Open Journal of Psychiatry
Vol.3 No.3(2013), Article ID:33673,10 pages DOI:10.4236/ojpsych.2013.33030
Antenatal anxiety in the first trimester: Risk factors and effects on anxiety and depression in the third trimester and 6-week postpartum*
![]()
1Department of Psychiatry, LKS Faculty of Medicine, The University of Hong Kong, Hong Kong, China
2Department of Obstetrics and Gynaecology, LKS Faculty of Medicine, The University of Hong Kong, Hong Kong, China
3Department of Obstetrics and Gynaecology, Queen Mary Hospital, Hong Kong, China
4Department of Obstetrics and Gynaecology, Queen Elizabeth Hospital, Hong Kong, China
5Department of Psychology, National University of Singapore, Singapore City, Singapore
Email: #1ayuchan@gmail.com
Copyright © 2013 Chui Yi Chan et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received 2 May 2013; revised 3 June 2013; accepted 10 June 2013
Keywords: Pregnancy; Antenatal Anxiety; Postpartum Anxiety and Depression
ABSTRACT
Objective: Anxiety is common among pregnant women. However, research attention in the area of reproductive mental health has mainly focused on postpartum depression in past decades. Given adverse outcomes of antenatal anxiety, there is an urgent need to fill the research gaps. The objectives of the present study were to determine the prevalence of antenatal anxiety symptoms and examine the risk factors and effects of anxiety symptoms in early pregnancy on anxiety and depressive symptoms in later pregnancy and early postpartum period. Methodology: A prospective longitudinal design with quantitative approach was adopted. A consecutive sample of 1470 Chinese pregnant women from hospitals in Hong Kong was invited to participate in the study and was assessed using standardized instruments on 3 time points including first and third trimesters of pregnancy and 6-week postpartum. Results: The results showed that 17.7% of pregnant women manifested anxiety symptoms in the first trimester of pregnancy. Single mothers, younger mothers, mothers who smoked before pregnancy and mothers who received low education level reported significantly higher levels of anxiety symptoms in the first trimester. Unwanted pregnancy, low self esteem, low marital satisfaction and perceived low social support were significant psychosocial risk factors for anxiety symptoms in the first trimester. Anxiety symptoms in the first trimester were independent predictors for anxiety symptoms in the third trimester (β = 0.26, t = 5.74, p < 0.001), however anxiety symptoms in the first trimester no longer significantly predicted anxiety and depressive symptoms in 6 weeks postpartum after adjusting for the effects of potential confounders. Discussions: The present study points to the need for greater research and clinical attention to antenatal anxiety given that antenatal anxiety is a prevalent problem and has serious impacts on maternal wellbeing. Such findings also contribute to the understanding of maternal anxiety and have implications for the design of effective identification, prevention and treatment of these significant clinical problems
1. INTRODUCTION
The transition to motherhood is a period of developmental challenge involving substantial changes and adjustments, both physiologically and psychologically. Pregnancy is thus a potential stressor and a high-risk period during which women with psychological vulnerability may develop mental health problems. Although mild symptoms of stress and anxiety in response to this challenge and stressor are expected, a significant proportion of pregnant women manifest symptoms of anxiety which may progress and develop into clinical anxiety disorders.
Indeed, anxiety disorders are common among women of child bearing age [1]. A study [2] assessed women during pregnancy and found 21% of pregnant women met DSM-IV diagnostic criteria for at least one anxiety disorders; another study [3] reported that the prevalence of state and trait anxiety symptoms was 59.5% and 45.3% respectively among pregnant women. Although antenatal anxiety is prevalent during pregnancy and a recent study [4] reported that antenatal anxiety symptoms were more prevalent than antenatal depressive symptoms, research attention in the area of reproductive mental health has mainly focused on postpartum depression. Even studies on antenatal psychiatric disorders are mainly on antenatal depression. Much less attention has been given to anxiety symptoms among pregnant and postpartum women.
Anxiety during pregnancy is found to be associated with a variety of adverse consequences in term of pregnancy outcomes and obstetrics complications such as somatic complaints [5], gestational and obstetric complications [6], alterations in fetal motor activity [7], and affected fetal heart rate patterns [7]. Regarding the effets on development of the offspring, antental anxiety symptoms significantly predict difficult temperament at 4 and 6 months among infants [8] and a delay in mental development among two-year-old children [9]. Thus, given the health implications of antenatal anxiety, there is an urgent need to refocus research efforts on antenatal anxiety.
Although antenatal anxiety has been identified as a predictor of postpartum depression and postpartum anxiety [2,10], little is known about if anxiety in early pregnancy can significantly predict anxiety and depression in later pregnancy and early postpartum period. Besides, in order to develop effective prevention and early intervention strategites, it is of value for examining how the effects of various demographic and psychosocial risk factors on anxiety in early pregnancy.
To fill the above-mentioned gaps and facilitate further research in this area and clinical practices and approaches to the prevention and treatment of anxiety in pregnancy and postpartum period, our study aimed at estimating the prevalence of antental anxiety symptoms in the first trimester and identifying its demographgic and psychosocial risk factors. We further examined whether antental anxiety symptoms in the first trimester could significantly predict antental anxiety symptoms in the third trimester, anxiety and depressive symptoms in 6 weeks postpartum.
2. METHOD
2.1. Participants and Procedures
Ethics approval was obtained from the Institutional Review Boards of the University of Hong Kong/Hospital Authority Hong Kong West Cluster and Hospital Authority Hong Kong Kowloon West Cluster. Informed written consent was obtained from all participants before the study. A consecutive sample of 1470 Chinese pregnant women at first presentation in the antenatal clinic of two regional hospitals in Hong Kong was invited to participate in the study. Eligible women included all pregnant women of Chinese ethnicity above 18 years of age. Women considering termination of pregnancy, having conceived through in-vitro fertilization or having significant medical diseases were excluded.
A prospective longitudinal design was used in present study. Participating women were assessed a total of 3 times. They were first assessed in the first trimester and re-assessed in the third trimester and 6 weeks postpartum. Antenatal questionnaires were administrated at the antenatal clinic whereas postpartum questionnaires were mailed to participants.
2.2. Instruments
Demographic and psychosocial risk factors such as self esteem, perceived social support and marital satisfaction and anxiety and depressive symptoms were assessed at the first trimester (12 weeks of gestation), at the third trimester (36 weeks of gestation) and at 6 weeks postpartum.
Antenatal and postpartum anxiety symptoms were assessed by the Anxiety Subscale of the Hospital Anxiety and Depression Scale (HADS-A) [11]. The HADS-A consists of seven items to assess presence or absence of anxiety symptoms over the past week and responses are rated on a four-point (0 - 3) response category. It was specifically developed to measure general anxiety states focusing on affective symptoms, and was designed to include minimal reference to somatic symptoms [12] such as insomnia and fatigue. As many somatic symptoms are common experiences in perinatal populations, the HADS-A is superior to other measures of anxiety symptoms because it is a relatively pure measure for reflecting psychological disturbances among pregnant women. The validated Chinese version of the HADS-A was used [13]. The recommended cutoff of 7/8 was used to identify probable cases of clinically significant anxiety [11]. The HADS-A has been validated among pregnant women with a sensitivity and specificity of 93% and 90% respectively. Cronbach’s reliability coefficients were found to vary from 0.71 to 0.81 [14].
