Open Journal of Anesthesiology
Vol.3 No.3(2013), Article ID:31254,5 pages DOI:10.4236/ojanes.2013.33033
Different Effects of Right and Left Stellate Ganglion Block on Systolic Blood Pressure and Heart Rate
![]()
1Chishukai Taneyama Clinic, Shiojiri City, Japan; 2Department of Anesthesiology, University of Kansas Medical Center, Rainbow Boulevard, Kansas City, USA.
Email: *sigeru-yokota@suwa.jrc.or.jp
Copyright © 2013 Shigeru Yokota et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received February 15th, 2013; revised March 30th, 2013; accepted April 15th, 2013
Keywords: Stellate Ganglion Block; Hypertension; Hypotension; Heart Rate
ABSTRACT
Purpose: Whether or not right and left stellate ganglion blocks (SGB) affect blood pressure (BP) and heart rate (HR) differently has been controversial. The aim of this study was to analyze BP and HR changes after large numbers of right or left SGBs. Methods: A total of 16,404 right SGBs and 13,766 left SGBs were performed with 6 ml of 1% mepivacaine using the anterior paratracheal approach at C6. Changes in systolic BP and HR 30 min after SGBs were compared to the baseline values. Results: Systolic BP decreased by 25 to 49 mmHg in 10.93% and more than 50 mmHg in 0.67% of 16,404 right SGBs. Those percentages were significantly higher than corresponding percentages; 8.43% and 0.49% of 13,766 left SGBs (P < 0.0001 and P < 0.05, respectively). On the other hand, systolic BP increased by 25 - 49 mmHg in 5.74% and more than 50 mmHg in 0.52% of left SGBs, and in 4.15% and 0.18% of right SGBs (P < 0.0001 and P < 0.0001 between left and right SGBs, respectively). Right SGB caused marked reduction in HR (greater than 30 beats/min), more than left SGB (4.22% versus 2.70%, P < 0.0001). Conclusions: Both right and left SGBs could produce clinically significant hypertension and hypotension, and also severe bradycardia. However, right SGB produces a higher incidence of significant reductions in systolic BP and HR, compared to left SGB. On the other hand, left SGB produces a significant increase in systolic BP compared to right SGB. Those differences likely stem from the hemispheric asymmetry in autonomic cardiovascular control.
1. Introduction
There have been conflicting reports as to whether right stellate ganglion block (SGB) and left SGB affect systolic blood pressure (systolic BP) and heart rate (HR) differently. Roger and colleagues [1] concluded that only right SGB resulted in bradycardia. In this study, however, systolic BP changes after SGB were not reported. Kashima and colleagues [2] also found out that only right SGB produced a significant increase in the RR interval. Goh et al. [3] reported that blood pressure did not change after either right or left SGB but heart rate decreased significantly only after right SGBs. Gardner and colleagues [4] could not find any changes in the electrophysiological and mechanical indices with unilateral block of the stellate ganglions. Similarly, Lobata and colleagues [5] did not observe differences in systolic BP and HR between right and left SGB. The report by Kimura et al.
[6] suggests that incidence of severe hypertension may be higher with left SGB than with right SGB.
We believe that small numbers of right and left SGBs in those studies were one contributing factor in the controversy as to how differently right and left SGBs affect systolic BP and HR. Larger sample sizes are necessary to find out the incidence of clinically significant changes of BP and HR since subjects respond differently each time to repeated and successful SGBs. The objective of this study was, therefore, to analyze systolic BP and HR changes in large sample sizes of right and left SGB procedures to clarify the controversy and to confirm some results of those previous studies.
2. Materials and Methods
With approval of the Ethics Committee at the Anesthesia and Pain Relief, Chishukai Taneyama Clinic (Shiojiri City, Nagano Prefecture, Japan), systolic BP and HR recorded before and 30 min after SGB were retrospectively analyzed for a total of 16,404 successful right SGBs performed on 848 subjects, and a total of 13,766 successful left SGBs performed on 792 subjects. Written informed consent for the block procedure was obtained from each patient, but no informed consent was obtained for the study as this study was a retrospective review of routine recording of systolic BP and HR stored in an electronic database. Recorded systolic BP and HR, and calculated changes of systolic BP (ΔSBP) and HR (ΔHR) were analyzed. Student paired t-test and unpaired t-test, and Chi-squared test were performed as appropriate for statistical analysis using Excel Statistical Program File ystat 2006xls.
