M. CHALKOO ET AL.
138
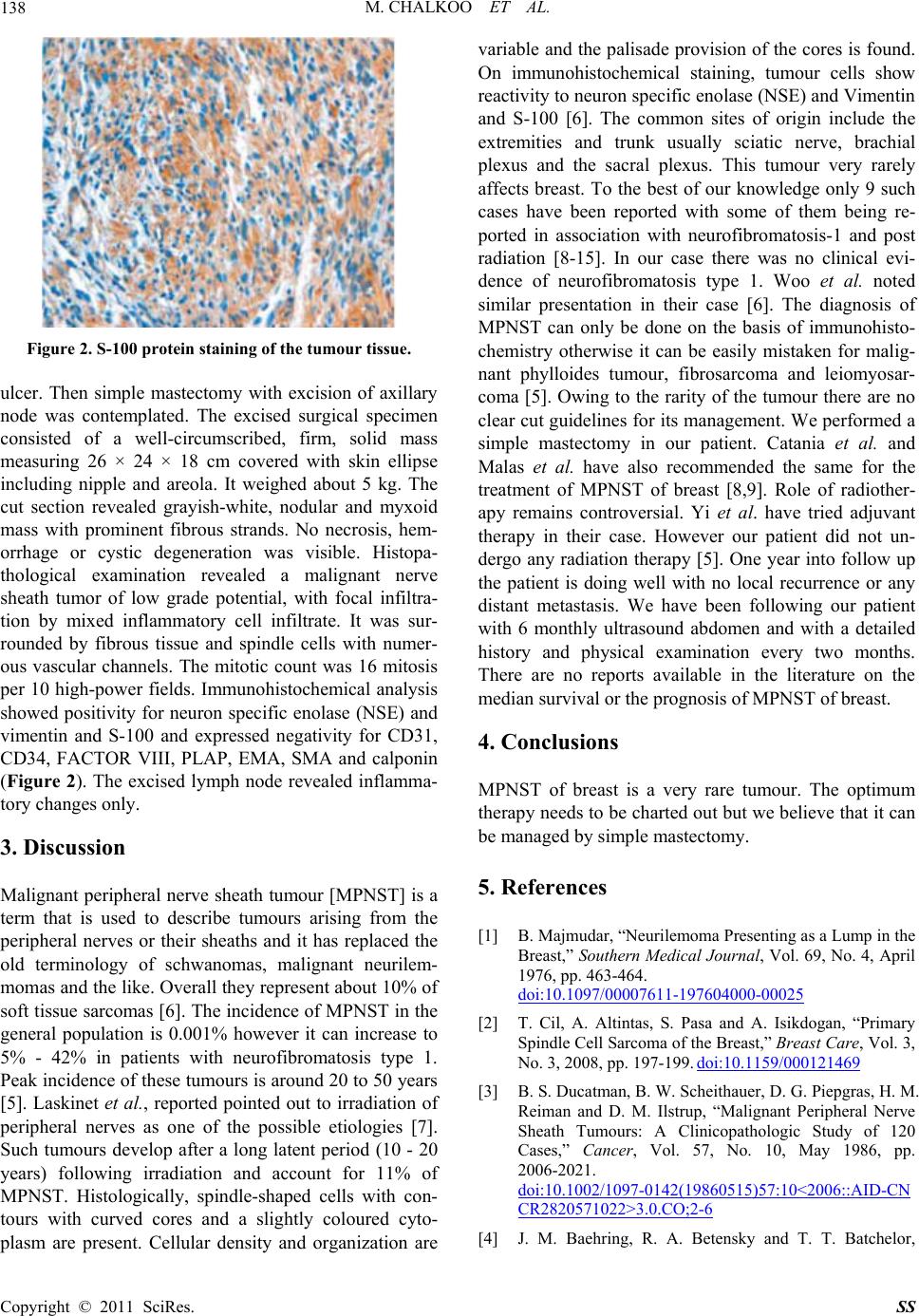
Figure 2. S-100 protein staining of the tumour tissue.