The Edinburgh Postnatal Depression Scale (EPDS) [15] was used to assess antenatal and postpartum depressive symptoms. The EPDS focuses on the cognitive and affective features of depression rather than on somatic symptoms. It consists of ten items and responses are rated on a four-point (0 - 3) response category. Although the EPDS was originally developed to measure postpartum depression [15], it has also been validated for assessing antenatal depression, with sensitivity and specificity in identifying antenatal depression being 64% and 90% respectively [16]. The EPDS has been widely used to measure antenatal depression in recent studies [17]. The Chinese version was validated among pregnant women in Hong Kong with good psychometric properties [18].
The 10-item Rosenberg Self Esteem Scale (RSES) [19] was used to assess pregnant women’s global feelings of self-worth or self acceptance. The scale consists of 10 items. Responses are rated on a four point ranging from “strongly disagree” to “strongly agree”. The scale has high reliability with test-retest correlation ranging from 0.82 to 0.88, and Cronbach’s reliability coefficients ranging from 0.77 to 0.88 [20].
The validated Chinese version of the Kansas Marital Satisfaction Scale (CKMS) [21,22] was used to assess marital satisfaction. It is a widely used three-item scale to measure women’s satisfaction with their spouse, their marriage, and their relationship with their spouse on a 7 point scale [23]. The KMSS demonstrates good internal consistency and reliability [23].
The validated Chinese version of Medical Outcomes Study Social Support Survey (MOS-SSS-C) [24] was used to assess self-perceived adequacy of social support. It consists of 20 items. Responses are rated on a fivepoint (1 - 5) scale. The criterion validity and construct validity of the MOS-SSS-C is supported. Cronbach’s alpha for the scale is 0.98 [24].
Participants were asked to indicate whether the pregnancy was planned (yes/no) and whether the pregnancy was wanted (yes/no) in the first trimester in order to assess their attitudes toward pregnancy.
Information on demographic variable were sought in the first trimester, including age, parity, marital status, educational background, monthly family income, past and current smoking behavior, past and current alcohol use.
2.3. Statistical Analysis
The overall level of significance was taken as 5% and all estimates were accompanied by 95% confidence intervals. Descriptive statistics were presented by means and standard deviations for continuous variables and percentages for categorical variables. Attrition analyses comparing those who participated in all time points of the study and those who dropped out of the study were performed with Fisher exact test for categorical variables, t tests for continuous variables.
