Open Journal of Orthopedics
Vol.3 No.3(2013), Article ID:34522,4 pages DOI:10.4236/ojo.2013.33034
Intraoperative Periprosthetic Femoral Fractures Related to Austin Moore Hemiarthroplasty—A Retrospective Review of 365 Patients*
![]()
Hip Unit at the Department of Orthopaedic Surgery, Hospital Clínic, University of Barcelona, Barcelona, Spain.
Email: #jenarofv@clinic.ub.es
Copyright © 2013 J. A. Fernández-Valencia et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received May 3rd, 2013; revised June 3rd, 2013; accepted June 15th, 2013
Keywords: Hip Hemiarthroplasty; Intraoperative Fracture; Complication
ABSTRACT
Intraoperative periprosthetic femoral fractures (IPFF) have been studied extensively for total hip arthroplasties, but not for hemiarthroplasties. Recent series in the literature show an IPFF rate for hemiarthroplasties ranging from 0% to 14%. The present study was designed to determine the prevalence and outcome after IPFF during non-cemented hemiarthroplasty. In addition, the surgical step at higher risk to produce these fractures was evaluated in an attempt to identify strategies that could minimize the prevalence of this complication. We performed an observational study of 365 consecutive patients undergoing and Austin-Moore hemiarthroplasty from 2005 to 2006 at our institution. The institutional IPFF rate was 6.8% (twenty-five out of 365). The moment at which the fracture was detected was collected: 1) intraoperatively and 2) in the postoperative radiological control. The surgical step in which the fracture occurred was collected: 1) neck osteotomy, 2) broaching, 3) prosthesis introduction, and 4) reduction. Results were compared to a control group according to blood transfusion rate, mortality rate and revision surgery rate. The fractures were detected during the surgery in twenty cases (80%); for the five remaining cases the fracture was only detected in the postoperative radiology. For those detected during the surgery, the two most common manouvers in which the fracture occurred was hip reduction (10 cases) and prosthesis introduction (7 cases). The blood transfusion rate, first-month mortality rate and revision surgery rate showed no statistical difference between the two groups (p = 0.3). In the present series, most of IPFF during Austin-Moore hemiarthroplasty implantation, occurred during arthroplasty reduction. Difficulties during this step should lead the surgeon to reconsider if technical mistakes are present and can be solved. However, if fracture occurs, adequate treatment of IPFF should provide satisfactory results without increasing blood transfusion needs, mortality or revision surgery.
1. Introduction
Intraoperative periprosthetic femoral fractures (IPFF) have been studied extensively for total hip arthroplasties, and revision surgery of THA shows the higher risk for this complication [1]. In a large cohort study, it was reported that IPFF were encountered during 1% (238) of 23,980 primary THA compared with 7.8% (497) of 6349 revisions [2], and other studies have shown similar results [3-5].
Whereas the literature attention on prevention of IPFF is focused on total hip arthroplasty and mostly for revision procedures, very recent studies show that the primary arthroplasty at the higher risk of IPFF is the uncemented hemiartroplasty in the elderly [6-8]. Despite hemiarthroplasty remains the goldstandard treatment for femoral neck fractures in the elderly, these fractures and their treatment have been under-reported in the literature [6].
The present study aims to determine the incidence of IPFF implanting the Austin-Moore arthroplasties in the elderly patient at our institution, the surgical step at higher risk to produce these fractures and the outcomes regarding a control group without IPFF.
2. Material and Methods
A retrospective study was performed in 365 consecutive Austin-Moore arthroplasties implanted in 354 skeletally mature patients, between January 1st, 2005 and December 31st, 2006. Ethics Committee decided approval was not required for this study.
All operations were performed by experienced surgeons or residents under direct supervision of an experienced surgeon. The lateral transgluteal approach modified by Hardinge [9] was done in all the cases, and intraoperative radiology was performed in all cases after the hemiarthroplasty implantation. Also according to our institution protocol, three days after the surgery a radiological study was also performed, including anteroposterior radiology of the pelvis, and lateral view of the operated side.
