Open Journal of Blood Diseases
Vol.2 No.4(2012), Article ID:25381,4 pages DOI:10.4236/ojbd.2012.2417
Repeat Whole Blood Donation Correlates Significantly with Reductions in BMI and Lipid Profiles and Increased Gamma Glutamic Transferase (GGT) Activity among Nigerian Blood Donors
![]()
1College of Health Technology, Otuogidi, Ogbia, Nigeria; 2Department of Haematology and Blood Transfusion, University of Calabar Teaching Hospital, Calabar, Nigeria; 3Haematology and Blood Transfusion Science Unit, Department of Medical Laboratory Science, College of Health Sciences, Niger Delta University, Wilberforce Island, Nigeria.
Email: *za.jeremiah@mail.ndu.edu.ng
Received October 5th, 2012; revised November 13th, 2012; accepted November 25th, 2012
Keywords: Blood Donation; Gamma Glutamic Transferase; Body Mass Index; Lipid Profiles
ABSTRACT
Background: The effect of repeated blood donation on some biochemical values of healthy adult male blood donors in Calabar, Nigeria was studied. Methods: One hundred and fifty three (153) healthy repeat blood donors and 90 first time blood donors constituted the study population. Samples were analyzed using colorimetric procedures. Results: The BMI values of 24.4 ± 2.4 kg/m2 in the first time donors was significantly higher than the 21.7 ± 1.7 kg/m2 obtained in repeat donors (P < 0.001). Among all the biochemical parameters, total cholesterol showed a significant change of 2.55 ± 0.74 mmol/l after repeated donations as compared to 3.45 ± 1.47 mmol/l in the first time donors (P < 0.005). Gamma glutamyl transferase (GGT) was significantly higher in repeat donors (70.5 ± 13.5 µl) than the first time donors (62.5 ± 13.3 µl) (P < 0.05). An LDL value of 1.02 ± 0.8 mmol/l in repeat donors was significantly lower than 1.69 ± 1.0 mmol/l in first time donors (P < 0.05). A VLDL value of 0.32 ± 0.2 mmol/l in repeat donors was equally lower than 0.44 ± 0.2 mmol/l obtained in the first time donors (P < 0.05). GGT showed positive correlation with lactate dehydrogenase (LDH) and low density lipoproteins (LDL) at P < 0.05 and P < 0.01 respectively among the repeat blood donors. Triglycerides showed a positive correlation with very low density lipoprotein (VLDL) among repeat donors at P < 0.05 significant level. Pearson correlation analysis also indicates that a significant positive relationship exists between GGT and low density lipoprotein (r = 0.891, P < 0.001). The regression analysis defined the relationship as linear (y = 0.0578x + 36.87; r2 = 0.7934, P < 0.05). Conclusion: A reduction in the values of some lipid profiles and high GGT activity is associated with repeated blood donations in this study population. Repeated blood donation may play a significant role in reducing the incidence of heart disease.
1. Introduction
The health benefits of screening for fatty liver and other components of the metabolic syndrome seems as necessary as performing tests for viral hepatitis B and C infections on the blood donors [1]. This is because an estimated 1% - 9% of people who have no symptoms are known to have high liver enzyme levels attributable to non alcoholic fatty liver disease whose risk factors have been known to be obesity, diabetes (insulin resistance), hyperlipidaemia and hypertension [2].
Blood donors are as a whole a protected group against coronary heart disease but according to Bharadwaj [3]there seems to be a reduction in benefit of blood donation as the duration from the date of last donation increases. Frequent blood donations have been reported to reduce the risk of myocardial infarction [4] and this is attributed to the reduction in the iron load with each blood donation [5]. Apart from iron, other biochemical parameters like gamma glutamic transferase (GGT) and lipid parameters play prominent roles in heart disease.
GGT is present in hepatocytes and biliary epithelial cells. The normal range is 0 - 50 U/L in men and 0 - 35 U/L in women. GGT elevation is the most sensitive marker of hepatobiliary disease. However, its routine clinic use is not recommended as it cannot by itself indicate a specific cause of liver disease. Elevated GGT in conjunction with alkaline phosphatase usually points to hepatobilliary injury [5-7]. Serum GGT activity has commonly been interpreted as a marker of alcohol consumption or liver disease [8].