Demographic risk factors for antenatal anxiety symptoms at the first trimester were assessed using independent sample t-test and one way ANOVAs. Psychosocial risk factors for antenatal anxiety symptoms at the first trimester were examined in two phases. In the first phase, the univariable relationship between antenatal anxiety symptoms at the first trimester and each of the psychosocial risk factor were examined using univariable linear regressions. In the second phase, a series of hierarchical multiple regression analyses were conducted in order to test whether psychosocial risk factors could provide additional predictive power of general anxiety symptoms after controlling for the effects of identified demographic risk factors. Thus, those demographic factors which were identified to be significant in the previous analyses were force-entered in the first block, and significant psychosocial risk factors which were identified in the first phase were entered in the second block using the forward stepwise procedure.
Similar analyses were performed to examine if antenatal anxiety symptoms in the first trimester could significantly predict antenatal anxiety symptoms in the third trimester, and postpartum anxiety and depressive symptoms. In the first phase, the univariable linear regressions were used. A series of hierarchical multiple regression analyses was then conducted to examine if antenatal anxiety symptoms at the first trimester could significantly predict anxiety symptoms at the third trimester, and postpartum anxiety and depressive symptoms after adjusting for the effects of identified demographic and psychosocial risk factors, and other forms of mental health problems (anxiety/depressive symptoms) in respective trimesters and postpartum period.
All Statistical analyses were performed with SPSS 19.0 (SPSS Inc., Chicago IL).
3. RESULTS
A total of 1647 pregnant women were invited to participate in the study. Out of these, 1470 pregnant women agreed and returned the completed questionnaire in the first trimester, yielding a response rate of 89.25%. Of these, 722 pregnant women returned completed questionnaires at the third trimester, yielding an attrition rate of 50.88%. A total of 298 (overall attrition rate: 79.73%) pregnant women completed postpartum questionnaires at 6 weeks postpartum.
The differences on demographic characteristics, psychological characteristics, anxiety symptoms and depressive symptoms at baseline (T1) between those who participated in all the antenatal assessments and those who dropped out before childbirth were tested using Chisquare and independent sample t-tests (Table 1). Four significant differences were noted. The two significant differences between the groups were age (c2(2) = 15.56, p < 0.01), educational level (c2(2) = 16.54, p < 0.01), family income (c2(2) = 19.34, p < 0.01), and planned pregnancy (c2(1) =4.01, p < 0.05). Women who did not complete all antenatal assessments were older (≥35),
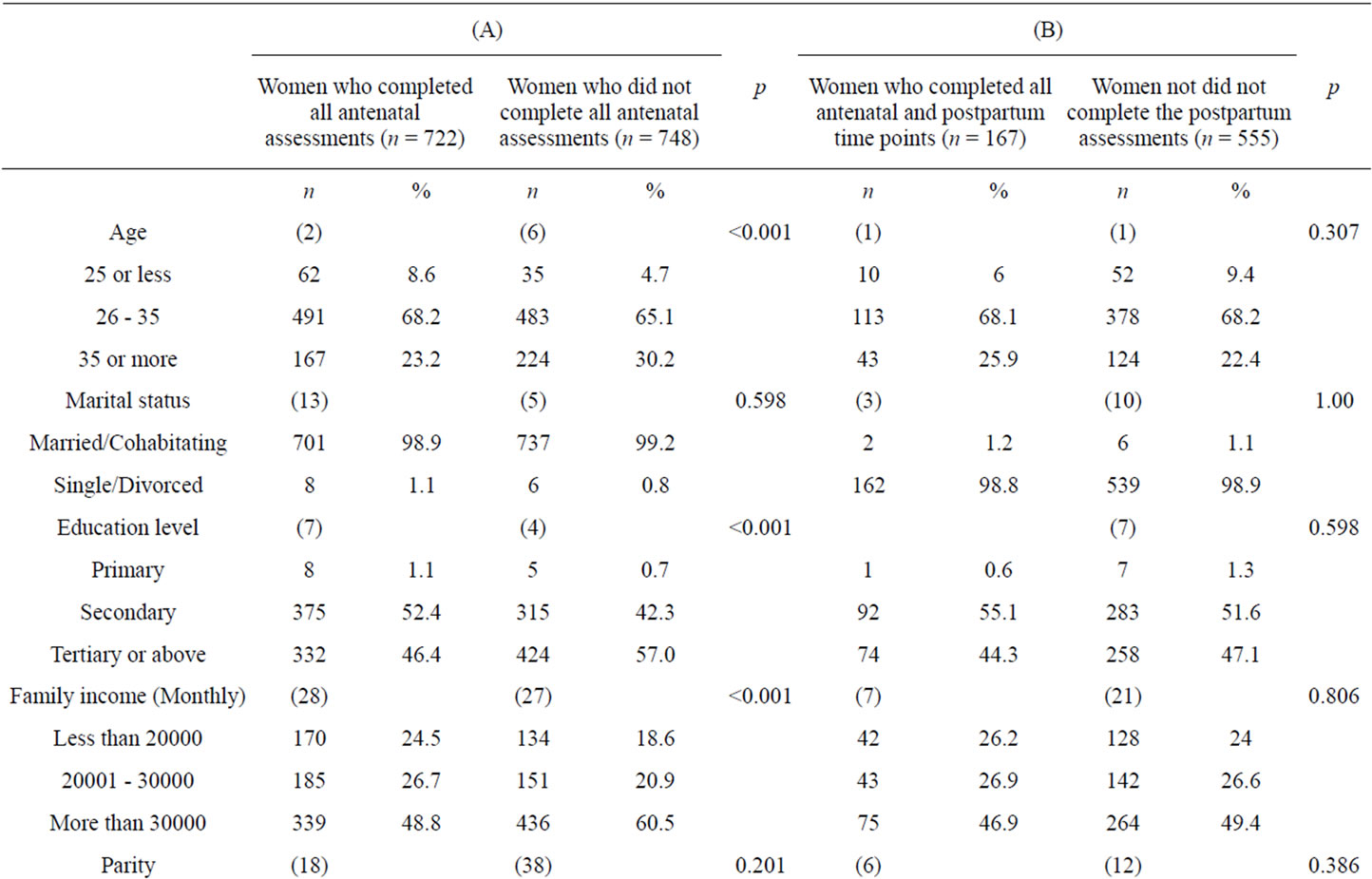
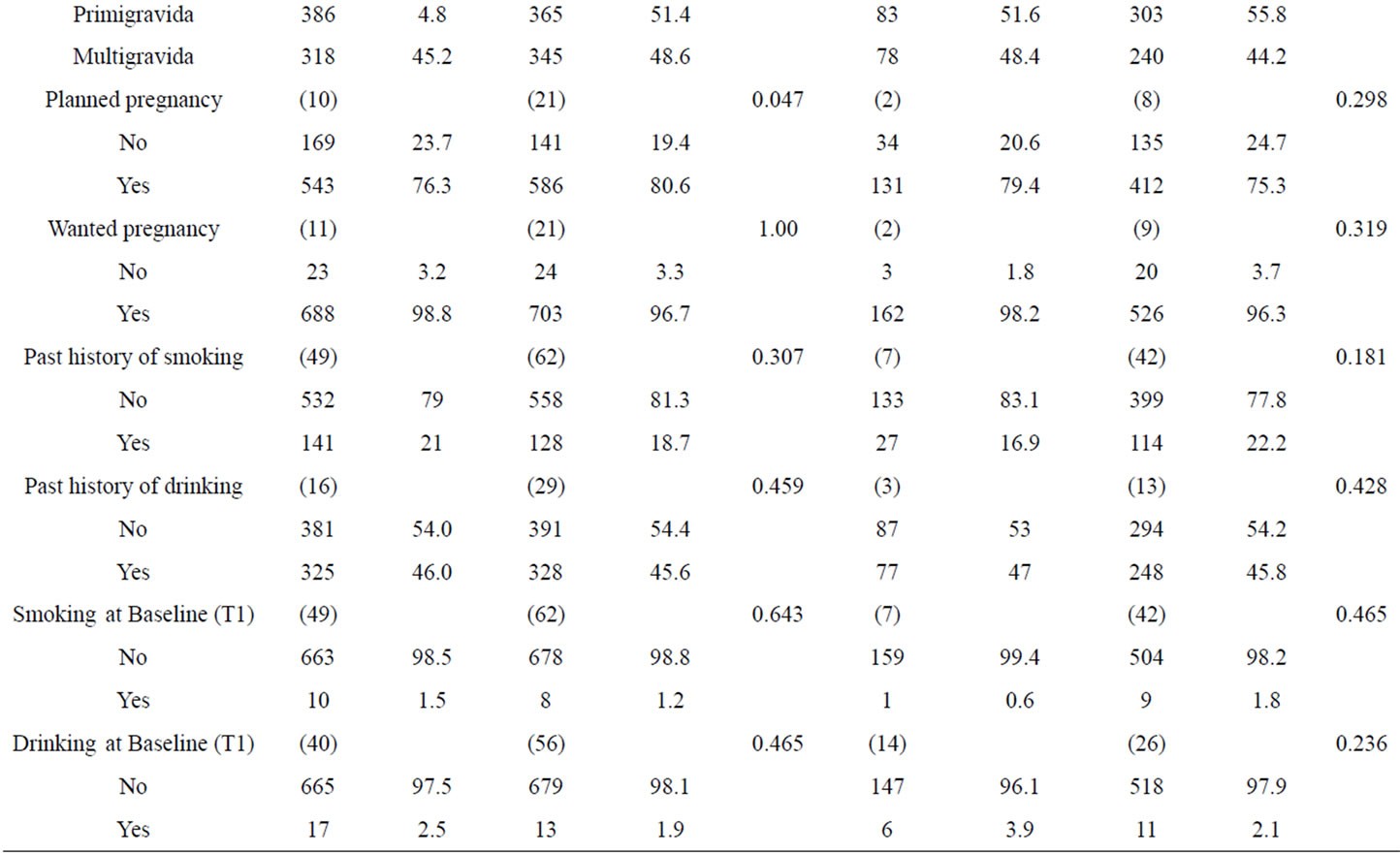
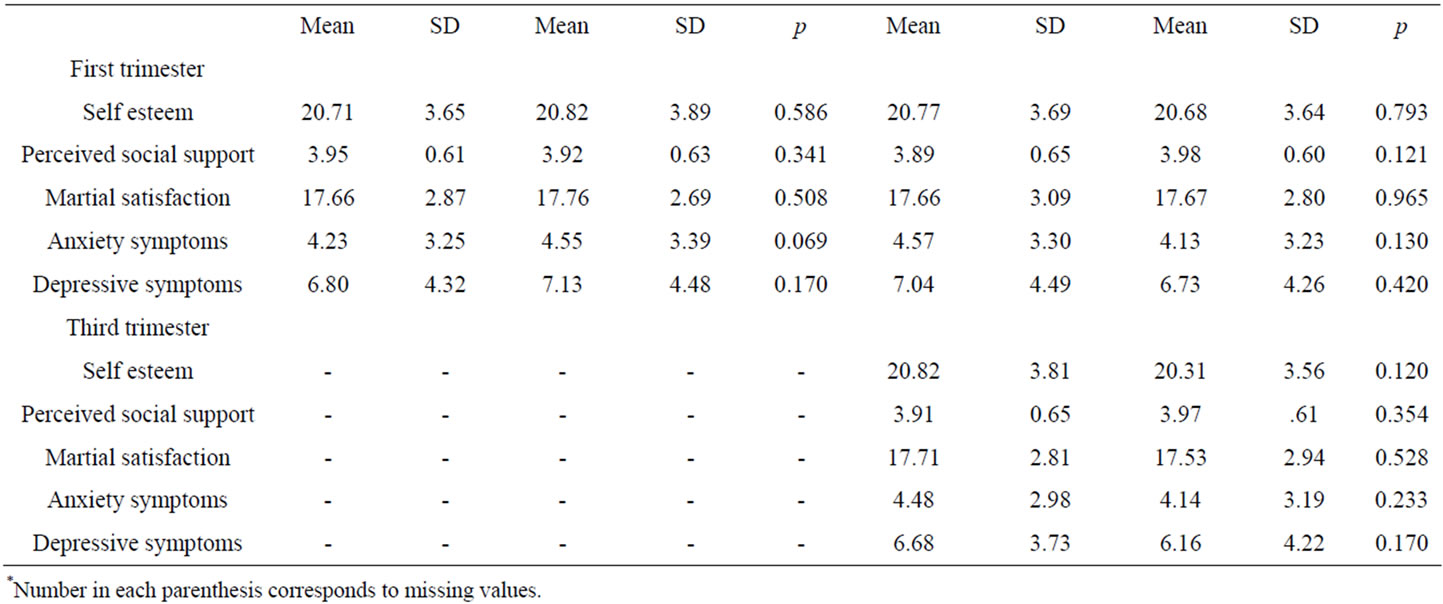
Table 1. Sample characteristics of women at first trimester with comparison between (A) Sample characteristics of women at first trimester who completed all the antenatal assessments and women who did not complete all the antenatal assessments and between (B) women who completed all antenatal and postpartum assessments and women who did not complete the postpartum assessment.
