 International Journal of Clinical Medicine, 2013, 4, 556-560 Published Online December 2013 (http://www.scirp.org/journal/ijcm) http://dx.doi.org/10.4236/ijcm.2013.412096 Open Access IJCM The Role of Helicobacter pylori Infection, and Malnutrition among Type 2 Diabetic Medical Services Patients in the Gaza Strip Mazen A. El-Sakka1, Ektemal M. Abu Jabal2, Luay M. Nasser3 1Pharmacognosy Department, Faculty of Pharmacy, Al Azhar University-Gaza, Gaza, Palestine; 2Nutrition Department, Ministry of National Economy, Gaza, Palestine; 3Medical Service, Gaza, Palestine. Email: sakkamazen@gmail.com Received October 12th, 2013; revised November 10th, 2013; accepted December 3rd, 2013 Copyright © 2013 Mazen A. El-Sakka et al. This is an open access article distributed under the Creative Commons Attribution Li- cense, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. ABSTRACT Background: Diabetes means the blood glucose, which is too high or too low. With Type 2 DM, the more common type, the body does not make o r use insulin well. In patients with DM, Helicobacter pylori is one of the most common infections worldwide. Available data on the possible association between H. pylori infection and DM are contradictory. There are a few studies in the Middle East, and this study is the pioneer study, in the Medical Services Clinics in Gaza strip. Aims: This study was conducted to reveal the prevalence of H. pylori infection, malnutrition, insulin resistance among T2DM patients, to describe the dietary requirements of T2DM patients, finally to evaluate the current informa- tion about diet, and lifestyle in the prevention of H. pylori, and malnutrition. Methodology: A cross-sectional study was conducted in the Medical Services Clinics in Gaza Strip, and there were 129 patients included in this study. Data were collected through hematological information and structured interview questionnaire. Results: Highly significant per- centage of H. pylori (70%) among the DM patients includes in the study, but not indicates any significant association between gender and H. pylori status. Conclusion: H. pylori patients should update their sugar level valu es in the record, and should get exercise and diet plan for every meal. Keywords: Type 2 Diabetes Mellitus (T2DM); Helicobacter pylori (H. pylori); Insulin Resistance (IR); Malnutrition 1. Introduction In recent years, a significant association has been re- ported between cardiovascular diseases, d iabetes mellitus, and dyslipidemia and Helicobacter pylori (H. pylori) infection. However, there are conflicting reports, and lack of data from the Middle East should prompt local studies for establishing the relationship between H. py- lori and such chronic diseases [1]. In patients with diabetes mellitus (DM), chronic infec- tions are frequent and severe, due to the impairment of their immune status. However, data on the prevalence of Helicobacter pylori infection in diabetics are scanty and contradictory. Patients with insulin-dependent diabetes mellitus (IDDM) are often affected by chronic infections [1]. Diabetes Mellitus means the blood glucose, or blood sugar are too high. With Type 2 diabetes mellitus, the more comm on type, the body does not make or use insulin well. Insulin is a hormone that h elps gluco se gets in to the