All values were expressed as mean ± SD, and P < 0.05 was considered statistically significant.
Methods of stellate ganglion block were standardized as follows: Patients received a series of right or left SGBs, or right and left SGBs for various disorders, such as complex regional pain syndrome type 1, thoracic outlet syndrome, cervical spondylosis, tension headache, etc. Patients were placed on a table in the supine position in a procedure room with background music and a fragranceproducing unit, and the room temperature was kept constant at 23˚C. Systolic BP was measured from the contralateral upper arm with an automatic sphygmomanometer and the lead II electrocardiogram was monitored continuously.
After baseline systolic BP and HR measurements, a blind technique of SGB was performed by two anesthesiologist pain specialists with 6 ml of 1% mepivacaine using the anterior paratracheal approach at the level of C6. Evidence of Horner’s syndrome (ptosis, myosis and enophthalmos) on the ipsilateral side was considered a successful block, and systolic BP and HR were recorded 30 min after the procedure. There were no complications, such as seizures.
3. Results
There were no demographic differences in terms of age and gender between right and left SGB groups (age: 62.2 ± 14.8 versus 59.6 ± 15.4 years old; male/female: 336/512 versus 337/455).
Figures 1 and 2 show histograms of ΔSBP and ΔHR with right and left SGB, both of which appear normally distributed. Average systolic BP decreased significantly after both right and left SGBs (P < 0.0001 and P < 0.0001, respectively) (Table 1). The reduction of systolic BP (ΔSBP) was significantly greater with right SGB than with left SGB (P < 0.0001). HR decreased significantly with both right and left SGBs (P < 0.0001).
Tables 2 and 3 show percent (%) and numbers of SGBs corresponding to different ranges of ΔSBP and ΔHR. Incidence of moderate to marked reduction in sys-
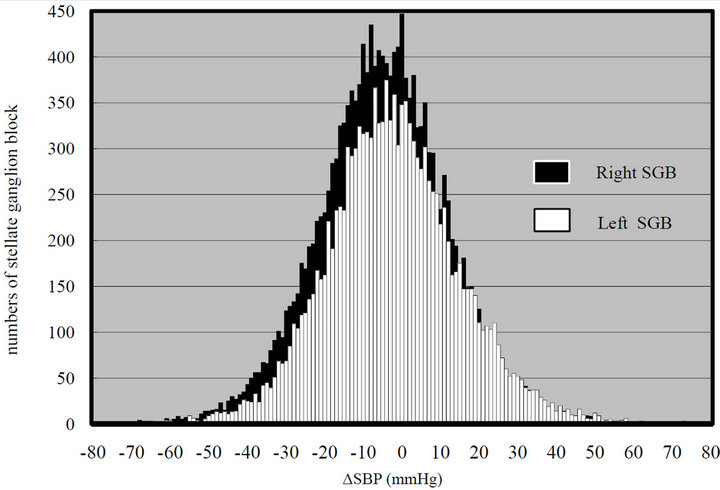
Figure 1. Histogram of Δ SBP with right stellate ganglion blocks (−4.8 ± 17.0 mmHg; mean ± SD) and with left stellate ganglion blocks (−2.2 ± 17.4 mmHg).

Figure 2. Histogram of Δ HR with right stellate ganglion blocks (−12.7 ± 9.4 beats/min; mean ± SD) and with left stellate ganglion blocks (−11.8 ± 8.7 beats/min).
tolic BP (ΔSBP; −25 to −49 and < −50 mmHg) were significantly higher with right SGB than with right SGB than with left SGB (P < 0.0001 and P < 0.05, respectively). On the other hand, left SGB produced a significantly higher incidence of moderate to marked increase in systolic BP (ΔSBP; +25 to +49 and < +50 mmHg) than did right SGB (P < 0.0001 and P < 0.0001, respectively) (Table 2). Incidence of marked reduction of HR (more than 30 beats/min) was significantly higher with right SGB than with left SGB (P < 0.0001) (Table 3).
4. Discussion
The main findings of the current study are: 1) Both right and left SGBs could produce significant hypotension or hypertension, and also marked bradycardia; 2) incidence of marked reduction in systolic BP was significantly higher with right SGB than with left SGB, and incidence of marked increase in systolic BP was significantly higher with left SGB than with right SGB; 3) incidence of
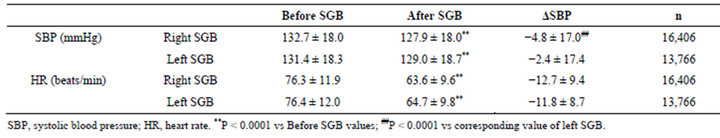
Table 1. SBP and HR before and after right or left SGB. Data represent mean ± SD.