A blood donor who indulges in unhealthy lifestyle of alcohol consumption may develop liver problem unnoticed, thereby constituting a risk in the blood donor pool. On the other hand, GGT is central to the extracellular catabolism of glutathione (GSH), a low molecular weight sulfhydryl compound which is a scavenger of oxygen free radicals and plays a key role in protecting against both intracellular and extracellular oxidative stress [9, 10]. However, GGT has been widely reported to be high in chronic heart failure patients and is also associated with disease severity [11].
Most studies are centered on the effect of blood donation on iron parameters probably due to the adverse consequences of anaemia or iron deficiency anemia [12,13]. Considering the lifestyle of most of our blood donors vis-a-vis excessive alcohol intake, smoking, etc. which has direct effect on hepatocytes, It therefore become necessary to look beyond anaemia to ensure a safety donor pool with minimal consequences on the blood recipients. This study was therefore aimed at determining the gamma glutamic transferase activity and lipid profiles of repeat donors in our setting for the purpose of establishing the baseline values.
2. Materials and Methods
2.1. Subjects
Two group of subjects participated in this study. The first group consisted of repeat donors (those who have donated blood at 3 to 4 times in a year for at least two consecutive years). The second group was the first time donors and consisted of men who were registered as new blood donors without any prior donations. Informed consent was received from each of the 103 repeat donors as well as from the 90 first time donors. The weights and heights of the participants were obtained and the body mass index (BMI) calculated as weight/height2. The blood pressure of the participants was also taken from each of them.
Four (4) milliliters of venous blood sample was collected from each subject, transferred into a plain bottle and used for biochemical analysis. Clotted blood samples in plain bottles were centrifuged at 2500 g for 5 minutes to separate the serum used for the analysis.
2.2. Gamma-Glutamyltransferase (GGT) Determination
GGT concentration was determined using human commercial kit which is based on the ability of the GGT in the sample to catalyze the transfer of the glutamyl group from GLUP-C to glycylglycine. The amount of 5-amino- 2-nitrobenzoate formed is proportional to GGT activeity and measured kinetically at 405 nm.
1.0 ml of the reagent containing glycylglycine, GLUPA-C, sodium azide and tris-buffer was put into test and control tubes already incubated at 37˚C. This was followed by the addition of 100 µl of the serum sample into the tubes. The contents of the tubes were mixed and incubated for 1 minute. The absorbance of the test and control were measured against the distilled water blank at 405 nm. The absorbance was repeated after 1 minute and the mean difference per minute multiplied by 1158 to obtain the result in microlitre (µl).
2.3. Lactate Dehydrogenase (LDH) Determination
LDH determination using the human kit is based on catalyses of the oxidation of lactate to pyruvate with simultaneous reduction of nicotinamide adenine dinucleotide (NAD) to NADH. The rate of NAD reduction can be measured as an increase in absorbance at 340 nm. This rate is directly proportional to LDH activity in serum.
1.0 ml of the reagent containing a mixture of NAD, L-lactate and buffer was put into test and control tubes already incubated at 37˚C. 50 µl of serum sample was added to these tubes, mixed and incubated for 30 seconds. The absorbance (A1) reading was done, then the tubes were re-incubated for another 1 minute and the absorbance (A2) measured. The change in the absorbance (A2-A1) was multiplied by the factor 3376 to obtain the result in microlitre. The absorbances of the test and control were measured against the distilled water blank at 340 nm.
2.4. Triglycerides Determination
10 µl each of sample and standard solutions were added to 1000 µl of the reagent containing lipases and quinoneimine indicator. It was mixed and incubated for 5 minutes at 37˚C. The absorbance of the sample and standard were measured against the reagent blank within 60 minutes.
2.5. Total Cholesterol Determination
1000 µl of the reagent containing a mixture of esterase, peroxidase and quinoneimine indicator was added to 10 µl of distilled water, standard and serum sample respectively in three different test tubes. The contents were mixed and incubated for 5 minutes at 37˚C. The absorbance of the sample and of the standard against the blank at 500 nm was determined.
2.6. High Density Lipoprotein (HDL) Cholesterol
1000 µl of the reagent was added to 100 µl of distilled water, supernatant from sample and standard supernatant respectively in three different test tubes. The contents were mixed and incubated for 5 minutes at 37˚C. The absorbances of the sample and of the standard were measured against the reagent blank at 500 nm. Low density lipoprotein (LDL) Cholesterol was calculated as follows:
LDL = Total Cholesterol-Triglycerides/2.2-HDL Cholesterol.