cells to give them energy. Without insulin, too much glucose stays in the blood. Over time, high blood glucose can lead to serious problems with heart, eyes, kidneys, nerves, gums and teeth [2]. Helicobacter pylori are one of the most common in- fections worldwide. Available data on the possible asso- ciation between H. pylori infection and diabetes mellitus (DM) are contradictory [3]. That is clearly indicated there is a considerable nutri- tional public problem. The intention of the study is to assess the nutritional status of the diabetic patients, whom have H. pylori bacteria in their stomach, and to determine the nutritional factors contributing in devel- opment of nutritional diabetic patients [4]. Since there are only a few studies in the Middle East, on the association of Helicobacter pylori and diabetes mellitus, we conducted this study and focus on the fre- quency of Helicobacter pylori infection, Insulin resis- 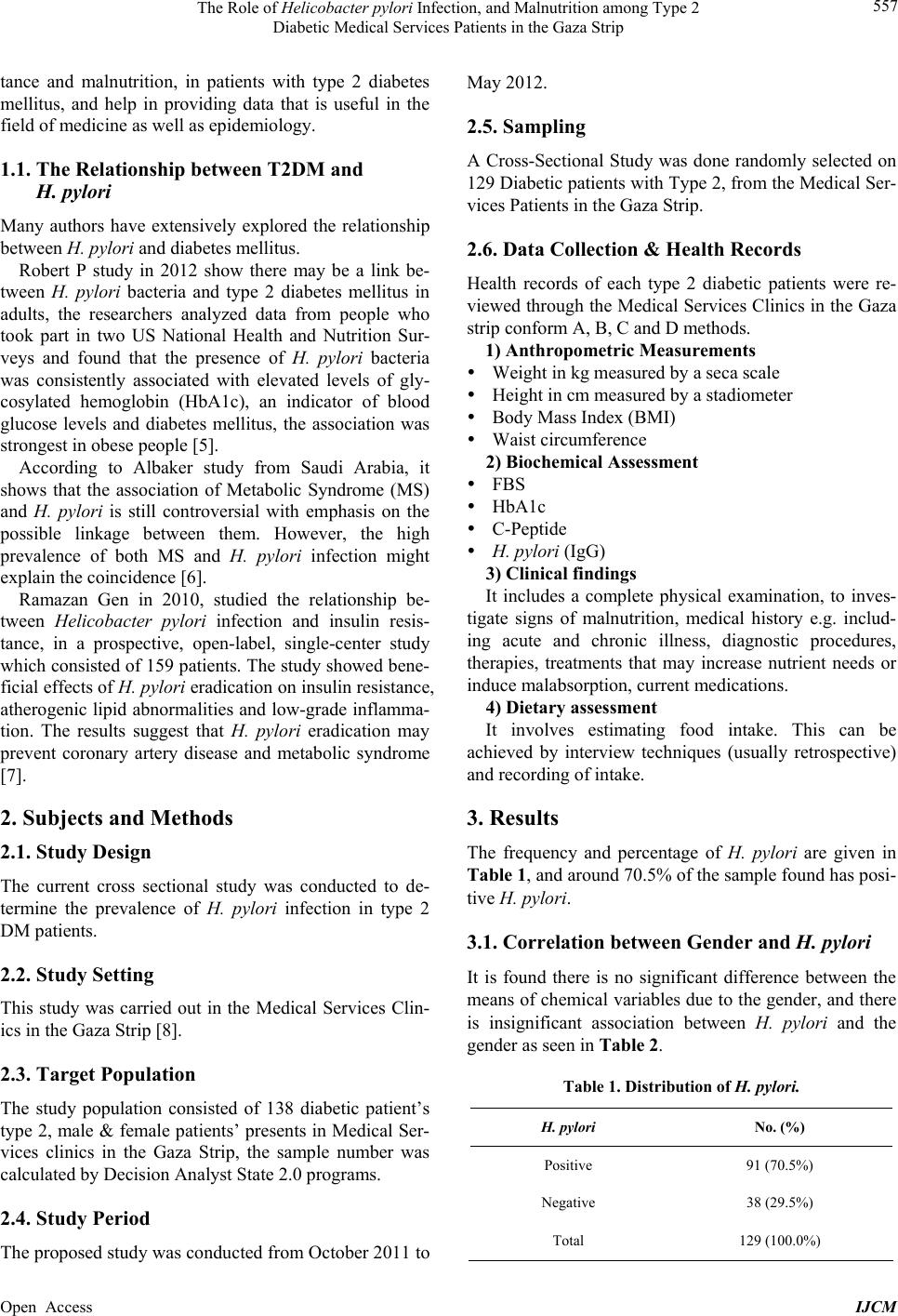 The Role of Helicobacter pylori Infection, and Malnutrition among Type 2 Diabetic Medical Services Patients in the Gaza Strip 557 tance and malnutrition, in patients with type 2 diabetes mellitus, and help in providing data that is useful in the field of medicine as well as epidemiology. 1.1. The Relationship between T2DM and H. pylori Many authors have extensively explored the relationship between H. pyl ori and diabetes mellitus. Robert P study in 2012 show there may be a link be- tween H. pylori bacteria and type 2 diabetes mellitus in adults, the researchers analyzed data from people who took part in two US National Health and Nutrition Sur- veys and found that the presence of H. pylori bacteria was consistently associated with elevated levels of gly- cosylated hemoglobin (HbA1c), an indicator of blood glucose levels and diabetes mellitus, the association was strongest in obese people [5]. According to Albaker study from Saudi Arabia, it shows that the association of Metabolic Syndrome (MS) and H. pylori is still controversial with emphasis on the possible linkage between them. However, the high prevalence of both MS and H. pylori infection might explain the coincidence [6]. Ramazan Gen in 2010, studied the relationship be- tween Helicobacter pylori infection and insulin resis- tance, in a prospective, open-label, single-center study which consisted of 159 patients. The study show ed bene- ficial effects of H. pylori eradication on insulin resistance, atherogenic lipid abno rmalities and low-grade inflamma- tion. The results suggest that H. pylori eradication may prevent coronary artery disease and metabolic syndrome [7]. 2. Subjects and Methods 2.1. Study Design The current cross sectional study was conducted to de- termine the prevalence of H. pylori infection in type 2 DM patients. 2.2. Study Setting This study was carried out in the Medical Services Clin- ics in the Gaza Strip [8]. 2.3. Target Population The study population consisted of 138 diabetic patient’s type 2, male & female patients’ presents in Medical Ser- vices clinics in the Gaza Strip, the sample number was calculated by Decision Analyst State 2.0 programs. 2.4. Study Period The proposed study was conducted from October 2011 to May 2012. 2.5. Sampling A Cross-Sectional Study was done randomly selected on 129 Diabetic patients with Type 2, from the Medical Ser- vices Patients in the Gaza Strip. 