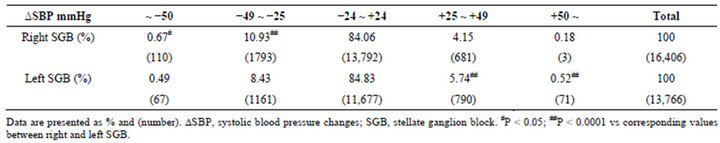
Table 2. Incidence of SBP changes after right or left SGB.
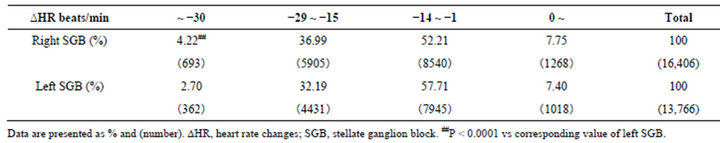
Table 3. Incidence of HR changes after right or left SGB.
marked reduction in HR was significantly higher with right SGB than with left SGB.
In our study, values of systolic BP and HR 30 min after SGB were compared to the baseline values, based on the following findings. It has been reported that Horner’s syndrome developed by 30 min after SGBs, and arterial baroreflex sensitivity and fractal cardiovascular dynamics were significantly attenuated at 30 min but not at 60 min after SGB [7]. Goh et al. [3] reported that heart rate became significantly decreased at 30 min after right SGB, and there was a maximal increase of skin temperature in the ipsilateral hands at 30 min after either side of SGBs. The blood flow of the optic nerve head was found to be increased at 30 min but not at 120 min after SGB [8].
To our knowledge, this was the first study in which different degrees of hypotension and hypertension, and also different degrees of HR changes were compared between right and left SGBs. In all other previous studies, overall average changes of BP and HR were compared between right and left SGBs, and this might be one reason, in addition to a small sample size, for conflicting results as to how right and left SGBs affect BP and HR differently.
The procedure room provided a stress-free atmosphere and a possible stress response to the block procedure, per se, should have been minimal, if any. The slight increases in heart rate in less than 8% of either right or left SGBs (Figure 2, Table 3) might be a reflection of the stress-free status during the procedures.
Successful SGB will decrease the sympathetic outflow from the stellate ganglions to the heart, exerting both negative inotropic action through ventricular innervation and negative chronotropic action to the sinus nodes. Therefore, it is conceivable that average systolic BP and average HR decreased after both right and left SGBs (Table 1). Furthermore, it was found that the reduction of average BP was significantly higher with right SGB than with left SGB (Table 1). The previous studies [3-5] did not show significant changes of average BP after either side of SGB, possibly due to small sample sizes in their studies. We focused further on clinically significant BP changes rather than average changes of BP, and found out that right SGB produced a higher incidence of significant hypotension compared to left SGB and left SGB produced a higher incidence of significant hypertension compared to right SGB. Unlike the previous studies [1-3], our study did not show a significant difference in significantly decreased average HR between right and left SGB (Table 1). However, incidence of marked bradycardia was higher with right SGB than with left SGB
(Table 3). As shown in the ΔHR histogram (Figure 2), most SGBs produced a reduction in HR. This may have been a reason why Rogers et al. [1] reported only HR changes after SGBs. We agree with their conclusion that the right stellate ganglion has a much greater chronotropic influence on the sinus node than does the left stellate ganglion. Animal studies show a similar finding: Sectioning the right inferior cardiac sympathetic nerve decreased HR by 30 to 50 beats/min, but sectioning the left cardiac sympathetic nerve slowed the HR less than 10 beats/min [9].
Kashima and colleagues [2] demonstrated the predominance of the right stellate ganglion in the sympathetic control of the human heart. Cardiac output was decreased significantly with right SGB but not with left SGB [10]. Moreover, our data showed that right SGB produced a higher incidence of not only marked reduction in HR but also moderate to severe reduction of systolic BP compared to left SGB (Tables 2 and 3). Thus, it is suggested that right stellate ganglions possess a predominant sympathetic influence on both the sinus node and the myocardium compared to the left stellate ganglions. Since cardiac sympathetic outflow is blocked by infiltrating local anesthetics to stellate ganglions, one would expect to observe a decrease but not an increase in systolic BP. However, blood pressure was increased in a fair number of right SGBs and left SGBs. This is clearly shown in the ΔSBP histogram (Figure 1) in which Δ systolic BP for both right and left SGBs appears normally distributed with their mean values close to zero.