received higher education, had higher family income and were more likely to have planned their pregnancy than women who completed all antenatal assessments. The two groups did not differ on other demographic characteristics at the first trimester (baseline), psychosocial characteristics at the first trimester, and they did not differ on mean anxiety and depression score at the first trimester. Those who participated in all three time points and those who dropped out after child birth did not differ on all demographic characteristics in the first trimester (baseline) or psychosocial characteristics in the first and third trimester (Table 1). The two groups were also not significantly different on mean anxiety and depression scores in the first and third trimester.
All participants were of Chinese ethnicity and born in Hong Kong. The mean age of the participants was 31.98 years (Standard Deviation [SD]: 4.12, range: 18 - 45 years). Almost all of the women (98.2%) were either married or cohabiting. Around half of participants (53.1%) were primiparous. 98.7% of pregnant women has attained at least a secondary level of education. Almost half of the participants (54.8%) had a family monthly more than $30,000 (Hong Kong dollars, which amount to approximately 3046 US dollars). The majority (78.5%) had planned for the pregnancy. Whether or not the pregnancy was planned, 96.7% of the pregnancies were wanted. 19.8% and 1.3% of participants smoked before pregnancy and during the first trimester respectively. 9% and 3% of participants smoked during the third trimester and 6 weeks postpartum respectively. 45.8% of the participants had the habit of drinking before pregnancy but only 1.1% and 1% of participants drank during the first and third trimester respectively. The rates of drinking increased after delivery. 10% of participants reported drinking during 6 weeks postpartum.
Using the validated cut-off scores of 7/8 for the Anxiety Subscale of Hospital Anxiety and Depression Scales (HADS-A) for probable cases of anxiety [11], the prevalence of anxiety was 17.7% (95% CI: 15.8% to 19.9%) and 16.2% (95% CI: 13.56% to 19.22%) in the first and third trimester respectively. The prevalence of general anxiety symptoms in the third trimester was significantly higher than in 6 weeks postpartum (χ2(1) = 21.18, p < 0.001). The rate was 14.7% (95% CI: 10.94% to 19.52%) in 6 weeks postpartum. The HADS-A mean scores of the participants in the first trimester, third trimester and 6 weeks postpartum respectively: 4.39 (SD 3.32), 4.22 (SD 3.14), and 3.76 (SD 3.29).
Using the locally validated cut-off scores of 9/10 for probable cases of depression [18], the prevalence of depression was 25.4% (95% CI: 23.09% to 27.71%), 20.9% (95% CI: 17.83% to 23.97%) and 15.8% (95% CI: 11.56% to 20.04%) in the first trimester, third trimester and 6 weeks postpartum period respectively. The mean scores of the Edinburgh Postnatal Depression Scale [15] (EPDS) were 6.97 (SD: 4.40), 6.28 (SD: 4.12) and 5.67 (SD: 4.05) in the first trimester, third trimester and 6 weeks postpartum respectively.