2.6. Data Collection & Health Records Health records of each type 2 diabetic patients were re- viewed through the Medical Services Clinics in the Gaza strip conform A, B, C and D methods. 1) Anthropometric Measurements Weight in kg measured by a seca scale Height in cm measured by a stadiometer Body Mass Index (BMI) Waist circumference 2) Biochemical Assessment FBS HbA1c C-Peptide H. pylori (IgG) 3) Clinical findings It includes a complete physical examination, to inves- tigate signs of malnutrition, medical history e.g. includ- ing acute and chronic illness, diagnostic procedures, therapies, treatments that may increase nutrient needs or induce malabsorption, current medications. 4) Dietary assessment It involves estimating food intake. This can be achieved by interview techniques (usually retrospective) and recording of intake. 3. Results The frequency and percentage of H. pylori are given in Table 1, and around 70.5 % of the sample found has posi- tive H. pylori. 3.1. Correlation between Gender and H. pylori It is found there is no significant difference between the means of chemical variables due to the gender, and there is insignificant association between H. pylori and the gender as seen in Table 2. Table 1. Distribution of H. pylori. H. pylori No. (%) Positive 91 (70.5%) Negative 38 (29.5%) Total 129 (100.0%) Open Access IJCM 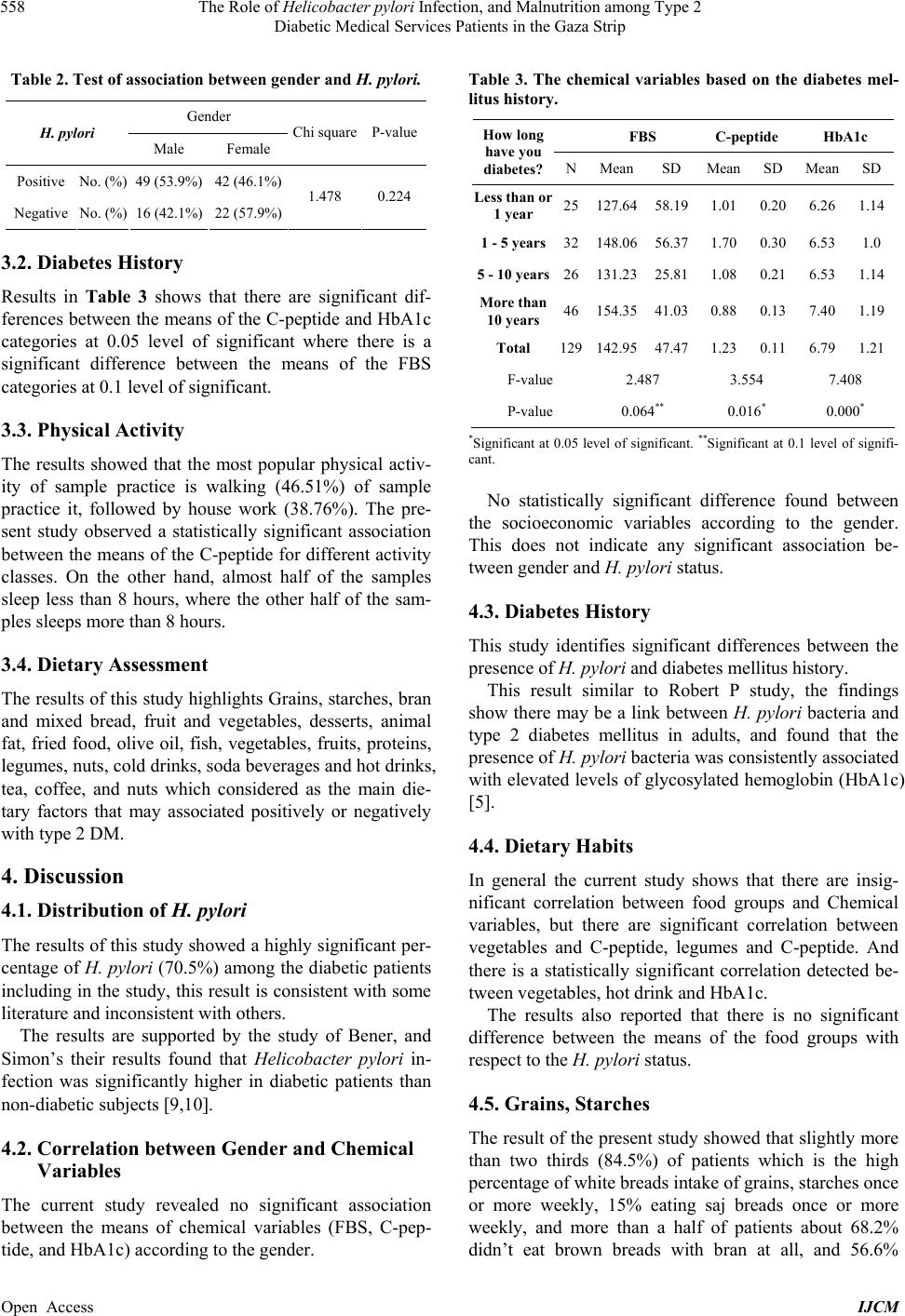 The Role of Helicobacter pylori Infection, and Malnutrition among Type 2 Diabetic Medical Services Patients in the Gaza Strip 558 Table 2. Test of association betw ee n gender and H. pylori. Gender H. pylori Male Female Chi squareP-value Positive No. (%) 49 (53.9%) 42 (46.1%) Negative No. (%) 16 (42.1%) 22 (57.9%) 1.478 0.224 3.2. Diabetes History Results in Table 3 shows that there are significant dif- ferences between the means of the C-peptide and HbA1c categories at 0.05 level of significant where there is a significant difference between the means of the FBS categories at 0.1 level of significant. 3.3. Physical Activity The results showed that the most popular physical activ- ity of sample practice is walking (46.51%) of sample practice it, followed by house work (38.76%). The pre- sent study observed a statistically significant association between the means of the C-pe ptide for different activity classes. On the other hand, almost half of the samples sleep less than 8 hours, where the other half of the sam- ples sleeps more than 8 hours. 3.4. Dietary Assessment The results of this study highlights Grains, starches, bran and mixed bread, fruit and vegetables, desserts, animal fat, fried food, olive oil, fish, vegetables, fruits, proteins, legumes, nuts, cold drinks, soda beverages and hot drinks, tea, coffee, and nuts which considered as the main die- tary factors that may associated positively or negatively with type 2 DM. 4. Discussion 4.1. Distribution of H. pylori The results of this study showed a highly significant per- centage of H. pylori (70.5%) among the diabetic patients including in the study, this resu lt is consistent with some literature and inconsistent with others. The results are supported by the study of Bener, and Simon’s their results found that Helicobacter pylori in- fection was significantly higher in diabetic patients than non-diabetic subjects [9,10]. 