ulcer. Then simple mastectomy with excision of axillary
node was contemplated. The excised surgical specimen
consisted of a well-circumscribed, firm, solid mass
measuring 26 × 24 × 18 cm covered with skin ellipse
including nipple and areola. It weighed about 5 kg. The
cut section revealed grayish-white, nodular and myxoid
mass with prominent fibrous strands. No necrosis, hem-
orrhage or cystic degeneration was visible. Histopa-
thological examination revealed a malignant nerve
sheath tumor of low grade potential, with focal infiltra-
tion by mixed inflammatory cell infiltrate. It was sur-
rounded by fibrous tissue and spindle cells with numer-
ous vascular channels. The mitotic count was 16 mitosis
per 10 high-power fields. Immunohistochemical analysis
showed positivity for neuron specific enolase (NSE) and
vimentin and S-100 and expressed negativity for CD31,
CD34, FACTOR VIII, PLAP, EMA, SMA and calponin
(Figure 2). The excised lymph node revealed inflamma-
tory changes only.
3. Discussion
Malignant peripheral nerve sheath tumour [MPNST] is a
term that is used to describe tumours arising from the
peripheral nerves or their sheaths and it has replaced the
old terminology of schwanomas, malignant neurilem-
momas and the like. Overall they represent about 10% of
soft tissue sarcomas [6]. The incidence of MPNST in the
general population is 0.001% however it can increase to
5% - 42% in patients with neurofibromatosis type 1.
Peak incidence of these tumours is around 20 to 50 years
[5]. Laskinet et al., reported pointed out to irradiation of
peripheral nerves as one of the possible etiologies [7].
Such tumours develop after a long latent period (10 - 20
years) following irradiation and account for 11% of
MPNST. Histologically, spindle-shaped cells with con-
tours with curved cores and a slightly coloured cyto-
plasm are present. Cellular density and organization are
variable and the palisade provision of the cores is found.
On immunohistochemical staining, tumour cells show
reactivity to neuron sp ecific enolase (NSE) an d Vimentin
and S-100 [6]. The common sites of origin include the
extremities and trunk usually sciatic nerve, brachial
plexus and the sacral plexus. This tumour very rarely
affects breast. To the best of our knowledge only 9 such
cases have been reported with some of them being re-
ported in association with neurofibromatosis-1 and post
radiation [8-15]. In our case there was no clinical evi-
dence of neurofibromatosis type 1. Woo et al. noted
similar presentation in their case [6]. The diagnosis of
MPNST can only be done on the basis of immunohisto-
chemistry otherwise it can be easily mistaken for malig-
nant phylloides tumour, fibrosarcoma and leiomyosar-
coma [5]. Owing to the rarity of the tumour there are no
clear cut guidelines for its management. We performed a
simple mastectomy in our patient. Catania et al. and
Malas et al. have also recommended the same for the
treatment of MPNST of breast [8,9]. Role of radiother-
apy remains controversial. Yi et al. have tried adjuvant
therapy in their case. However our patient did not un-
dergo any radiation therapy [5]. One year into follow up
the patient is doing well with no local recurrence or any
distant metastasis. We have been following our patient
with 6 monthly ultrasound abdomen and with a detailed
history and physical examination every two months.
There are no reports available in the literature on the
median survival or the prognosis of MPNST of breast.
4. Conclusions
MPNST of breast is a very rare tumour. The optimum
therapy need s to be charted out but we believ e that it can
be managed by simple mastectomy.
5. References
[1] B. Majmudar, “Neurilemoma Presenting as a Lump in the
Breast,” Southern Medical Journal, Vol. 69, No. 4, April
1976, pp. 463-464.
doi:10.1097/00007611-197604000-00025
[2] T. Cil, A. Altintas, S. Pasa and A. Isikdogan, “Primary
Spindle Cell Sarcoma of the Breast,” Breast Care, Vol. 3,
No. 3, 2008, pp. 197-199. doi:10.1159/000121469
[3] B. S. Ducatman, B. W. Scheithauer, D. G. Piepgras, H. M.
Reiman and D. M. Ilstrup, “Malignant Peripheral Nerve
Sheath Tumours: A Clinicopathologic Study of 120
Cases,” Cancer, Vol. 57, No. 10, May 1986, pp.
2006-2021.
doi:10.1002/1097-0142(19860515)57:10<2006::AID-CN
CR2820571022>3.0.CO;2-6
[4] J. M. Baehring, R. A. Betensky and T. T. Batchelor,
Copyright © 2011 SciRes. SS