The medical records were reviewed to identify the cases in which an IPFF occurred. A total of twenty-five cases were identified (Group 1), and thus the institutional IPFF rate was 6.8%. The twenty-five patients who had an IPFF were thirteen women and twelve men with a mean age of 84 years (range, seventy-five to ninety-seven years). The fracture affected the right side in 16 cases.
The moment at which the fracture was detected was collected: 1) intraoperatively (both by direct visualization or by using intraoperative radiology) and 2) in the postoperative radiological control. For those fractures occurred during the surgery, the surgical maneuver in which the fracture occurred was collected: 1) neck osteotomy, 2) broaching, 3) prosthesis introduction, and 4) reduction.
The description of the fracture was performed according to the validated Vancouver system for classifying postoperative periprosthetic femoral fractures adapted for use in the intraoperative period [10]. According to this classification system, the femur was divided into three anatomical areas: A (the pertrochanteric region), B (the diaphysis), and C (the distal metaphyseal, or supracondylar, region). In each anatomic location, the fracture was further subclassified as 1) cortical perforation; 2) undisplaced linear crack; 3) displaced or unstable fractures. The type of treatment for the periprosthetic fracture was registered.
The Group 1 was compared to a control group of patients (Group 2). The Group 2 was 30 consecutive patients with Austin-Moore arthroplasties that did not sustain an IPFF, which underwent surgery between September 1st, 2006 and November 1st, 2006.
For both groups the following data was obtained: age, gender, ASA score and time waiting for the surgery (days). Results were compared between the two groups according to blood transfusion, first-month mortality and revision surgery rates.
Data was registered and analyzed with OpenEpi, version 2.3 (available at http://www.openepi.com). Descriptive statistics were calculated for all variables. Chi square test was used to compare transfusion rate and first-month mortality rate between the two groups. The P value was set prior to analysis at 0.05.
3. Results
The fractures were detected during the surgery in twenty cases (80%); for the five remaining cases the fracture was only detected in the postoperative radiology. All the fractures detected in the postoperative radiology were greater trochanter fractures, and were considered to have occurred unnoticed during the surgical procedure.
The IPFF were classified as Vancouver A2 in fourteen cases and A3 in eleven cases. No intraoperative Vancouver A1 fractures occurred, nor any Vancouver B or C type fractures. For those IPFF detected during the sugery, the moment in which the fracture occurred was; ten cases during hip reduction, seven cases during prosthesis introduction, one case during the femoral neck osteotomy, one case during broaching and in one case a dislocation and a periprosthetic fracture was observed in the intraoperative radiology control.
The intraoperative PPF was wired with one cerclage in 10 cases, and with two cerclages in 4 cases. The indication was changed to a cemented hemiarthroplasty and cerclage wire in 3 cases, and in the last 3 cases the Austin-Moore arthroplasty was stable and did not require any additional treatment (Figure 1).
The control group (Group 2) was comparable according to sex, age and ASA rating, and for both groups the mean the time waiting for the surgical procedure was 3 days. There was a trend towards an increased number of re-operated patients in the group presenting an IPFF Vancouver type A fracture compared with the control group, 16% vs 3%, respectively but it did not show a difference statistically significant. The blood transfusion rate (16% vs 25%) and first-month mortality rate (12% vs 11%) were similar between the two groups (p > 0.05).