4.2. Correlation between Gender and Chemical Variables The current study revealed no significant association between the means of chemical variables (FBS, C-pep- tide, and HbA1c) according to the gender. Table 3. The chemical variables based on the diabetes mel- litus history. FBS C-peptide HbA1c How long have you diabetes? NMeanSD Mean SD MeanSD Less than or 1 year 25127.6458.19 1.01 0.20 6.261.14 1 - 5 years32148.0656.37 1.70 0.30 6.531.0 5 - 10 years26131.2325.81 1.08 0.21 6.531.14 More than 10 years 46154.3541.03 0.88 0.13 7.401.19 Total 129142.9547.47 1.23 0.11 6.791.21 F-value 2.487 3.554 7.408 P-value 0.064** 0.016* 0.000* *Significant at 0.05 level of significant. **Significant at 0.1 level of signifi- cant. No statistically significant difference found between the socioeconomic variables according to the gender. This does not indicate any significant association be- tween gender and H. pylori status. 4.3. Diabetes History This study identifies significant differences between the presence of H. pylori and diabetes mellitus history. This result similar to Robert P study, the findings show there may be a link between H. pylori bacteria and type 2 diabetes mellitus in adults, and found that the presence of H. pylori bacteria was consistently associated with elevated levels of glycosylated hemoglobin (HbA1c) [5]. 4.4. Dietary Habits In general the current study shows that there are insig- nificant correlation between food groups and Chemical variables, but there are significant correlation between vegetables and C-peptide, legumes and C-peptide. And there is a statistically significant correlation detected be- tween vegetables, hot drink and H bA1c. The results also reported that there is no significant difference between the means of the food groups with respect to the H. pylori status. 4.5. Grains, Starches The result of the present stu dy showed that slightly more than two thirds (84.5%) of patients which is the high percentage of white brea ds int a ke of grains, st arches once or more weekly, 15% eating saj breads once or more weekly, and more than a half of patients about 68.2% didn’t eat brown breads with bran at all, and 56.6% Open Access IJCM  The Role of Helicobacter pylori Infection, and Malnutrition among Type 2 Diabetic Medical Services Patients in the Gaza Strip 559 didn’t eat brown breads without bran at all. The present study results show that 11.6% from the samples eating macaroni/spaghetti once per day or more, and 47.3% of patient didn’t intake it at all. In general terms, most of the studies revealed th at con- sumption of refined sugars is directly associated with diabetes mellitus disea se [ 11]. 4.6. Fruit The current study shows that more than two thirds (79.1%) of patients eating and drinking citrus as orange grapefruits and lemons, once per day or more, and only 1.6% percentage didn’t intake it at all. The results show that 60.5% of patients eating the ap- ples once or more per day, then 34.9% patients eaten watermelon once or more per day, in the end of the fruits list comes the pineapple (fresh/canned) which taken by 17.8% of the diabeti c pati ent s. 4.7. Vegetables Some studied shows that the regular consumption of fruit and vegetables