Open Journal of Ophthalmology
Vol.3 No.2(2013), Article ID:31270,3 pages DOI:10.4236/ojoph.2013.32011
Pseudo-Glaucoma after Hypertensive Retinopathy
![]()
Department of Ophthalmolgy, Faculty of Medicine, Shimane University, Izumo, Japan.
Email: tanito-oph@umin.ac.jp
Copyright © 2013 Katsunori Hara et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received March 2nd, 2013; revised April 3rd, 2013; accepted May 2nd, 2013
Keywords: Hypertensive Retinopathy; Pseudo-Glaucoma; Retinal Nerve Fiber Layer Defects (NFLD); Spectral-Domain Optical Coherence Tomography (SD-OCT)
ABSTRACT
A 35-year-old Japanese woman showed the typical fundus appearance of acute hypertensive retinopathy, including multiple cotton-wool spots, retinal hemorrhages, star exudates, and disc edema bilaterally. Her systemic blood pressure was high (246/158 mmHg). Nephrologists diagnosed her with secondary hypertension due to immunoglobulin A nephropathy. After 2 years, all signs of acute retinopathy resolved and only multiple striated or sectorial darkening of the fundus (retinal nerve fiber layer defects [NFLD]) remained. Computerized analysis of the macular thickness measurement by optical coherence tomography alerted the risk of glaucoma. NFLD is a hallmark of early glaucoma which is more reliable than IOP elevations since normal tension glaucoma is popular in Japan. To differentiate this case from true glaucoma, information regarding her past history is critical for her future ophthalmologists.
1. Introduction
The Glaucoma, the leading cause of irreversible blindness worldwide [1], is characterized by progressive “glaucomatous” optic neuropathy and corresponding visual field loss. Thus, a diagnosis of glaucoma is established primarily based on the morphologic fundus appearance. However, several systemic disease-related ocular conditions such as diabetic retinopathy [2,3], interferon retinopathy [4], and cotton-wool spots (CWS) of unknown etiology but presumably from chronic hypertension [ 5 ] form fundus lesions that resemble glaucomatous neuronal damage and can compromise the glaucoma diagnosis. We report a case with acute hypertensive retinopathy that could be misdiagnosed as true glaucoma after remission of the retinopathy.
2. Case Report
A 35-year-old Japanese woman noticed blurred vision 1 week before visiting our hospital. Her intraocular pressure (IOP) was normal (14 mmHg) bilaterally. The fundus appearance, including multiple CWS, retinal hemorrhages, star exudates, and disc edema (Figures 1(A) and (B)), were all typical of acute hypertensive retinopathy. Her systemic blood pressure was high (246/158 mmHg). Nephrologists diagnosed her with secondary hypertension due to immunoglobulin A nephropathy. After 2 weeks of antihypertensive therapy, her blood pressure normalized and the visual acuity returned to 1.2 bilaterally (from 0.8 right and 1.2 left). After 2 years, all signs of acute retinopathy resolved and only multiple striated or sectorial darkening of the fundus (retinal nerve fiber layer defects [NFLD]) remained (Figures 1(C) and (D)). Computerized analysis of the macular thickness measurement by optical coherence tomography (OCT) (RS-3000, Nidek, Aichi, Japan) alerted us to the risk of glaucoma (Figures 1(E) and (F)).
3. Discussion
NFLD is a hallmark of early glaucoma that is more reliable than IOP elevations since glaucoma often can develop without elevations of IOP out of the normal range (normal tension glaucoma) [ 6 ]. To differentiate this case from true glaucoma, information regarding her past history is critical for her future ophthalmologists. Patients with acute severe hypertension might be treated only for the hypertension without making a diagnosis of acute hypertensive retinopathy. Thus, not only is it critical for ophthalmologists to obtain patients’ past histories but providing information regarding possible pseudo-glaucoma to patients from physicians who treat hypertension also would be beneficial to avoid misdiagnosis as in the current case.