4. Discussion
In a recent UK survey, Crosmann et al. reported that for active patients bipolar arthroplasty was most commonly
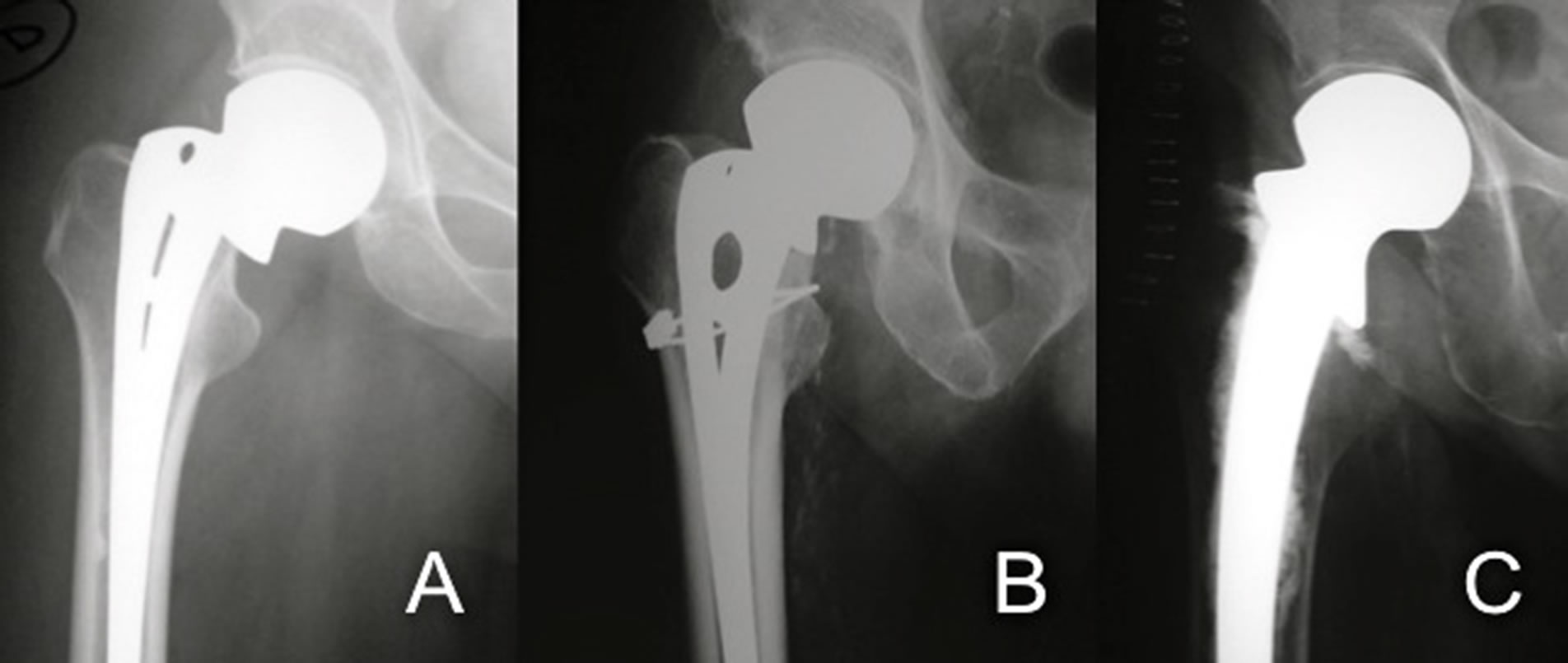
Figure 1. Treatment options for IPFF.
used (41%), while for the frail patients AMP or Thompson hemiarthroplasties were undertaken in 94% of the UK hospitals [11].
While problems with post-operative complications, delayed healing, implant loosening and increased mortality rates have been well described previously, the intraoperative PPF performing hemiarthroplasty, and its management has been insufficiently studied in the published literature [6].
Our institutional IPFF rate has been 6.8%. Most of the series dealing with Austin-Moore arthroplasties do not indicate or focus on IPFF [12-15]. In order to determine the incidence of IPFF related to Austin-Moore arthroplasties, the information can be obtained from the literature regarding the comparison group in prospective studies for the treatment of femoral neck fractures. Singh et al. reported the incidence of one intra-operative PPF in the Austin-Moore arthroplasty group (29 patients, 3.4%) [16]. Khan et al. reported three (2.5%) iatrogenic femoral fractures associated with cementless Austin-Moore arthroplasty insertion [17], and Pryor who assessed 91 of those hemiarthroplasties over a 12-month period, reported one periprosthetic femoral fracture (1.1%), which required re-operation [12]. A higher incidence was reported by Foster et al [6]; in their series this complication occurred in 5 patients over a total of 70 (7%). Weinrauch et al. presented the results of a multicentre retrospective study over 380 Austin-Moore arthroplasties, and revealed that 11.8% of the cases presented an IPFF [8]. In another study by Weinrauch, about surgical mistakes during the Austin-Moore prosthesis implantation, a 14% of intraoperative fractures was reported among a total of 147 consecutive cases [7]. As a conclusion, the incidence of IPFF related to an Austin-Moore arthroplasty has been reported from 0 to 14%.