2.7. Statistical Analysis
The statistical analysis was done using SPSS statistical package (version 15 Chicago, IL, USA). All results were calculated as mean ± SD and a P value of ≤ 0.05 was considered statistically significant. Mean values were compared using the paired t-test. Pearson correlation analysis was performed to determine the factors affecting changes in donor parameters after repeated blood donations.
3. Results
A total of two hundred and fourty three (243) blood donors participated in this study. Ninety (37.0%) of them were first time donors while one hundred and fifty three (63.0%) were repeat donors. Majority of them (73.3%) were under 30 years of age while 26.7% were between 31 - 35 years. None of the blood donors was above 35 years. All the donors in the repeat category were under 30 years of age. All the blood donors were males.
Table 1 shows the blood pressure, age, BMI and biochemical parameters of the 243 blood donors who participated in the study. There was no significant difference in the age and blood pressure parameters. The BMI values of 24.4 ± 2.4 kg/m2 in the first time donors was significantly higher than the 21.7 ± 1.7 kg/m2 obtained in repeat donors (P < 0.001). Gamma glutamyl transferase was significantly higher in repeat donors (70.5 ± 13.5 µl) than the first time donors (62.5 ± 13.3 µl) (P < 0.05). Lactate dehydrogenase enzyme showed no significant changes in the values between the two groups (P = 0.948).
Table 2 shows the lipid profile of the two categories of donors. Total cholesterol decreased significantly in repeat donors to the value of 2.6 ± 0.7 µl when compared with 3.5 ± 1.5 µl obtained in first time blood donors (P < 0.05). Similarly, LDL and VLDL values were decreased significantly in repeat donors. An LDL value of 1.02 ± 0.8mmol/l in repeat donors was significantly lower than 1.69 ± 1.0 mmol/l in first time donors. A VLDL value of 0.32 ± 0.2 mmol/l in repeat donors was equally lower than 0.44 ± 0.2mmol/l obtained in the first time donors. High density lipoproteins and triglycerides values did not differ significantly when the two categories were compared. Pearson correlation analysis indicate that a significant positive relationship exists between GGT and low density lipoprotein (r = 0.891, P < 0.001). The regression analysis defined the relationship as linear (y = 0.0578x + 36.87; r2 = 0.7934, P < 0.05).
4. Discussion
Reports from different parts of the world showed that there is dyslipidaemia in repeat blood donors [4,13,14]. This common finding from different authors on the reduced total cholesterol level among repeat blood donors has further been confirmed in this study. Because high body iron stores have been suggested as a risk factor for myocardial infarction, donation of blood could reduce
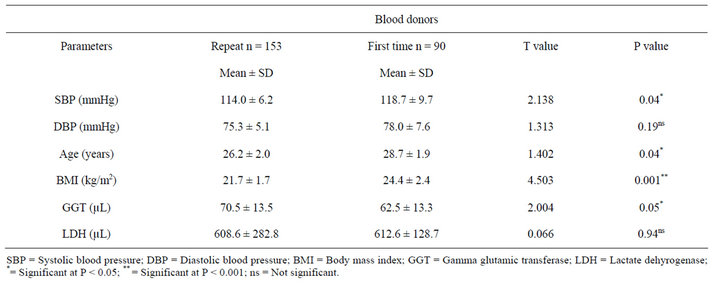
Table 1. Blood pressure, anthropometric indices and biochemical parameters of 243 participants.

Table 2. Lipid profile of first time and repeat donors in 243 blood donors.
the risk by lowering body iron stores The reason for this reduction was attributed to the “iron hypothesis” which proposed that the reduction in the iron load with each blood donation was the reason for the fall in incidence of cardiovascular problems [15].
In this study, no variation was observed in serum gamma glutamic transferase and LDH of the repeated blood donors when compared with the first time donors. Similarly, no significant associations between GGT and age, BMI and anthropometric measurements as substantiated by the works of Giral et al. [15]. However, Khedmat et al. [1] were of contrary opinion. In their works, there was a highly significant association between GGT and age, BMI, blood pressure, serum lipids and lipoproteins. Long term deleterious effects of repeated blood donations may be masked by the donor’s life style [16].
5. Conclusion
This study has further confirmed that repeated blood donations could lead to the reduction in the lipid profiles of the blood donors.
REFERENCES
- H. Khedmat, F. Fallahian, H. Abolghasemi, B. Hajibeigi, Z. Attarchi, F. Alaeddini, M. T. Holisaz, M. Pourali, S. Sharifi and N. Zarei, “Serum G-Glutamyltransferase, Alanine Aminotransferase and Aspartate Aminotransferase Activity in Iranian Healthy Blood Donor Men,” World Journal of Gastroenterology, Vol. 13, No. 6, 2007, pp. 889-894.