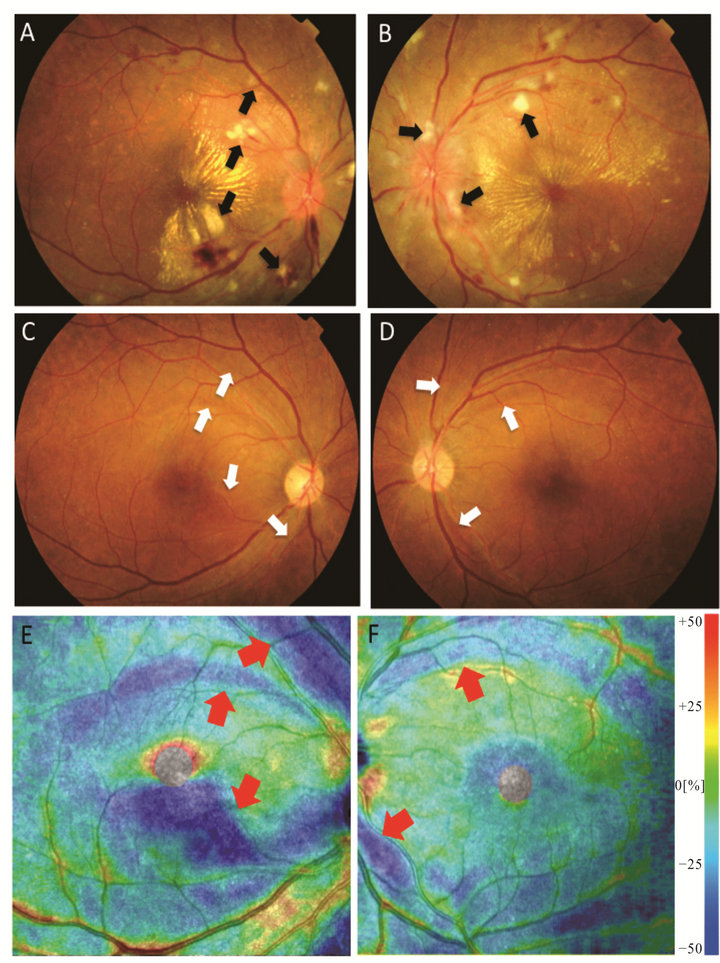
Figure 1. Focal loss of retinal nerve fibers after remission of acute hypertensive retinopathy. Multiple cotton-wool spots (CWS) (arrows) are seen in the acute phase on fundus photography (A, B). After normalization of blood pressure, focal nerve fiber losses resembling early glaucomatous signs are seen on fundus photography at the same locations of the past CWS (C, D; arrows) and the inner retinal thickness map obtained using optical coherence tomography (E, F; arrows). (A, C, E), right eye; (B, D, F), left eye.
4. Conclusion
Although NFLD is a sensitive sign of early glaucoma, some retinal diseases including acute hypertensive retinopathy also form NFLD. Since glaucoma with normal IOP level is common, patient’s past history is critical to avoid making a misdiagnosis of glaucoma in such cases.
REFERENCES
- A. Foster and S. Resnikoff, “The Impact of Vision 2020 on Global Blindness,” Eye (London, England), Vol. 19, No. 10, 2005, pp. 1133-1135. doi:10.1038/sj.eye.6701973
- L. M. Alencar, F. A. Medeiros and R. Weinreb, “Progressive Localized Retinal Nerve Fiber Layer Loss Following a Retinal Cotton Wool Spot,” Seminars in Ophthalmology, Vol. 22, No. 2, 2007, pp. 103-104. doi:10.1080/08820530701420058
- E. Chihara, T. Matsuoka, Y. Ogura and M. Matsumura, “Retinal Nerve Fiber Layer Defect as an Early Manifestation of Diabetic Retinopathy,” Ophthalmology, Vol. 100, No. 8, 1993, pp. 1147-1151.
- K. Hara, M. Tanito and A. Ohira, “Retinal Nerve Fibre Layer Defects Associated with Cotton-Wool Spots in Patients with Interferon Retinopathy,” Acta Ophthalmologica, Vol. 90, No. 2, 2012, pp. e158-e160. doi:10.1111/j.1755-3768.2011.02106.x
- J. W. Koh, K. H. Park, M. S. Kim and J. M. Kim, “Localized Retinal Nerve Fiber Layer Defects Associated with Cotton Wool Spots,” Japanese Journal of Ophthalmology, Vo. 54, No. 4, 2010, pp. 296-299. doi:10.1007/s10384-010-0830-0
- A. Iwase, Y. Suzuki, M. Araie, T. Yamamoto, H. Abe, K. Shirato, Y. Kuwayama, H. K. Mishima, H. Shimizu, G. Tomita, Y. Inoue and Y. Kitazawa, “The Prevalence of Primary Open-Angle Glaucoma in Japanese: The Tajimi Study,” Ophthalmology, Vol. 111, No. 9, 2004, pp. 1641- 1648.

