Health
Vol.6 No.4(2014), Article ID:43011,9 pages DOI:10.4236/health.2014.64037
Prevalence of Helicobacter pylori and hygiene practices among public secondary school students in Ikeja local government area, Lagos, Nigeria
![]()
Department of Environmental Health Sciences, Faculty of Public Health, College of Medicine, University of Ibadan, Ibadan, Nigeria; *Corresponding Author: mkcsridhar@gmail.com
Copyright © 2014 Sridhar Kameswara Chandra Mynepalli et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. In accordance of the Creative Commons Attribution License all Copyrights © 2014 are reserved for SCIRP and the owner of the intellectual property Sridhar Kameswara Chandra Mynepalli et al. All Copyright © 2014 are guarded by law and by SCIRP as a guardian.
Received 24 November 2013; revised 31 December 2013; accepted 10 January 2014
KEYWORDS
Helicobacter pylori; Hygiene; School Children; Lagos Slums; Hand Washing; Sanitation
ABSTRACT
This study determined prevalence of Helicobacter pylori and hygiene practices among public secondary school students in Ikeja Local Government Area (LGA), Lagos state, Nigeria. An institutional-based, cross-sectional study was conducted among two randomly selected secondary schools. One hundred (100) consented students participated in the study and interviews were conducted using a semi-structured questionnaire while blood samples were collected by venipuncture. Respondents’ ages were 16.1 ± 2.8 years and 54.0% were females. Mean number of persons living in a room was 7.0 ± 3.5, and however, 39.0% of the respondents lived in a room with 4 - 6 persons. The prevalence of H. pylori was 59.0% (59/100). Majority, 64.4% of those infected with H. pylori were 15 years and above while 62.7% females were tested positive to H. pylori. Some, 38.9% of the participants infected with H. pylori drink tap water while 84.7% did hand washing after visiting toilets with water and soap. Mostly, 64.0% of those tested positive to H. pylori did not experience abdominal pain in the last 4 weeks. No significant association existed between drinking water source, hand washing practice after defecation and H. pylori positivity. Routine examination of school students is required to detect Helicobacter pylori in order to commence treatment immediately and awareness about the H. pylori infection should be increased throughout secondary school to prevent further infection.
1. INTRODUCTION
Helicobacter pylori (H. pylori), which was the first formally recognized bacterial carcinogen and one of the most successful human pathogens, has been etiologically associated with gastritis and gastritis associated diseases, peptic ulcer, gastric adenocarcinoma and primary gastric lymphoma [1,2]. The prevalence of infection varies between and within countries in relation with race, ethnicity, and geographical area of the population [3]. Epidemiology of H. pylori infection demonstrated a high prevalence in developing up to 90% than in developed countries [4]. Although, high prevalence is found among the immigrants compared with the local population in the developed countries [5], a low prevalence rate (6.5%) has been reported among school children in Germany [6]. Unless the infection is treated, colonization persists lifelong and has been attributed to the poor socioeconomic status, hygienic practices, and overcrowding in their residences [7,8]. In a study by Haluszki et al. [9], it was reported an increased risk associated with smoking and the ingestion of salted or pickled foods while consumption of uncooked vegetables has also been described as a mode of H. pylori transmission [10]. However, it has been estimated that most infected subjects develop no clinical signs and symptoms of peptic ulceration and continue their lives with superficial chronic gastritis [3]. High percentage (17%) of infected subjects will develop peptic ulcer (4.25%), experience ulcer complications and still fewer (1%) will progress to gastric cancer development of disease depends on bacteria, host and environmental factors [1,11] .
Evidence for its substantial casual role in the pathogenesis of gastric cancer has substantially increased since its isolation in 1982. H. pylori, a gram-negative bacillus that colonizes the stomach is probably the most common chronic bacterial infection worldwide [12]. It has been suggested that communities with a high prevalence of stomach cancer commonly have a high rate of infection with H. pylori infection and decrease in the incidence of gastric cancer and the decreasing rate of the prevalence of H. pylori infection has been observed, especially in the developed countries [13]. Nevertheless, controversial reports, especially from African countries where despite the high rate of H. pylori infection, gastric cancer has a very low prevalence, make it hard to conclude on the significant role of H. pylori infection on the incidence and prognosis of gastric cancers [14]. However, a prospective cohort study among Japanese patients with noncancerous gastric and duodenal pathological conditions demonstrated that patients who were positive for H. pylori infection in the study initiation were significantly more likely to develop gastric cancers [15].