Because solution injected around the stellate ganglions spreads to surrounding areas [11], adjacently located vagal afferents such as the aortic depressor nerve could have been blocked with SGB. Diminished aortic depressor nerve discharge can trigger arterial baroreflex, leading to increased sympathetic outflow with resultant increased peripheral vascular resistance, myocardial contractility and systolic BP. Ikeda and colleagues [12] observed increased tibial nerve muscle sympathetic activity after left SGB and postulated that not only vagal afferents from the aortic arch but also afferent impulses from the carotid sinus and vagal afferents from cardiopulmonary baroreceptors may have been blocked.
Another question arises: Why did left SGB produce a significantly higher incidence of moderate to severe increase in systolic BP compared to right SGB (Table 2). Kimura and colleagues [6] reported seven cases of severe hypertension (systolic BP > 200 mmHg) after SGB, with an estimated occurrence rate of 1/2000 - 1/3000. It is interesting to note that 6 cases were after left SGB and only one case was after right SGB. Therefore, there may be mechanisms by which left SGB causes a higher incidence of severe hypertension. Several studies suggest hemispheric lateralization of autonomic cardiovascular control in which the parasympathetic nervous system dominates the left homolateral half [13-15]. Thus, even a partially blocked afferent impulse from the left vagal afferents may be strong enough to trigger a significant high pressure baroreflex, resulting in a higher incidence of severe hypertension with left SGB than with right SGB. Although there was a lower incidence than with left SGB, there were cases of moderate to marked increase in systolic BP with right SGB (Table 2). One reason, in addition to individual variations, may be due to ultradian rhythms in which sympathetic and parasympathetic nervous activity switch dominance on the two sides from time to time [16].
The limitations of this study are as follows: Our data were obtained from successful SGBs performed in 2002- 2006, and a blind technique was used in our study as other previous studies in which the effects of right and left SGB on blood pressure and heart rate were studied. Recently, ultrasound-guided SGB has gained popularity and the total amount of local anesthetics for SGB can be reduced. Therefore, our results could be different if the ultrasound-guided SGB technique had been used. Thus, it would be interesting to study the effects of ultrasoundguided right and left SGBs on blood pressure and heart rate in the future.
Our study was not a prospective study, and SGBs with saline were not performed to obtain control values. A majority of patients received right or left SGB but not both sides of SGB for comparison. It was not taken into consideration how each patient responded differently to each successful SGB during multiple SGB procedures. However, it was necessary to use repeated data from the same patients in order to find the incidence of clinically significant changes of BP and HR and to compare different degrees of BP and HR changes between right and left SGBs. We could not examine whether or not there were any differences in cardiopulmonary conditions, medical disorders, medications and so forth between right and left SGB groups. However, the large patient population, as well as normally distributed systolic BP and HR changes should warrant comparison of those parameters between right and left SGB groups.
In summary, clinicians should be aware that both right and left SGB could produce severe hypotension and hypertension, and also marked bradycardia. However, clinicians also should be aware that right SGB causes a higher incidence of severe hypotension than does left SGB. On the other hand, left SGB causes a higher incidence of significantly increased BP than does right SGB. Reduction in HR is a common response to both right and left SGBs, but right SGB causes a higher incidence of a significant reduction in HR than does left SGB.
REFERENCES
- M. C. Rogers, G. Battit, B. McPeek and D. Todd, “Lateralization of Sympathetic Control of the Human Sinus Node: ECG Changes of Stellate Ganglion Block,” Anesthesiology, Vol. 48, No. 2, 1978, pp. 139-141. doi:10.1097/00000542-197802000-00009
- T. Kashima, H. Tanaka, S. Minagoe and H. Toda, “Electrocardiographic Changes Induced by the Stellate Ganglion Block in Normal Subjects,” Journal of Electrocardiology, Vol. 14, No. 2, 1981, pp. 169-174. doi:10.1016/S0022-0736(81)80052-0
- J. S. Goh, B. W. Min and H. D. Kim, “Blood Pressure, Pulse Rate and Temperature Changes of the Ipsilateral Upper Extremity after Unilateral Stellate Ganglion Block,” Journal of Korean Pain Society, Vol. 3, No. 1, 1990, pp. 27-33.
