Journal of Cosmetics, Dermatological Sciences and Applications
Vol.2 No.4(2012), Article ID:25865,2 pages DOI:10.4236/jcdsa.2012.24049
A Case of Erythema Nodosum Associated with Subareolar Abscess
![]()
1Departments of Dermatology, Graduate School of Medicine, Hirosaki University, Hirosaki, Japan; 2Departments of Surgery, Graduate School of Medicine, Hirosaki University, Hirosaki, Japan.
Email: *derma@cc.hirosaki-u.ac.jp
Received August 1st, 2012; revised September 3rd, 2012; accepted September 14th, 2012
Keywords: Erythema Nodosum; Subareolar Abscess; Breast; Staphylococcal Infections
ABSTRACT
While erythema nodosum is a nodular, erythematous eruption predominantly affecting the extensor aspects of the legs, breast abscesses are the result of relatively common bacterial infections, and only 2 studies have reported an association between erythema nodosum and breast abscesses. Here, we report the case of a patient with repeated erythema nodosum associated with subareolar abscesses. The patient was a 34-year-old woman with painful erythematous nodules on her right shin, accompanied by an indurated lesion on her right breast 4 days before the onset of the nodules. Therefore, the patient underwent circumareolar incision, and consequently the painful erythematous nodules disappeared. However, after 39 days, the patient developed another tender, painful lesion in her right breast and painful erythematous nodules on her right shin. After another circumareolar incision, the painful erythematous nodules disappeared again. Therefore, we suggested a significant association between erythema nodosum and breast abscess in this patient. The most common underlying causative organism in breast abscess is Staphylococcus aureus; however, erythema nodosum has rarely been proven to be associated with staphylococcal infections. Therefore, the relationship between S. aureus and erythema nodosum is rather controversial. However, the resistance to the usual treatment methods and prolonged clinical course in our case suggest that the pathogenesis of erythema nodosum associated with breast abscesses might be different from that of the common form of erythema nodosum.
1. Case Report
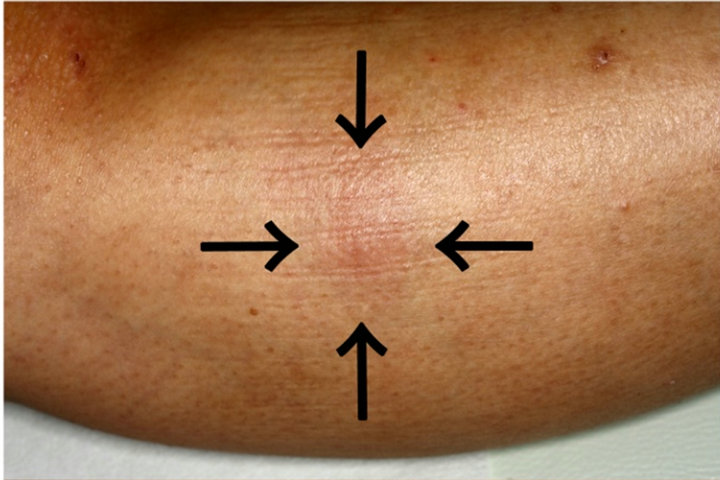
A 34-year-old woman with an 8-day history of multiple painful erythematous nodules on her shin was admitted to our hospital (Figure 1(a)). A skin biopsy showed histological features that were compatible with erythema nodosum (EN). Careful examination showed no evidence of any underlying common causes of EN such as streptococcal infection, tuberculosis, Behçet’s disease, sarcoidosis, enteropathies, or malignancies. In addition, the patient had no history of oral contraceptive pills or hormone replacement. Four days before the onset of nodules on her legs, however, she was diagnosed with subareolar abscess.
Before admission to our hospital, the patient experienced pain in her right breast for 6 weeks and also had slight fever for 4 weeks. First, she visited a general practitioner, and mastadenitis was detected by ultrasonography and mammography. In addition, although the patient had gross hematuria, the results of cystoscopic examination were normal. Then, the patient consulted the mammary surgeon at our hospital. She presented with a 40- mm-diameter, painful, indurated lesion on her right breast. Ultrasound examination of her right breast revealed an extensive abscess under the nipple and areola. Therefore, the patient was prescribed an antibiotic (cefdinir 300 mg/day for 4 days) and a painkiller (loxoprofen sodium 180 mg/day for 4 days); however, the patient continued to experience pain. In the meanwhile, the patient noticed painful lesions on the leg, and finally was admitted to our hospital.