Most studies attributed sociodemographic factors to the H. pylori positivity. For instance, Barik [11] reported that 80% of adult population was infected with H. Pylori in developing countries with age being the strongest risk factor. Also, it was found that H. Pylori positivity had a strong association with age > 40 years in Yemen [16]. Similarly, Ito, et al. [17] indicated that males were at significant risk for the infection of H. pylori while Replogle et al. [18] noted that the infection risk was the same for males and females. In Nigeria, however, among the few studies that investigated H. pylori infection attributed it to environmental factors such as hygiene practices and diet [19]. Despite the fact that environmental factors such as water sources, housing conditions, hygiene practices have roles to play in its infection, there is dearth of information on the available literature on these factors. Therefore, this study determined prevalence of H. pylori and hygiene practices among public secondary school students in Ikeja LGA, Lagos state, Nigeria.
2. MATERIALS AND METHODS
2.1. Study Area
Lagos metropolis is situated between Lat. (6 22' and 6 42') N and Long. (42' and 4 22') E, and comprises of 20 Local Government Areas, namely—Agege, Ajeromi/Ifelodun, Alimosho, Amuwo-Odofin, Apapa, Badagry, Epe, Eti-Osa, Ibeju-Lekki, Ifako-Ijaiye, Ikeja, Ikorodu, Kosofe, LagosIsland, LagosMain-land, Mushin, Ojo, Oshodi/Isolo, Somolu and Surulere. It is located in the tropical rain forest zone of the country and climate oscillates between a dry season (November to April) and a wet season May to October). Ikeja LGA, the study area is situated between Lat. (53000 and 54000) N and Long. (72000 and 73000) E, with an estimated total population of 313,196 (males: 169, 233 and females: 143,963) [20]. The LGA is made up of 12 settlements namely; Aguda, Omole, Agidingbi, Ikeja (Central), Ogba, Ikeja G.R.A, Maryland, Onigbongbo, Ojodu, part of Ilupeju, Onileke and Opebi. There are 13 public secondary schools, 16 private secondary schools and two military secondary schools, giving a total of 28 secondary schools, all distributed among the 12 major settlements in the L.G.A (Ministry of Education, Planning, Research and Statistics Division, The Secretariat, Alausa, Ikeja, Nigeria, Personal communication).
2.2. Study Design and Study Location
This study was an institutional-based, cross-sectional and involved secondary school students in Ikeja LGA, Lagos state. Respondents were selected by simple random sampling. A set of semi-structured questionnaire was developed to elicit information such as demographic characteristics of students, source of drinking water, sanitary practices and perceived health problems of respondents. Also, blood samples from selected students were collected, tested for Immunoglobulin antibodies against H. pylori by ELISA (manufactured by Organics and marketed by May and Baker pharmaceuticals Nigeria Ltd).
2.3. Study Population and Sampling Techniques
This study was carried out among public secondary school students. Two schools were selected from the 13 public secondary schools by simple random sampling. One hundred (100) consented students of these two secondary schools participated in the study. During the planning of the study, the researchers approached the authorities in-charge of the selected schools particularly the principals and the Local Education District Officer in-charge of public schools with formal letters to obtain permission to carry out the work in the schools and also explained the study objectives. Furthermore, a lecture on the theme and objectives of the study was given at one of the “Parents Teachers Association” (PTA) meetings ensuring that they understood all aspects of the study. Permission and supervision were granted over the collection of blood samples from students in the school by health officials from Ministry of Health sought by Ministry of Education. Consent forms after they had been completed and signed, were obtained from parents/guardians, heads of schools and the students. Parents, who accepted their children to be included in the study, presented them at the time of blood sampling by one of the authors who is qualified.