is associated with reduced risks of chro- nic diseases, where they contain significant amounts of bioactive components and fibers that may provide desir- able health benefits beyond basic nutrition [12]. The cur- rent study shows that (34% - 44%) of patients eating a cooked vegetables as okra, molokhia, zucchini, potato (cooked/boiled/or mashed), green beans, spinach, once or more per day, and the results shows that about 67.4% from patients are eating vegetable salad daily, and in other patients taken once or more per day. 4.8. Proteins The study results show that more than 40% from diabetic patient intake milks, yo gurts, cheeses, eggs, and between 18% - 30% from the samples didn’t eat them at all. And about 69.8% from chickens, that’s because the diabetic patients inclu ding in the study prefer the ch icken more than other meats and intake it once or more per weeks, where 1.6% from patients don’t eat it at all. 4.9. Legumes The results show that diabetic patients often eating leg- ume as lentil, pea, chickpeas, bean with sesame paste, green beans, about 50% - 55% of patients eating legumes one or more per day, and 10% from patients didn’t eat legumes at all. 4.10. Nuts The results show that 20% - 24% from patients eats nuts as (peanuts, walnuts, sunflower, watermelon, almonds), once or more per weeks, and the higher percentage of patients didn’t eat it at all. 4.11. Desert The results show that 11.6% only from the diabetic pa- tients eat keck (others), and 30.6% from samples eat home sweats, but the higher percentage of diabetic pa- tients didn’t eats keck or oriented sweats at all, because of their effects of elevated the blood sugar. 4.12. Cold & Hot Drinks The results found that 57.4% drinks the fresh fruits juice, and 31% from patients didn’t drink it at all, about 21.7% drink soda, and 57.4% from the samples didn’t drinks it at all, about 76.7% from patients drinks tea, 55% drinks coffee, and 20% - 24 % from them drinking cinnamon, ginger, and herbal tea. 4.13. Fried Food The study showed consumption of fried foods and exces- sive oil about 52.7% eats (flafel, potato, eg gplants, cauli- flower), and 18.6% only didn’t eat it at all. 4.14. Fast Food The results showed little consumption of fast foods (as pizza, shawerma, borger, thailandy) only about 3.9% - 9.3% eats fast foods, and 85% didn’t eat it at all. 4.15. Spices The results found that all the samples takes spices as red/green pepper black pepper, curcuma, other spices with in the foods, 79.8% - 82% eat it once or more per day. 4.16. Pickles The results show that 43.4% intake the pickles as home- made olives once or more per day, and 37.2% didn’t eat the homemade, an d 70.0 % fr om the patient didn’t eat any pickles from market at all. 5. Conclusions & Recommendation In the present study, H. pylori infection, insulin resis- tance and malnutrition in type 2 DM patients, were done for all subjects. 1) An adequate lifestyle, socioeconomic factors, and some biochem ical altera tions coul d play an import ant role in the etiology of type 2 DM pat i e nt s. 2) This study d emonstrates t he strong relati onship of H. pylori infection a s a risk factor fo r insulin resi stance, more than 70.5% of the samples found to have positive H. py- Open Access IJCM  The Role of Helicobacter pylori Infection, and Malnutrition among Type 2 Diabetic Medical Services Patients in the Gaza Strip Open Access IJCM 560 lori. 3) Greater attention of the eradication of H. pylori has been shown to play important roles in the etiology of other chronic diseases. 