The results of independent sample t-test, one way ANOVAs and univariable linear regression analyses examining the relationship between each of maternal demographic factors and anxiety symptoms at the first trimester were presented in Table 2. Pregnant women who were single mothers (t(1357) = 2.55, p < 0.05), and who smoked before pregnancy (t(1284) = 4.05, p < 0.05) were more likely to have higher level of anxiety symptoms. Although the results of one way ANOVAs did not show any significant effects of age groups (F(2, 1365) = 2.65, p = 0.071) and educational levels (F(3, 1363) = 2.48, p = 0.059) on anxiety levels, post hoc comparison
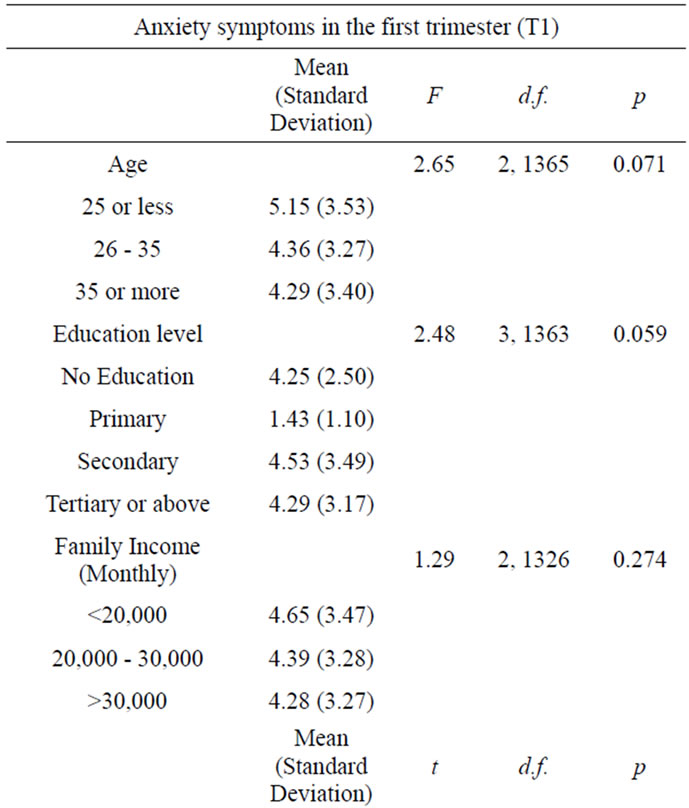
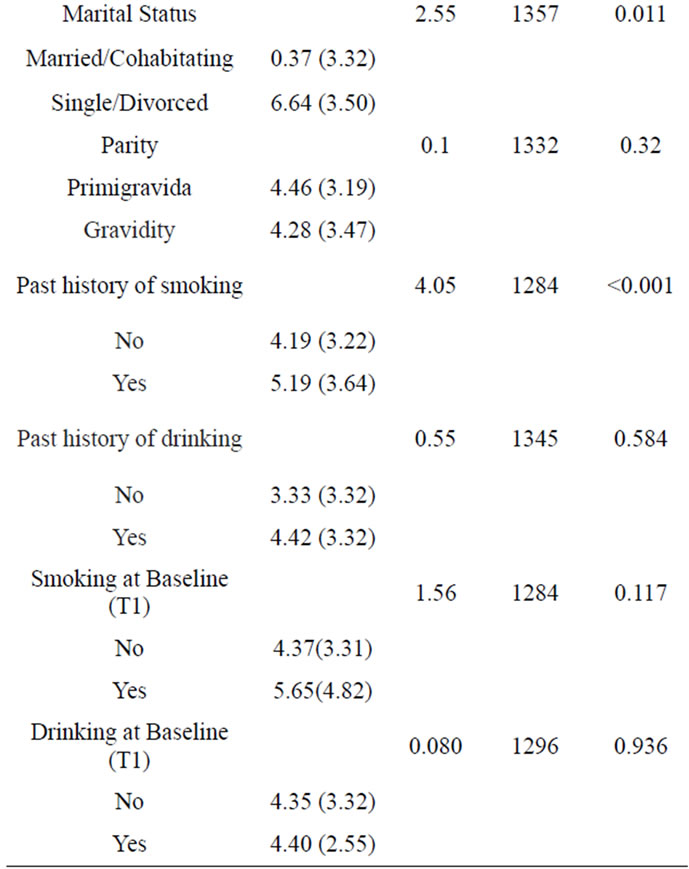
Table 2. Demographic risk factors for anxiety symptoms in the first trimester.
using the Least significant difference (LSD) test indicated that pregnant women who were young age (p < 0.05) and who received low education level (p < 0.05) reported significantly higher levels of anxiety symptoms.
Regarding psychosocial risk factors, the results of independent sample t-test and univariable linear regression analyses showed that women with unplanned pregnancy (t(1368) = 5.84, p < 0.001), with unwanted pregnancy (t(1369) = 4.01, p < 0.001), with low self esteem (β = −0.36, t = −13.21, p < 0.001), with low perceived social support (β = −0.33, t = −12.13, p < 0.001) and with low marital satisfaction (β = −0.25, t = −9.3, p < 0.001) were more likely to have higher level of anxiety symptoms in the first trimester.
When a forward stepwise hierarchical multiple regression was applied to the psychosocial factors in the first trimester (Table 3), unwanted pregnancy (β = 0.10, t = 3.41, p < 0.01), low self esteem (β = −0.26, t = −8.19, p < 0.01), low marital satisfaction (β = −0.08, t = −2.61, p < 0.01) and perceived low social support (β = −0.22, t = −6.67, p < 0.01) were significantly and independently associated with higher levels of general anxiety symptoms in the first trimester. The psychosocial risk factors including unplanned pregnancy, unwanted pregnancy, low self esteem, low marital satisfaction and perceived low social support explained a significant proportion of variance in general anxiety symptoms in the first trimester (R2 = 0.22, F(8, 1041) = 36.67, p < 0.001).
The results of univariable linear regression analyses examining the association of anxiety symptoms in the first trimester with anxiety and depressive symptoms in the third trimester and 6 weeks postpartum (Table 4). Anxiety symptoms in the first trimester significantly predicted anxiety (β = 0.55, t = 16.91, p < 0.001) and depressive symptoms (β = 0.49, t = 14.08, p < 0.001) in the third trimester; and also significantly predicted anxiety (β = 0.49, t = 9.41, p < 0.001) and depressive symptoms (β = 0.43, t = 7.95, p < 0.001) in 6 weeks postpartum.
Two hierarchical multiple regression analyses (Table 5) were conducted in order to examine if anxiety symptoms in the first trimester could significantly predict anxiety and depressive symptoms in the third trimester after adjusting for the effects of identified demographic and psychosocial risk factors, depressive symptoms in the first trimester and other forms of mental health problems (anxiety/depressive symptoms) in the third trimester. Result showed anxiety symptoms in the first trimester still significantly predicted anxiety symptoms in the third trimester (β = 0.26, t = 5.74, p < 0.001). However, anxiety symptoms in the first trimester no longer significantly predict depressive symptoms in the third trimester after adjusting for the effects of potential confounders.
Similar hierarchal multiple regression analyses (Table 6) were conducted for postpartum anxiety and depressive symptoms. After adjusting for identified demographic and psychosocial risk factors, depressive symptoms in the first trimester, and other forms of mental health prob-
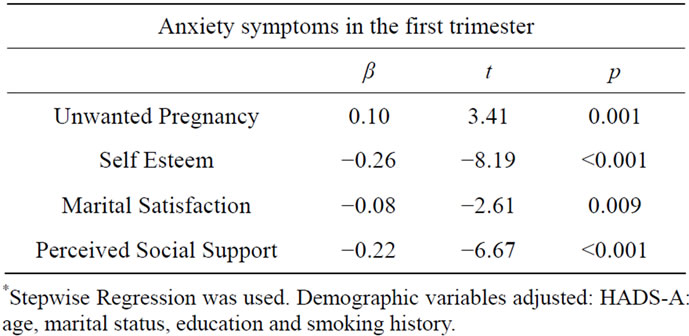
Table 3. Psychosocial characteristics associated with anxiety symptoms in the first trimester after controlling for demographic risk factors*.