The patient was administered an antibiotic and painkiller for 2 weeks; however, owing to the poor efficacy of the drugs in treating the subareolar abscess, the abscess persisted. Therefore, the surgeon incised the abscess and drained the pus. Further, negative culture was obtained from her lesions. After a circumareolar incision, the painful erythematous nodules on her right shin disappeared, with consequent pigmentation of the skin.
After 39 days, the patient developed another tenderpainful area in her right breast (Figure 1(b)), accompanied with painful erythematous nodules on her right shin. She was treated with surgical drainage and intravenous antibiotics again (Figure 1(b)). After another circumareolar incision, the painful erythematous nodules on her shin disappeared again. Subsequently, we diagnosed this patient with EN associated with breast abscess.
2. Discussion
EN is a nodular, erythematous eruption predominantly affecting the extensor aspects of the legs, and is associated with a wide variety of diseases [1]. In brief, the causes of EN may be classified as follows: infections with bacteria, fungi, or protozoa; viral diseases; malignancies; medications; and miscellaneous conditions. Breast abscesses are the result of relatively common bacterial infections, but only 2 study has reported an association between EN and breast abscess [2,3].
Breast abscess is a relatively common infection, classified into 2 types: acute puerperal breast abscess and
 (a)
(a) (b)
(b)
Figure 1. (a) Upper panel: A nodular erythematous lesion on the shin (arrows indicates 1 lesion); (b) Lower panel: The patient developed another tender, painful area in her right breast. Scars of previous drainage are evident.
duct ectasia [4]. She had the baby 3 years ago. She discontinued breast-feeding about a year and a half ago. The American Academy of Periodontology recommends breastfeeding till 1 year. Breastfeeding supports an infant’s immune system. Undernourished children and those not exclusively breast-fed for the first 6 months of life are at a high risk of developing pneumonia and other disease as well. Mastitis is a breast abscess that occurs in lactating women when a milk duct gets plugged. Subareolar abscess occurs in young to middle-aged nonlactating women, and involves the nipple tissue or areolar glands. She had no trouble breast-feeding. In the present case, the patient’s condition corresponded to duct ectasia. Duct ectasia-related abscesses occur in nonlactating women, often toward the end of their reproductive years.
Here we report a case of EN associated with breast abscess. Our investigations showed no evidence of infection, but the most common underlying causative organism in breast abscesses is Staphylococcus aureus [4,5]. However, EN has rarely been proven to be associated with staphylococcal infections [3,6]. Thus, the relationship between S. aureus and EN is rather controversial. Moreover, the resistance to the usual treatment methods and prolonged clinical course in our case suggest that the pathogenesis of EN associated with breast abscess might be different from that of the more common forms of EN. Further research to identify causative microorganism in EN associated with breast abscess is required.
REFERENCES
- L. Requena and C. Requena, “Erythema Nodosum,” Dermatology Online Journal, Vol. 8, No. 1, 2002, p. 4.
- K. Al Benwan, A. Al Mulla, H. Izumiya and M. J. Albert, “Erythema Nodosum and Bilateral Breast Abscesses Due to Salmonella Enterica Serotype Poona,” Journal of Clinical Microbiology, Vol. 48, No. 10, 2010, pp. 3786- 3787. doi:10.1128/JCM.00780-10
- H. Ujiie, D. Sawamura, K. Yokota, Y. Tateishi, D. Inokuma and H. Shimizu, “Intractable Erythema Nodosum Associated with Severe Breast Abscesses: Reports of Two Cases,” Clinical and Experimental Dermatology, Vol. 30, No. 5, 2005, pp. 584-589.
- E. A. Benson, “Management of Breast Abscesses,” World Journal Surgery, Vol. 13, No. 6, 1989, pp. 753-756. doi:10.1007/BF01658428
- D. A. Ekland and M. G. Zeigler, “Abscess in the Nonlactating Breast,” Archives of Surgery, Vol. 107, No. 3, 1973, pp. 398-401. doi:10.1001/archsurg.1973.01350210034011
- B. Cribier, A. Caille, E. Heid and E. Grosshans, “Erythema Nodosum and Associated Diseases. A Study of 129 Cases,” International Journal of Dermatology, Vol. 37, No. 9, 1998, pp. 667-672. doi:10.1046/j.1365-4362.1998.00316.x
NOTES
*Corresponding author.