- M. J. Gardner, S. Kimber, D. E. Johnstone, R. C. Shukla, B. M. Horacek, C. Forbes and J. A. Armour, “The Effects of Unilateral Stellate Ganglion Blockade on Human Cardiac Function during Rest and Exercise,” Journal of Cardiovasc Electrophysiology, Vol. 4, No. 1, 1993, pp. 2-4. doi:10.1111/j.1540-8167.1993.tb01207.x
- E. B. Lobato, K. B. Kern, G. B. Paige, M. Brown and C. A. Sulek, “Differential Effects of Right versus Left Stellate Ganglion Block on Left Ventricular Function in Humans: An Echocardiographic Analysis,” Journal of Clinical Anesthesia, Vol. 12, No. 4, 2000, pp. 315-318. doi:10.1016/S0952-8180(00)00158-6
- T. Kimura, K. Nishiwaki, S. Yokota, T. Komatsu and Y. Shimada, “Severe Hypertension after Stellate Ganglion Block,” British Journal of Anaesthesia, Vol. 94, No. 6, 2005, pp. 840-842. doi:10.1093/bja/aei134
- C. Taneyama and H. Goto, “Fractal Cardiovascular Dynamics and Baroreflex Sensitivity after Stellate Ganglion Block,” Anesthesia & Analgesia, Vol. 109, No. 4, 2009, pp. 1335-1340. doi:10.1213/ane.0b013e3181b018d8
- H. G. Yu, H. Chung, K. W. Yoon and H. J. Kim, “Stellate Ganglion Block Increases Blood Flow into the Optic Nerve Head and the Peripapillary Retina in Human,” Autonomic Neuroscience, Vol. 109, No. 1-2, 2003, pp. 53-57. doi:10.1016/j.autneu.2003.08.010
- T. Kawada, K. Uemura, K. Kashihara, Y. Jin, M. Li, C. Zheng, M. Sugimachi and K. Sunagawa, “Uniformity in Dynamic Baroreflex Regulation of Left and Right Cardiac Sympathetic Nerve Activities,” American Journal of Physiology. Regulatory, Integrative and Comparative Physiology, Vol. 284, No. 6, 2003, pp. R1506-R1512.
- K. Yokoyama and K. Sugiyama, “Hemodynamic Effects of Stellate Ganglion Block: Analysis Using a Model of Aortic Input Impedance,” Canadian Journal of Anesthesia, Vol. 49, No. 8, 2002, pp. 887-888. doi:10.1007/BF03017432
- M. Guntumukkala and P. A. Hardy, “Spread of Injectate after Stellate Ganglion Block in Man: An Anatomical Study,” British Journal of Anaesthesia, Vol. 66, No. 6, 1991, pp. 643-644. doi:10.1093/bja/66.6.643
- T. Ikeda, S. Iwase, Y. Sugiyama, T. Matsukawa, T. Mano, M. Doi, M. Kikura and K. Ikeda, “Stellate Ganglion Block Is Associated with Increased Tibial Nerve Muscle Sympathetic Activity in Humans,” Anesthesiology, Vol. 84, No. 4, 1996, pp. 843-850. doi:10.1097/00000542-199604000-00011
- M. J. Hilz, M. Dutsch, K. Perrine, P. K. Nelson, U. Rauhut and O. Devinsky, “Hemispheric Influence on Autonomic Modulation and Baroreflex Sensitivity,” Annals of Neurology, Vol. 49, No. 5, 2001, pp. 575-578. doi:10.1002/ana.1006
- W. Wittling, A. Block, S. Genzel and E. Schweiger, “Hemispheric Asymmetry in Parasympathetic Control of the Heart,” Neuropsychologia, Vol. 36, No. 5, 1998, pp. 461- 468. doi:10.1016/S0028-3932(97)00129-2
- B. W. Yoon, C. A. Morillo, D. F. Cechetto and V. Hachinski, “Cerebral Hemispheric Lateralization in Cardiac Autonomic Control,” Archives of Neurology, Vol. 54, No. 6, 1997, pp. 741-744. doi:10.1001/archneur.1997.00550180055012
- D. S. Shannahoff-Khalsa, “Selective Unilateral Autonomic Activation: Implications for Psychiatry,” CNS Spectrums, Vol. 12, No. 8, 1997, pp. 625-634.
NOTES
*Corresponding author.