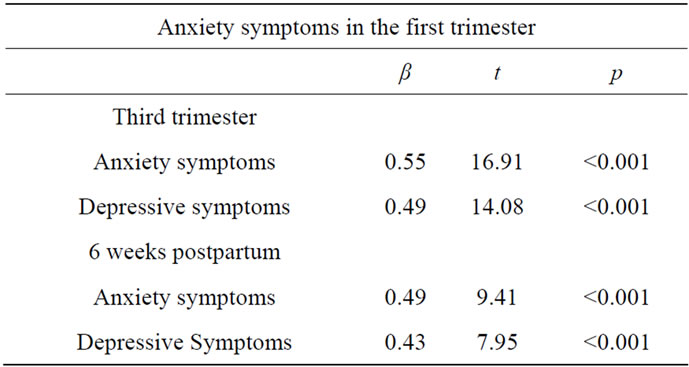
Table 4. Univariate regression analysis of anxiety symptoms in the first trimester for predicting anxiety and depressive symptoms in the third trimester and in the 6 weeks postpartum.

Table 5. Hierarchical multiple regression analysis of anxiety symptoms in the first trimester for predicting anxiety and depressive symptoms in the third trimester adjusting for the effects of potential confounders.
lems (anxiety/depressive symptoms) in the 6 weeks postpartum, anxiety symptoms in the first trimester were no longer significant predictors for postpartum depressive symptoms but were still significant predictors for postpartum anxiety symptoms (β = 0.24, t = 4.31, p < 0.001). However, after adding anxiety and depressive symptoms in the third trimester as covariate in the hierarchical multiple regression model, anxiety symptoms in the first trimester were no longer significant predictors for postpartum anxiety symptoms.
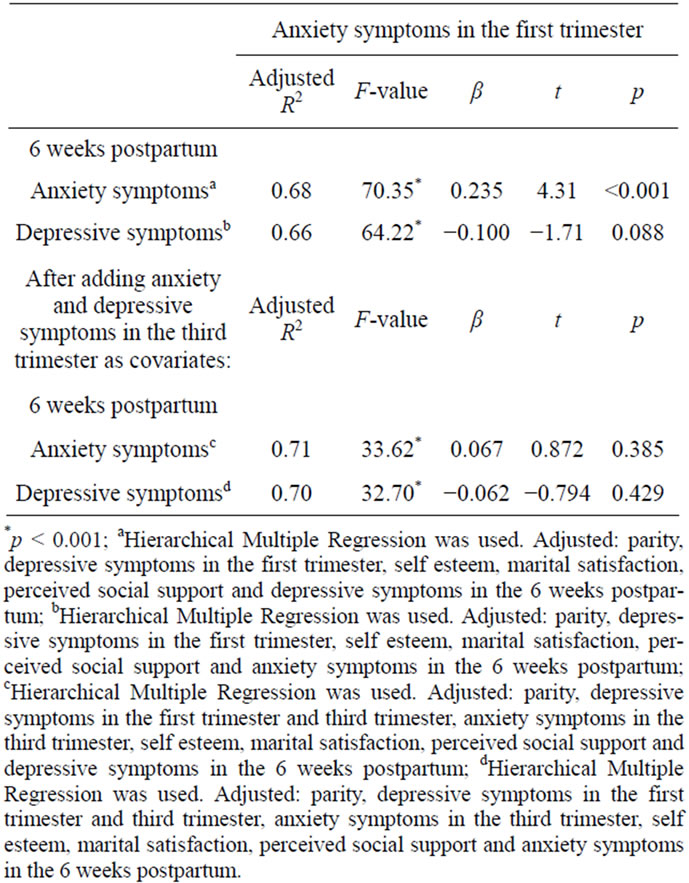
Table 6. Hierarchical multiple regression analysis of anxiety symptoms in the first trimester for predicting anxiety and depressive symptoms in the 6 weeks postpartum adjusting for the effects of potential confounders.
4. DISCUSSIONS
A lot of research attention is focused on postpartum depression. Relatively little attention has been paid to antenatal mental health problems specifically antenatal anxiety. Our study, however, showed that antenatal anxiety is more prevalent than postpartum depression. The prevalence of anxiety using the HADS-A, at a suggested cutoff of 7/8, was found to be 17.7% and 16.2% in the first and third trimester respectively and the prevalence of postpartum depression, at a recommended cutoff of 9/10, was found to be 15.8%. In addition, the prevalence for antenatal anxiety which was found in present study was consistent and similar to that reported in western studies. A study [25] used a cutoff 44/45 of the State Anxiety Inventory (STAI-S) and found that the prevalence of anxiety was 15.0% and 18.2% in the first and third trimester respectively. The present finding highlights the need for greater research and clinical attention to be paid to antenatal anxiety, given the adverse outcome of antenatal anxiety on maternal well-being and fetal development [5,7]. Anxiety was found to be less common in the postpartum period than during pregnancy [26]. Indeed, the prevalence was found to be 14.7%. Despite this, postpartum anxiety is also of concern given that such symptoms affect maternal well-being, and relate to poor parenting style [27].
Regarding significant demographic risk factors for anxiety symptoms in the first trimester, history of smoking was found to be a significant factor. A lot of previous studies have already provided evidences that cigarette smoking is associated with psychological morbidity such as anxiety disorders [28,29]. Those women with history of smoking may have already developed or manifested anxiety symptoms prior to pregnancy. Thus, their existing and untreated anxiety symptoms may increase the risk of manifesting anxiety symptoms when encountering the challenges and changes in early pregnancy. In addition, the withdrawal symptoms resulting from smoking cessation may increase the vulnerability to experience anxiety symptoms. Other significant demographic variables include marital status, age and educational levels. Pregnant women who are single mothers, who are younger and who attain lower education level, may find more challenges in adjusting a new role and a new set of expectations from themselves and others, and thus they are more likely to manifest anxiety symptoms in early pregnancy.
In turn, significant psychosocial risk factors for anxiety symptoms in the first trimester include unwanted pregnancy, low self esteem, low marital satisfaction and perceived low social support. Previous study [30] found that unwanted pregnancy significantly increased psychological risk. Pregnant women with unwanted pregnancy have more difficulties in accepting the fact of pregnancy as well as adjusting themselves to their maternal role and therefore they may increase their tension and fear in response to such dramatic challenges and changes resulting from their pregnancy. In addition, pregnant women with low self esteem are more likely to be ill prepared to face the developmental transition and all the changes resulting from the pregnancy, thus they increase vulnerability to manifest anxiety symptoms. A meta analysis [31] also reported that self esteem was significantly associated with anxiety symptoms during pregnancy. Women with low marital satisfaction were more likely to report higher level of anxiety symptoms. The present finding is consistent to previous evidence that the quality of marital relationship played an important role in antenatal mood [32]. Well adjusted couples are more likely to have equal attitude toward pregnancy and family formation, thus they are more likely to support each other in the pregnancy and expectant mother is less likely to manifest antenatal anxiety symptoms. Perceived social support is also important to antenatal anxiety symptoms in early pregnancy. The present finding is in line with past studies that there was a significant inverse relationship of social support and anxiety symptoms in pregnancy [31]. The importance of social support for physical and psychological well-being has been well documented [33,34]. Social support is a protective and beneficial factor because it prevents potentially stressful circumstances from being perceived as such or reduces the severity of the reactions to actual stressors [35]. The perception of social support is particularly essential during pregnancy because pregnancy is a time of stress requiring psychological adjustments to physical and role changes.