- G. N. Ioanou, E. J. Boyko and S. P. Lee, “The Prevalence and Predictors of Elevated Serum Aminotransferase Activity in the United States in 1999-2002,” American Journal of Gastroenterology, Vol. 101, No. 1, 2006, pp. 76-82. HUdoi:10.1111/j.1572-0241.2005.00341.xU
- R. S. Bharadwaj, “A Study of Lipid Profiles among Male Voluntary Blood Donors in Chennai City,” Indian Journal of Community Medicine, Vol. 30, No. 1, 2005, pp. 1-5.
- T. Pekka and R. Salonen, “Cohort Study of Relationship between Donating Blood and the Risk of Myocardial Infarction,” British Medical Journal, Vol. 314, No. 7083, 1997, pp. 793-794. HUdoi:10.1136/bmj.314.7083.793U
- A. Gebre-Yohannes and S. I. Rehelbeck, “Coronary Heart Disease Risk Factors among Blood Donors in North West Ethiopia,” East African Medical Journal, Vol. 75, No. 9, 1998, pp. 495-500.
- G. Aragon and Z. M. Younossi, “When and How to Evaluate Mildly Elevated Liver Enzymes in Apparently Healthy Patients,” Cleveland Clinic Journal of Medicine, Vol. 77, No. 3, 2010, pp. 195-204. HUdoi:10.3949/ccjm.77a.09064U
- C. A. Burtis and E. R. Ashwood, “Tietz Fundamentals of Clinical Chemistry,” 5th Edition, WB Saunders, Philadelphia, 2001, pp. 463-493.
- M. Kravos and I. Malesic, “Kinetics and Isoforms of Serum Glutamate Dehydrogenase in Alcohols,” Alcohol and Alcoholism, Vol. 43, No. 3, 2007, pp. 281-286.
- J. B. Whitefield, “Gamma Glutamic Transferase,” Critical Reviews in Clinical Laboratory Science, Vol. 38, No. 4, 2001, pp. 263-355.
- G. Wu, Y. Z. Fang, S. Yang, J. R. Lupton and N. D. Turner, “Glutathione Metabolism and Its Implications for Health,” The Journal of Nutrition, Vol. 134, No. 3, 2004, pp. 489-492.
- G. Poelz, C. Eberl, H. Achrainer and H. Ulmer, “Prevalence of Elevated GGT and Prognostic Significance of GGT in Chronic Heart Failure,” Circulation and Heart Failure, Vol. 2, No. 4, 2009, pp. 294-302.
- Z. A. Jeremiah and B. B. Koate, “Anaemia, Iron Deficiency and Iron Deficiency Anaemia among Blood Donors in Port Harcourt, Nigeria,” Blood Transfusion, Vol. 8, No. 2, 2010, pp. 113-117.
- D. G. Meyers, D. Strickland, P. A. Maloley, J. K. Seburg, J. E. Wilson and B. F. McManus, “Possible Association of a Reduction in Cardiovascular Events with Blood Donation,” Heart, Vol. 78, No. 2, 1997, pp. 188-193.
- J. T. Salonen and T. P. Toumainnen, “Donating Blood Is Associated with Reduced Risk of Myocardial Infarction. The Kuopio Ischemic Heart Disease Risk Factor Study,” American Journal of Epidemiology, Vol. 148, No. 5, 1998, pp. 445-451. HUdoi:10.1093/oxfordjournals.aje.a009669U
- P. Giral, V. Ratziu and J. C. Chapman, “Letter Regarding Article by Ruttmann et al., ‘γ-Glutamyltransferase as a Risk Factor for Cardiovascular Disease Mortality: An Epidemiological Investigation in a Cohort of 163 944 Austrian Adults’,” Circulation, Vol. 113, No. 8, 2006, pp. e299-e300. HUdoi:10.1161/CIRCULATIONAHA.105.594176U
- G. Edgren, M. Reilly, H. Hjalgrim, J. Adami, K. Rostgarrd, A. Shanwell and M. Melbye, “Donation Frequency, Iron Loss and Risk of Cancer among Blood Donors,” Journal of the National Cancer Institute, Vol. 100, No. 8, 2008, pp. 572-579. HUdoi:10.1093/jnci/djn084UH
NOTES
*Corresponding author.