4) We can conclude that there is insignificant associa- tion between the H. pylori and diabetes mellitus history (the duration of diabetes). H. pylori infection is not asso- ciated with duration of diabetes, 5) The study exhibited a positive significant difference between the means of weight for persons with positive and negative H. pylori status. Consequently, the mean of BMI of positive groups is significantly higher than the mean BMI for the negative group. 6) The results suggest that data seem to indicate a po- tential association between H. pylori infection, malnutri- tion and IR, and further studies are needed to strengthen this association and to clarify whether there is a causative link between t hem. Serum H. pylori should be integrated into routinely para-clinical investigations in all patients with type 2 DM. REFERENCES [1] A. Baradaran and H. Nasri, “Helicobacter pylori Specific IgG Antibody and Serum Magnesium in Type-2 Diabetes Mellitus Chronic Kidney Disease Patients,” Saudi Jour- nal of Kidney Diseases and Transplantation, Vol. 22, No. 2, 2011, pp. 282-285. [2] National Institutes of Health (NIH), “A Service of the U.S. National Library of Medicine. Annual Report,” 2012, [3] S. A. Polyzos, J. Kountouras, C. Zavos and G. Deretzi, “The Association between Helicobacter pylori Infection and Insulin Resistance; Part 1,” Heicobacter Journal, Vol. 16, No. 1, 2010, pp. 76-88. [4] M. D. Goutham Rao, “Insulin Resistance Syndrome,” American Family Physician, Vol. 63, No. 6, 2001, pp. 1159-1164. [5] R. Preidt, “Type of Bacteria May Be Linked to Diabetes, The Association between H. pylori Infection, Type 2 Dis- ease,” A Service of the US National Library of Medicine, 2012. [6] W. I. Albaker, “Helicobacter pylori Infection and Its Re- lationship to Metabolic Syndrome: Is It a Myth or Fact?” Saudi Journal of Gastroenterology, Vol. 17, No. 3, 2011, pp. 165-169. http://dx.doi.org/10.4103/1319-3767.80377 [7] R. Gen, M. Demir and H. Ataseven, “Effect of Helico- bacter pylori Eradication on Insulin Resistance, Serum Lipids and Low-Grade Inflammation,” Southern Medical Journal, Vol. 103, No. 3, 2010, pp. 190-196. http://dx.doi.org/10.1097/SMJ.0b013e3181cf373f [8] Medical Services Commission, Annual Report 2010/ 2011. [9] A. Bener, S. A. Uduman, A. Ameen, et al., “Prevalence of Helicobacter pylori Infection among Low Socio-Eco- nomic Workers,” Journal of Communicable Diseases, Vol. 34, No. 3, 2002, pp. 179-184. [10] L. Simon’s, J. Tornoczky, M. Toth, M. Jambor and Z. Sudar, “The Significance of Campylobacter pylori Infec- tion in Gastroenterologic and Diabetic Practice,” Orvosi Hetilap, Vol. 130, No. 25, 1989, pp. 1325-1329. [11] A. Cuevas, J. Miquel, M. Reyes and F. Nervi, “Diet as a Risk Factor for Cholesterol Gallstone Disease,” Journal of the American College of Nutrition, Vol. 23, No. 3, 2004, pp. 187-196. [12] R. Liu, “Health Benefits of Fruit and Vegetables Are from Additive and Synergistic Combinations of Phyto- chemicals,” American Journal of Clinical Nutrition, Vol. 78, No. 3, 2003, pp. 517-520.
|