Another aim of the present study was to examine if anxiety symptoms in early pregnancy could significantly predict anxiety and depressive symptoms in later pregnancy and early postpartum. After adjusting for the effect of potential confounders, anxiety symptoms in the first trimester only significantly predicted anxiety symptoms in the third trimester. Those women who reported higher levels of anxiety symptoms in the first trimester continued to find difficulties in adjusting to their significant physical changes and new maternal roles, and they were more likely to persistently worry and fear about the health of fetus and childbirth during the antenatal period. Although there was a trend for anxiety symptoms in the first trimester to predict postpartum anxiety and depressive symptoms, anxiety and depressive symptoms in the third trimester explained away their associations on multivariate analysis. There is an interval of 8 - 9 months between the first trimester and 6 weeks postpartum. It is fair and reasonable that proximal experience such as anxiety and depressive symptoms experienced in the third trimester are more likely to account for postpartum mental health problems. Despite this, the significance of anxiety symptoms in the first trimester should not be discounted given that they significantly predict anxiety symptoms in the third trimester, and anxiety symptoms in the third trimester are important for postpartum mental health problems. More importantly, previous studies reported that anxiety symptoms in early pregnancy were found to be significantly associated with problems in attention regulation at 3 months and 8 months among infants [36] and also attention deficit hyperactivity disorder (ADHD), externalizing problems, and self report anxiety in 8- and 9-year old children [37].
The present findings are best viewed in light of the methodological constraints of this study. Firstly, the interpretation and application of the findings should be done with caution because the measurement of anxiety and depressive symptoms was solely relied on self report instruments instead of diagnostic tools. However, the measurements which were used in the present study are well-validated and have demonstrated good psychometric properties among Hong Kong Chinese. Other limitation of present study is that non-pregnant comparison group was not included in the present study so that it was unable to tell whether the rates of general anxiety are higher in pregnant women than among non-childbearing women of similar ages. The studies in Italy reported that the prevalence rate of current Axis I disorders was 26.5% during the first trimester of pregnancy [38] but this rate has been estimated to be 4.7% among the general female population in Italy [39]. Little is known of the anxiety. Matched controls should be included in the future studies in order to detect whether the rates of anxiety are different. Last but not least, the attrition rate is relatively high in present study. Pregnant women were asked to fill in questionnaires in all 3 time points starting from the first trimester to 6 weeks postpartum. Antenatal questionnaires were administrated in antenatal clinics. 6 weeks postpartum questionnaires, however, were conducted by mail and thus resulted in a comparatively lower response rate in the postpartum period. The high attrition rate warrants caution in the interpretation of the result. Those who dropped out of the study in the postpartum period may be those at the greatest risk of postpartum anxiety and depression. The dropped out participants may be burdened by infant care and affected by avolition, hence being at higher risk of postpartum mental health problems. The non-response bias might affect the validity and generalization of the findings. However, such potential bias was likely to be minimal based on the results of attrition analysis. The defaulted participants after the childbirth were not found to be different from those who remained in the study in term of demographic characteristics, psychosocial characteristics, mean anxiety and depressive score in the first and third trimesters of the pregnancy.
Despite the limitations, our study highlights anxiety symptoms which are relatively common in pregnant women and thus greater attention should be paid to antenatal anxiety of pregnant women. Screening, detection and intervention for anxiety during early pregnancy are important because pregnant women who have higher levels of anxiety symptoms in the first trimester are more likely to have such symptoms in the third trimesters. Our study also identified significant demographic and psychosocial risk factors for antenatal anxiety in the first trimester. Such knowledge contributes to the effective design of screening, prevention, and intervention strategies, particularly for the high risk groups.
REFERENCES
- Kessler, R., Keller, M. and Wittchen, H. (2001) The epidemiology of generalized anxiety disorder. Psychiatric Clinics of North America, 24, 19-39. doi:10.1016/S0193-953X(05)70204-5
- Grant, K., McMahon, C. and Austin, M. (2008) Maternal anxiety during the transition the transition to parenthood: A prospective study. Journal of Affective Disorders, 108, 101-111. doi:10.1016/j.jad.2007.10.002
- Faisal-Cury, A. and Rossi Menezes, P. (2007) Prevalence of anxiety and depression during pregnancy in a private setting sample. Archives of Women’s Mental Health, 10, 25-32. doi:10.1007/s00737-006-0164-6
- Lee, A.M., Lam, S.K., Sze Mun Lau, S.M., Chong, C.S.Y., Chui, H.W. and Fong, D.Y.T. (2007) Prevalence, course, and risk factors for antenatal anxiety and depres- - sion. Obstetrics & Gynecology, 110, 1102. doi:10.1097/01.AOG.0000287065.59491.70
- Kelly, R.H., Russo, J. and Katon, W. (2001) Somatic complaints among pregnant women cared for in obstetrics: Normal pregnancy or depressive and anxiety symptom amplification revisited? General Hospital Psychiatry, 23, 107-113. doi:10.1016/S0163-8343(01)00129-3
- Laursen, M., Johansen, C. and Hedegaard, M. (2009) Fear of childbirth and risk for birth complications in nulliparous women in the Danish National Birth Cohort. BJOG, 116, 1350-1355. doi:10.1111/j.1471-0528.2009.02250.x
- DiPietro, J.A., Hilton, S.C., Hawkins, M., Costigan, K.A. and Pressman, E.K. (2002) Maternal stress and affect influence fetal neurobehavioral development. Developmental Psychology, 38, 659. doi:10.1037/0012-1649.38.5.659
- Austin, M.P., Tully, L. and Parker, G. (2007) Examining the relationship between antenatal anxiety and postnatal depression. Journal of Affective Disorders, 101, 169-174. doi:10.1016/j.jad.2006.11.015
- Brouwers, E., van Baar, A. and Pop, V. (2001) Maternal anxiety during pregnancy and subsequent infant development. Infant Behavior and Development, 24, 95-106. doi:10.1016/S0163-6383(01)00062-5
- Heron, J., O’Connor, T., Evans, J., Golding, J. and Glover, V. (2004) The course of anxiety and depression through pregnancy and the postpartum in a community sample. Journal of Affective Disorders, 80, 65-73. doi:10.1016/j.jad.2003.08.004
- Zigmond, A.S. and Snaith, R.P. (1983) The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica, 67, 361-370. doi:10.1111/j.1600-0447.1983.tb09716.x
- Snaith, R.P. (2003) The hospital anxiety and depression scale. Health and Quality of Life Outcomes, 1, 29. doi:10.1186/1477-7525-1-29
- Leung, C., Ho, S., Kan, C. and Hung, C. (1993) Evaluation of the Chinese version of the Hospital Anxiety and Depression Scale: A cross-cultural perspective. International Journal of Psychosomatics, 40, 29-34.