Different strategies are possible in order to minimize the prevalence of this complication. It has been advocated the use of cemented hemiarthroplasty since bone cement is expected to reinforce the osteoporotic proximal femur in the frail elderly patient [6]. However, cement insertion has been shown to adversely affect pulmonary and cardiovascular function during the conduct of surgery and the immediate postoperative period, which may be poorly tolerated in the elderly with pre-existing comorbidity [18]. It has been outlined of paramount importance to rule out well known technical defects implanting the Austin Moore arthroplasty such as: 1) inadequate length of the neck remnant, 2) inadequate calcar seating, and 3) the presence of difference size in the prosthetic head compared with the contralateral normal femoral head [12,14]. In the present study, we indicate that the most dangerous moment to produce a fracture during AMP is hip reduction, and we suggest to consider if any those technical defects are present, especially if reduction turns to be difficult.
Our study has several weaknesses: it was a retrospective study, and the treatment of the intraoperative periprosthetic fracture was performed according to the preference of the orthopaedic surgeon. However, there is limited information regarding the results of the treatment of Vancouver type A fractures related to AMP [5,8], and the present series contributes to outline the importance of this complication. Although the mortality and transfusion rate did not increase comparing to those cases without IPFF, a moderate trend towards a higher reoperation rate was observed in the group with intraoperative fracture.
A higher sample would be needed to confirm this association.
As a final conclusion, intraoperative periprosthetic femoral fractures in Austin-Moore arthroplasties are underreported and in the present series the rate was 6.8%. More studies are needed to determine strategies for prevention and treatment of this condition. We would suggest that any difficulty in hip reduction must orientate us to reconsider if any technical mistake must be solved, and we advocate fracture stabilization by using cerclage wires or cables for Vancouver B2 intraoperative fractures and a cemented hemiarthroplasty plus cerclage for Vancouver B3 intraoperative fractures.
REFERENCES
- F. Rayan and F. Haddad, “Periprosthetic Femoral Fractures in Total Hip Arthroplasty: A Review,” Hip International, Vol. 20, No. 4, 2010, pp. 418-426.
- D. J. Berry, “Epidemiology: Hip and Knee,” Orthopedic Clinics of North America, Vol. 30, No. 2, 1999, pp. 183- 190. doi:10.1016/S0030-5898(05)70073-0
- M. M. Taylor, M. H. Meyers and J. P. Harvey Jr., “Intraoperative Femur Fractures during Total Hip Replacement,” Clinical Orthopaedics and Related Research, Vol. 137, 1978, pp. 96-103.
- P. A. Mitchell, N. V. Greidanus, B. A. Masri, D. S. Garbuz and C. P. Duncan, “The Prevention of Periprosthetic Fractures of the Femur during and after Total Hip Arthroplasty,” Instructional Course Lectures, Vol. 52, 2003, pp. 301-308.
- R. G. Molli, A. V. Lombardi Jr., K. R. Berend, J. B. Adams and M. A. Sneller, “A Short Tapered Stem Reduces Intraoperative Complications in Primary Total Hip Arthroplasty,” Clinical Orthopaedics and Related Research, Vol. 470, No. 2, 2012, pp. 450-461. doi:10.1007/s11999-011-2068-7
- A. P. Foster, N. W. Thompson, J. Wong and A. P. Charlwood, “Periprosthetic Femoral Fractures—A Comparison between Cemented and Uncemented Hemiarthroplasties,” Injury, Vol. 36, No. 3, 2005, pp. 424-429. doi:10.1016/j.injury.2004.07.023
- P. Weinrauch, “Intra-Operative Error during Austin Moore Hemiarthroplasty,” Journal of Orthopaedic Surgery, Vol. 14, No. 3, 2006, pp. 249-252.
