Secondary Reconstruction of Recurrent Primary Intraosseous Meningioma of the
Calvarium Using a Fasciocutaneous Anterolateral Thigh Free Flap
282
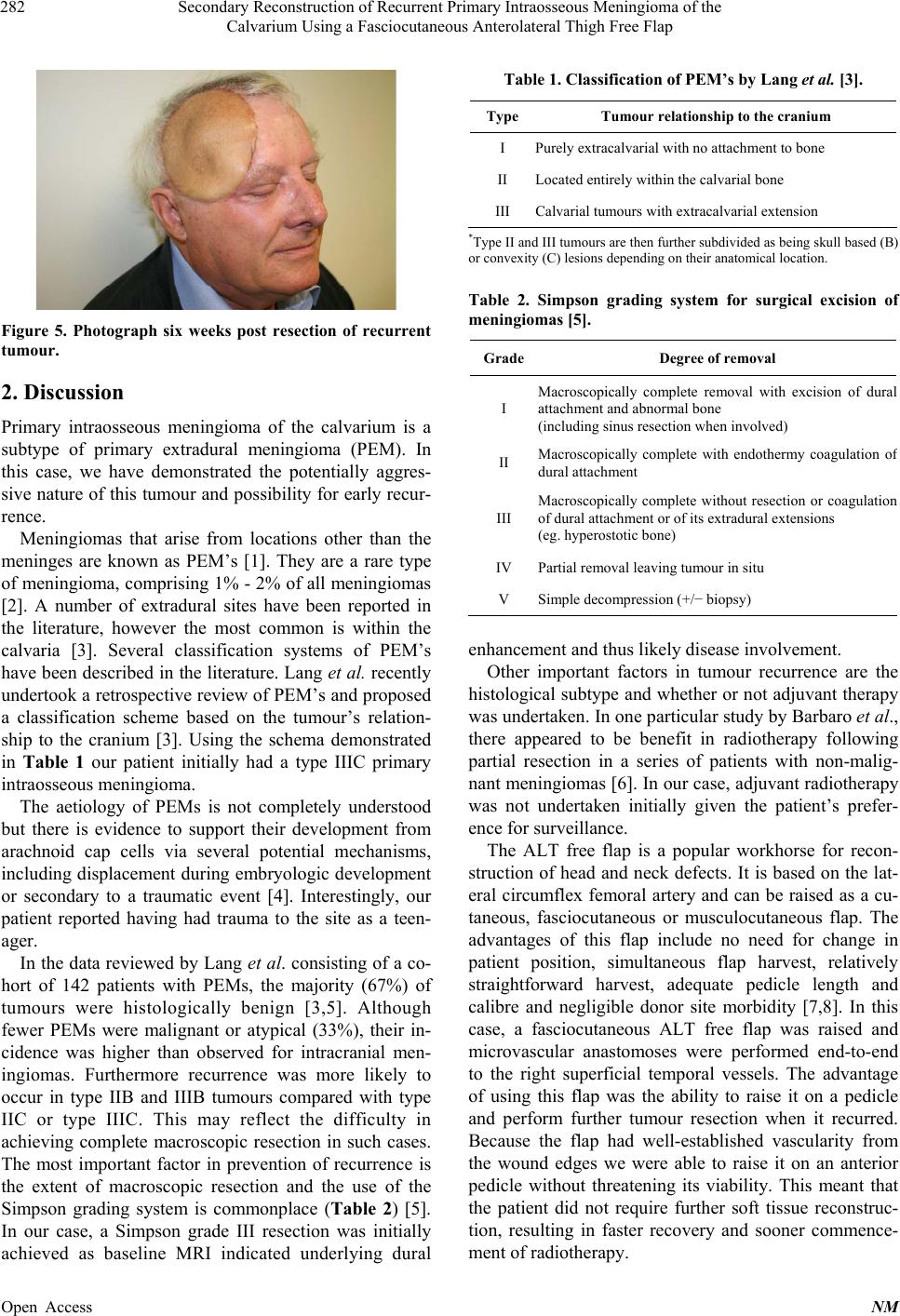
Figure 5. Photograph six weeks post resection of recurrent
tumour.