- Abiodun, O. (1994) A validity study of the Hospital Anxiety and Depression Scale in general hospital units and a community sample in Nigeria. The British Journal of Psychiatry, 165, 669-672. doi:10.1192/bjp.165.5.669
- Cox, J.L., Holden, J. and Sagovsky, R. (1987) Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. The British Journal of Psychiatry, 150, 782-786. doi:10.1192/bjp.150.6.782
- Murray, D. and Cox, J.L. (1990) Screening for depression during pregnancy with the Edinburgh Depression Scale (EPDS) Journal of Reproductive and Infant Psychology, 8, 99-107. doi:10.1080/02646839008403615
- Bowen, A., Stewart, N., Baetz, M. and Muhajarine, N. (2009) Antenatal depression in socially high-risk women in Canada. Journal of Epidemiology and Community Health, 63, 414-416. doi:10.1136/jech.2008.078832
- Lee, D., Yip, S., Chiu, H., Leung, T., Chan, K., Chau I., et al. (1998) Detecting postnatal depression in Chinese women. Validation of the Chinese version of the Edinburgh Postnatal Depression Scale. The British Journal of Psychiatry, 172, 433-437. doi:10.1192/bjp.172.5.433
- Rosenberg, M. (1965) The measurement of self-esteem. Society and the Adolescent Self Image, 297-307.
- Blascovich, J. and Tomaka, J. (1991) Measures of selfesteem. Measures of Personality and Social Psychological Attitudes, 1, 115-160.
- Schumm, W.R., Crock, R.J., Likcani, A., Akagi, C.G. and Bosch, K.R. (2008) Reliability and validity of the Kansas Marital Satisfaction Scale with different response formats in a recent sample of US Army personnel. Individual Differences Research, 6, 26-37.
- Shek, D.T. and Tsang, S.K. (1993) The Chinese version of the Kansas Marital Satisfaction Scale: Some psychometric and normative data. Social Behavior and Personality: An International Journal, 21, 205-214.
- Schumm, W.R., Scanlon, E.D., Crow, C.L., Green, D.M. and Buckler, D.L. (1983) Characteristics of the Kansas Marital Satisfaction Scale in a sample of 79 married couples. Psychological Reports, 53, 583-588. doi:10.2466/pr0.1983.53.2.583
- Yu, D.S., Lee, D.T. and Woo, J. (2004) Psychometric testing of the Chinese version of the medical outcomes study social support survey (MOS-SSS-C) Research in Nursing & Health, 27, 135-143. doi:10.1002/nur.20008
- Teixeira, C., Figueiredo, B., Conde, A., Pacheco, A. and Costa, R. (2009) Anxiety and depression during pregnancy in women and men. Journal of Affective Disorders, 119, 142-148. doi:10.1016/j.jad.2009.03.005
- Andersson, L., Sundström-Poromaa, I., Wulff, M., Åström, M. and Bixo, M. (2006) Depression and anxiety during pregnancy and six months postpartum: A follow-up study. Acta Obstetricia et Gynecologica Scandinavica, 85, 937- 944. doi:10.1080/00016340600697652
- Gondoli, D.M. and Silverberg, S.B. (1997) Maternal emotional distress and diminished responsiveness: The mediating role of parenting efficacy and parental perspective taking. Developmental Psychology, 33, 861. doi:10.1037/0012-1649.33.5.861
- Glassman, A.H., Helzer, J.E., Covey, L.S., Cottler, L.B., Stetner, F., Tipp, J.E., et al. (1990) Smoking, smoking cessation, and major depression. JAMA: The Journal of the American Medical Association, 264, 1546-1549. doi:10.1001/jama.1990.03450120058029
- Breslau, N., Kilbey, M.M. and Andreski, P. (1991) Nicotine dependence, major depression, and anxiety in young adults. Archives of General Psychiatry, 48, 1069. doi:10.1001/archpsyc.1991.01810360033005
- Bowen, A. and Muhajarine, N. (2006) Antenatal depression. Can Nurse, 102, 26-30.
- Littleton, H.L., Breitkopf, C.R. and Berenson, A.B. (2007) Correlates of anxiety symptoms during pregnancy and association with perinatal outcomes: A meta-analysis. American Journal of Obstetrics and Gynecology, 196, 424-432. doi:10.1016/j.ajog.2007.03.042
- Scottish Intercollegiate Guidelines Network (2002) Postnatal depression and puerperal psychosis. A national clinical guideline. SIGN Executive, Edinburgh.
- Kahn, J., Hessling, R. and Russell, D. (2003) Social support, health, and well-being among the elderly: What is the role of negative affectivity? Personality and Individual Differences, 35, 5-17. doi:10.1016/S0191-8869(02)00135-6
- Sayal, K., Checkley, S., Rees, M., Jacobs, C., Harris, T., Papadopoulos, A., et al. (2002) Effects of social support during weekend leave on cortisol and depression ratings: a pilot study. Journal of Affective Disorders, 71, 153-157. doi:10.1016/S0165-0327(01)00414-1
- Kearns, B., Neuwelt, C., Patricia, M., Hitchman, M. and Lennan, B. (1997) Social support and psychological distress before and after childbirth. Health & Social Care in the Community, 5, 296-308. doi:10.1111/j.1365-2524.1997.tb00126.x
- Huizink, A.C., Mulder, E.J.H., Robles de Medina, P.G., Visser, G.H.A. and Buitelaar, J.K. (2004) Is pregnancy anxiety a distinctive syndrome? Early Human Development, 79, 81-91. doi:10.1016/j.earlhumdev.2004.04.014
- Van den Bergh, B.R.H. and Marcoen, A. (2004) High antenatal maternal anxiety is related to ADHD symptoms, externalizing problems, and anxiety in 8- and 9-year-old. Child Development, 75, 1085-1097. doi:10.1111/j.1467-8624.2004.00727.x
- Borri, C., Mauri, M., Oppo, A., Banti, S., Rambelli, C., Ramacciotti, D., et al. (2008) Axis I psychopathology and functional impairment at the third month of pregnancy: Results from the Perinatal Depression-Research and Screening Unit (PND-ReScU) study. The Journal of Clinical Psychiatry, 69, 1617. doi:10.4088/JCP.v69n1012
- de Girolamo, G., Polidori, G., Morosini, P., Scarpino, V., Reda, V., Serra, G., et al. (2006) Prevalence of common mental disorders in Italy. Social Psychiatry and Psychiatric Epidemiology, 41, 853-861. doi:10.1007/s00127-006-0097-4
NOTES
*This study was supported by a grant from the General Research Fund of the Research Grants Council of the Hong Kong Special Administrative Region (Ref: CERG HKU7470/06H).
#Corresponding author.