- P. C. Weinrauch, W. R. Moore, D. R. Shooter, M. P. Wilkinson, E. M. Bonrath, N. J. Dedy, T. J. McMeniman, M. K. Jabur, S. L. Whitehouse and R. W. Crawford, “Early Prosthetic Complications after Unipolar Hemiarthroplasty,” ANZ Journal of Surgery, Vol. 76, No. 6, 2006, pp. 432- 435. doi:10.1111/j.1445-2197.2006.03757.x
- K. Hardinge, “The Direct Lateral Approach to the Hip,” Journal of Bone and Joint Surgery (British), Vol. 64, No. 1, 1982, pp. 17-19.
- D. Davidson, J. Pike, D. Garbuz, C. P. Duncan and B. A. Masri, “Intraoperative Periprosthetic Fractures during Total Hip Arthroplasty. Evaluation and Management,” Journal of Bone and Joint Surgery (American), Vol. 90, No. 9, 2008, pp. 2000-2012. doi:10.2106/JBJS.H.00331
- P. T. Crossman, R. J. Khan, A. MacDowell, A. C. Gardner, N. S. Reddy and G. S. Keene, “A Survey of the Treatment of Displaced Intracapsular Femoral Neck Fractures in the UK,” Injury, Vol. 33, No. 5, 2002, pp. 383-386. doi:10.1016/S0020-1383(02)00002-5
- G. A. Pryor, “A Study of the Influence of Technical Adequacy on the Clinical Result of Moore hemiarthroplasty,” Injury, Vol. 21, No. 6, 1990, pp. 361-365. doi:10.1016/0020-1383(90)90119-F
- K. J. Ravikumar and G. Marsh, “Internal Fixation versus Hemiarthroplasty versus Total Hip Arthroplasty for Displaced Subcapital Fractures of Femur-13 Year Results of a Prospective Randomised Study,” Injury, Vol. 31, No. 10, 2000, pp. 793-797. doi:10.1016/S0020-1383(00)00125-X
- K. M. Sharif and M. J. Parker, “Austin Moore Hemiarthroplasty: Technical Aspects and Their Effects on Outcome, in Patients with Fractures of the Neck of Femur,” Injury, Vol. 33, No. 5, 2002, pp. 419-422. doi:10.1016/S0020-1383(02)00041-4
- W. P. Yau and K. Y. Chiu, “Critical Radiological Analysis after Austin Moore Hemiarthroplasty,” Injury, Vol. 35, No. 10, 2004, pp. 1020-1024. doi:10.1016/j.injury.2003.08.016
- G. K. Singh and R. G. Deshmukh, “Uncemented AustinMoore and Cemented Thompson Unipolar Hemiarthroplasty for Displaced Fracture Neck of Femur: Comparison of Complications and Patient Satisfaction,” Injury, Vol. 37, No. 2, 2006, pp. 169-174. doi:10.1016/j.injury.2005.09.016
- R. J. Khan, A. MacDowell, P. Crossman, A. Datta, N. Jallali, B. N. Arch and G. S. Keene, “Cemented or Uncemented Hemiarthroplasty for Displaced Intracapsular Femoral Neck Fractures,” International Orthopaedics, Vol. 26, No. 4, 2002, pp. 229-232. doi:10.1007/s00264-002-0356-2
- A. J. Donaldson, H. E. Thomson, N. J. Harper and N. W. Kenny, “Bone Cement Implantation Syndrome,” British Journal of Anaesthesia, Vol. 102, 2009, pp. 12-22. doi:10.1093/bja/aen328
NOTES
*The authors declare the absence of conflict of interests.
#Corresponding author.