2. Discussion
Primary intraosseous meningioma of the calvarium is a
subtype of primary extradural meningioma (PEM). In
this case, we have demonstrated the potentially aggres-
sive nature of this tumour and possibility for early recur-
rence.
Meningiomas that arise from locations other than the
meninges are known as PEM’s [1]. They are a rare type
of meningioma, comprising 1% - 2% of all meningiomas
[2]. A number of extradural sites have been reported in
the literature, however the most common is within the
calvaria [3]. Several classification systems of PEM’s
have been described in the literature. Lang et al. recently
undertook a retrospective review of PEM’s and proposed
a classification scheme based on the tumour’s relation-
ship to the cranium [3]. Using the schema demonstrated
in Table 1 our patient initially had a type IIIC primary
intraosseous meningioma.
The aetiology of PEMs is not completely understood
but there is evidence to support their development from
arachnoid cap cells via several potential mechanisms,
including displacement during embryologic development
or secondary to a traumatic event [4]. Interestingly, our
patient reported having had trauma to the site as a teen-
ager.
In the data reviewed by Lang et al. consisting of a co-
hort of 142 patients with PEMs, the majority (67%) of
tumours were histologically benign [3,5]. Although
fewer PEMs were malignant or atypical (33%), their in-
cidence was higher than observed for intracranial men-
ingiomas. Furthermore recurrence was more likely to
occur in type IIB and IIIB tumours compared with type
IIC or type IIIC. This may reflect the difficulty in
achieving complete macroscopic resection in such cases.
The most important factor in prevention of recurrence is
the extent of macroscopic resection and the use of the
Simpson grading system is commonplace (Table 2) [5].
In our case, a Simpson grade III resection was initially
achieved as baseline MRI indicated underlying dural
Table 1. Classification of PEM’s by Lang et al. [3].
Type Tumour relationship to the cranium
I Purely extracalvarial with no attachment to bone
II Located entirely within the calvarial bone
III Calvarial tumours with extracalvarial extension
*Type II and III tumours are then further subdivided as being skull based (B)
or convexity (C) lesions depending on their anatomical location.
Table 2. Simpson grading system for surgical excision of
meningiomas [5].
GradeDegree of removal
I
Macroscopically complete removal with excision of dural
attachment and abnormal bone
(including sinus resection when involved)
II Macroscopically complete with endothermy coagulation o
dural attachment
III
Macroscopically complete without resection or coagulation
of dural attachment or of its extradural extensions
(eg. hyperostotic bone)
IV Partial removal leaving tumour in situ
V Simple decompression (+/− biopsy)
enhancement and thus likely disease involvement.
Other important factors in tumour recurrence are the
histological subtype and whether or not adjuvant therapy
was undertaken. In one particular study by Barbaro et al.,
there appeared to be benefit in radiotherapy following
partial resection in a series of patients with non-malig-
nant meningiomas [6]. In our case, adjuvant radiotherapy
was not undertaken initially given the patient’s prefer-
ence for surveillance.
The ALT free flap is a popular workhorse for recon-
struction of head and neck defects. It is based on the lat-
eral circumflex femoral artery and can be raised as a cu-
taneous, fasciocutaneous or musculocutaneous flap. The
advantages of this flap include no need for change in
patient position, simultaneous flap harvest, relatively
straightforward harvest, adequate pedicle length and
calibre and negligible donor site morbidity [7,8]. In this
case, a fasciocutaneous ALT free flap was raised and
microvascular anastomoses were performed end-to-end
to the right superficial temporal vessels. The advantage
of using this flap was the ability to raise it on a pedicle
and perform further tumour resection when it recurred.
Because the flap had well-established vascularity from
the wound edges we were able to raise it on an anterior
pedicle without threatening its viability. This meant that
the patient did not require further soft tissue reconstruc-
tion, resulting in faster recovery and sooner commence-
ment of radiotherapy.
Open Access NM