects limiting compliance by the patient, and resistance of the tumor to dopamine agonists, are still of concern. In recent years, there has been a renewed interest in the surgical treatment of PRL-secreting tumors [11] . Surgery for large-to-giant pituitary adenomas is technically challenging. Usually, microsurgical treatment is recommended for most pituitary adenomas using a transsphenoidal approach [8] . The goals of surgery are to remove the tumor, relieve the mass effect, improve visual abnormalities, reduce hormone hypersecretion to normal levels, and preserve normal pituitary function [1] [12] . Although the transsphenoidal approach has been widely adopted as a safe and effective method for the removal of the majority of pituitary adenomas, large lesions may still present with considerable difficulties [13] -[15] . However, complete resection of tumors with excessive suprasellar extension may be difficult to achieve [8] . The present case highlights the fact that pituitary adenomas with obstructive hydrocephalus should be distinguished from other tumors especially colloid cysts as the prognosis and management with selection of the surgical ap-

Figure 5. Postoperative CT image shows that hydrocephalus has resolved.
 (a)
(a) (b)
(b) (c)
(c)
Figure 6. Axial (a), coronal (b) and sagittal (c) postoperative MRI imagesshowing residual pituitary mass. Hydrocephalus has resolved and theforamen of Monro is open.
proach differs significantly depending on the nature of the lesion. Therefore, the first step of microsurgical treatment (transnasal transsphenoidal approach) was to remove the tumor extending into third ventricle, to resolution of obstructive hydrocephalus. Subsequently, completing the residual tumor resection from suprasellar region will be removed by cranial surgery or the patient will be treated by medical therapy.
References
- Rotariu, D., Gaivas, S., Faiyad, Z., Iencean, A.S. and Poeata, L. (2011) Pituitary Adenoma, Therapeutic and Approach and Surgical Results. Romanian Neurosurgery, 4, 465-475.
- Liao, A.C., Wan, S.C., Tsai, F., Chen, Y.K. and Shen, Y.Y. (2002) Incidental Pituitary Macrodenoma Detected in FDG-PET: Three Cases Report. Annals of Nuclear Medicine, 15, 211-217.
- Thapar, K. and Kovacs, K. (1998) Tumors of the Sellar Region. In: Bigner, D.D., Mclendon, R.E. and Bruner, J.M., Eds., Russel and Rubinsteins Pathology of Tumors of the Nervous System, 6th Edition, Williams & Wilkins, Baltimore, 561.
- Scarone, P., Losa, M., Mortini, P. and Giovanelli, M. (2006) Obstructive Hydrocephalus and Intracranial Hypertension Caused by a Giant Macroprolactinoma. Prompt Response to Medical Treatment. Journal of Neuro-Oncology, 76, 51-54. http://dx.doi.org/10.1007/s11060-005-2319-0
- Cappabinaca, P., Cavallo, L.M., Colao, A., Del Basso De Caro, M., Esposito, F., Cirillo, S., et al. (2002) Endoscopic Endonasal Transphenoiodal Approach: Outcome Analysis of 100 Consecutive Procedures. Minimally Invasive Neurosurgery, 45, 193-200.http://dx.doi.org/10.1055/s-2002-36197
- Charalampaki, P., Reisch, R., Ayad, A., Conrad, J., Welschenhold, S., Perneczky, A., et al. (2007) Endoscopic Endonasal Pituitary Surgery: Surgical and Outcome Analysis of 50 Cases. Journal of Clinical Neuroscience, 14, 410-415.http://dx.doi.org/10.1016/j.jocn.2006.02.014
- Chole, R.A., Lim, C., Dunham, B., Chicoine, M.R. and Dacey, R.G. (2011) A Novel Transnasal Transsphenoidal Speculum: A Design for Both Microscopic and Endoscopic Transshenoidal Pituitary Surgery. Journal of Neurosurgery, 114, 1380-1385.
- Guo, F., Li, Z., Song, L. and Liu, X. (2013) One Exceedingly Rare Co-Existence of Pituitary Adenoma with Hydrocephalus and Cerebral Aneurysm: Case Repot and Literature Review. Life Science Journal, 10, 1447-1451.
- Ferda, P.U. and Wardlaw, S.L. (1999) Diagnosis and Treatment of Pituitary Tumors. The Journal of Clinical Endocrinology and Metabolism, 84, 3859-3866. http://dx.doi.org/10.1210/jcem.84.11.6202
- Molitch, M.E. (1999) Medical Treatment of Prolactinmas. Endocrinology Metabolism Clinics of North America, 28, 143-169.http://dx.doi.org/10.1016/S0889-8529(05)70061-X
- Losa, M., Mortini, P., Barzaghi, R., Gioia, L. and Giovanelli, M. (2002) Surgical Treatment of Prolactin-Secreting Pituitary Adenoma: Early Results and Long-Term Outcome. The Journal of Clinical Endocrinology and Metabolism, 87, 3180-3186. http://dx.doi.org/10.1210/jcem.87.7.8645
- Jackson, I.M.D. and Noren, G. (1999) Role of Gamma Knife Therapy in Management of Pituitary Tumors. Endocrinology Metabolism Clinics of North America, 28, 133-142. http://dx.doi.org/10.1016/S0889-8529(05)70060-8
- Alfieri, A., Jho, H.D. and Tschabitscher, M. (2002) Endoscopic Endonasal Approach to the Ventral Cranio-Cervical Junction: Anatomical Study. Acta Neurochirurgica (Wien), 144, 219-225. http://dx.doi.org/10.1007/s007010200029
- Bohinski, R.J., Warnich, R.E., Gaskill-Shipley, M.F., Zuccarello, M., Van Loveren, H.R., Kormos, D.W., et al. (2001) Intraoperative Magnetic Resonance Imaging to Determine the Extent of Resection of Pituitary Macroademonas during Transsphenoidal Microsurgery. Journal of Neurosurgery, 49, 1133-1144.
- Jho, H.D. and Ha, H.G. (2004) Endoscopic Endonasal Skull Base Surgery: Part 2—The Cavernous Sinus. Minimally Invasive Neurosurgery, 47, 9-15. http://dx.doi.org/10.1055/s-2004-818346
NOTES

*Corresponding author.