Simple random sampling technique was used to represent a proportional distribution from the various arms of classes. Each arm of class was given an equal chance of being selected. Selection of the various arms was made by balloting. For example, in the different arms of JS 1, about 6 - 8 arms in both the schools, were assigned numbers on a small piece of paper each; these were dropped into a big bowl; thoroughly mixed and a class captain was asked to pick a piece of paper. Consenting students in the class(es) selected were interviewed while blood samples were collected immediately after the interview from the respondents. Interviews were conducted by two trained research assistants (one male and one female) who are university graduates and were acquainted with questionnaire research. They were trained in how to use the instrument and how they should introduce themselves and the research objectives modestly to the students during the interview.
2.4. Laboratory Analysis
Blood samples (3 - 5 ml) were collected from each student by venipuncture, into 5ml clean plain vial containing no anticoagulant. Samples were taken to the laboratory where they were allowed to stand for 20 min for blood to clot before centrifuged. Supernatant serum was separated and transferred into another clean test tube and corked. Specimens were stored at –20˚C till they were ready to be assayed.
The ImmunoComb II H. pylori IgG kit was used for the quantitative determination of IgG to Hp in serum. It consists of an indirect solid-phase EIA. The solid phase is a comb with 12 projections (“teeth”). Each tooth is sensitized at two positions: Upper spot—goat antibodies to human immunoglobulin (internal control). Lower spot—antigens of inactivated H. pylori. The developing plate has 6 rows (A - F) of 12 wells, each row containing a reagent solution ready for use at a different step in the assay. The test was performed stepwise, moving the comb from row to row, with incubation at each step. At the onset of the test, serum specimens were pre-diluted 1 in 11 and added to the diluent in the wells of row A of the developing plate. The comb is then inserted into the wells of row A antibodies to Hp if present in the specimen, will specifically bind to Hp antigens in the lower spot on the teeth of the comb. Simultaneously, immunoglobulin present in the specimens was captured by the anti-human immunoglobulin on the upper spot (internal control).
Unbound components were washed away in row B. in row C, the anti-Hp IgG captured on the teeth will react with anti-human IgG labeled alkaline phosphatase (AP). In the next two rows, unbound components are removed by washing (i.e. rows D and E) in row F, the bound alkaline phosphatase reacts with chromogenic components. The results were visible as gray-blue spots on the surface of the teeth of the comb. The test kit includes a positive control (anti-Hp IgG) and a negative control which were included in each assay run. Upon completion of the test, the tooth used with the positive control should show two gray-blue spots. The tooth used with negative control should show upper spot and either no spot or a faint lower spot. The upper spot should also appear on all other teeth, to confirm that the specimen was added.
2.5. Data Analysis
Data generated from the field were edited daily. Then they were coded and entered into the computer for analyses using Epi-Info 6.04 statistical software packaged. Data were presented as mean standard deviation for continuous variables and percentages for categorical variable. Chi-square statistic was used to determine the associations between demographic characteristics, housing conditions, drinking water sources, hygiene practices and H. pylori positivity among the students. Statistical significance was defined at p < 0.05.
2.6. Ethical Considerations
The study was approved by the joint Ethical committee of University of Ibadan and University College Hospital, Ibadan, Nigeria and consent was obtained from selected schools principals and the respondents, the Local Education District Officer in-charge of public schools and Parents’ Teacher’s Association of the selected school.
3. RESULTS
3.1. Demographic Characteristics of the Participants
Table 1 presents the demographic profile of the participants. The mean age which ranged from 9 - 19 years was 16.1 ± 2.8 years. There were (54.0%) female and (46.0%) male. Most (82.0%) were Christians while 16.0% practice Islam. Most of the participants’ father (94.0%) and mother (90.0%) had completed secondary education. Majority (60.0%) lived in flat type apartment as depicted in Figure 1. Mean number of persons living in a room was 7.0 ± 3.5 (rang = 1 - 15) while 39.0% of those who lived in a room were between 4 - 6 persons as illustrated in Figure 2.
3.2. Prevalence of H. pylori Infection
The H. pylori positivity ratio was found to be 59.0% (59/100) as shown in Figure 3. Majority (64.4%) of participants, aged 15 years and above) were infected with H.
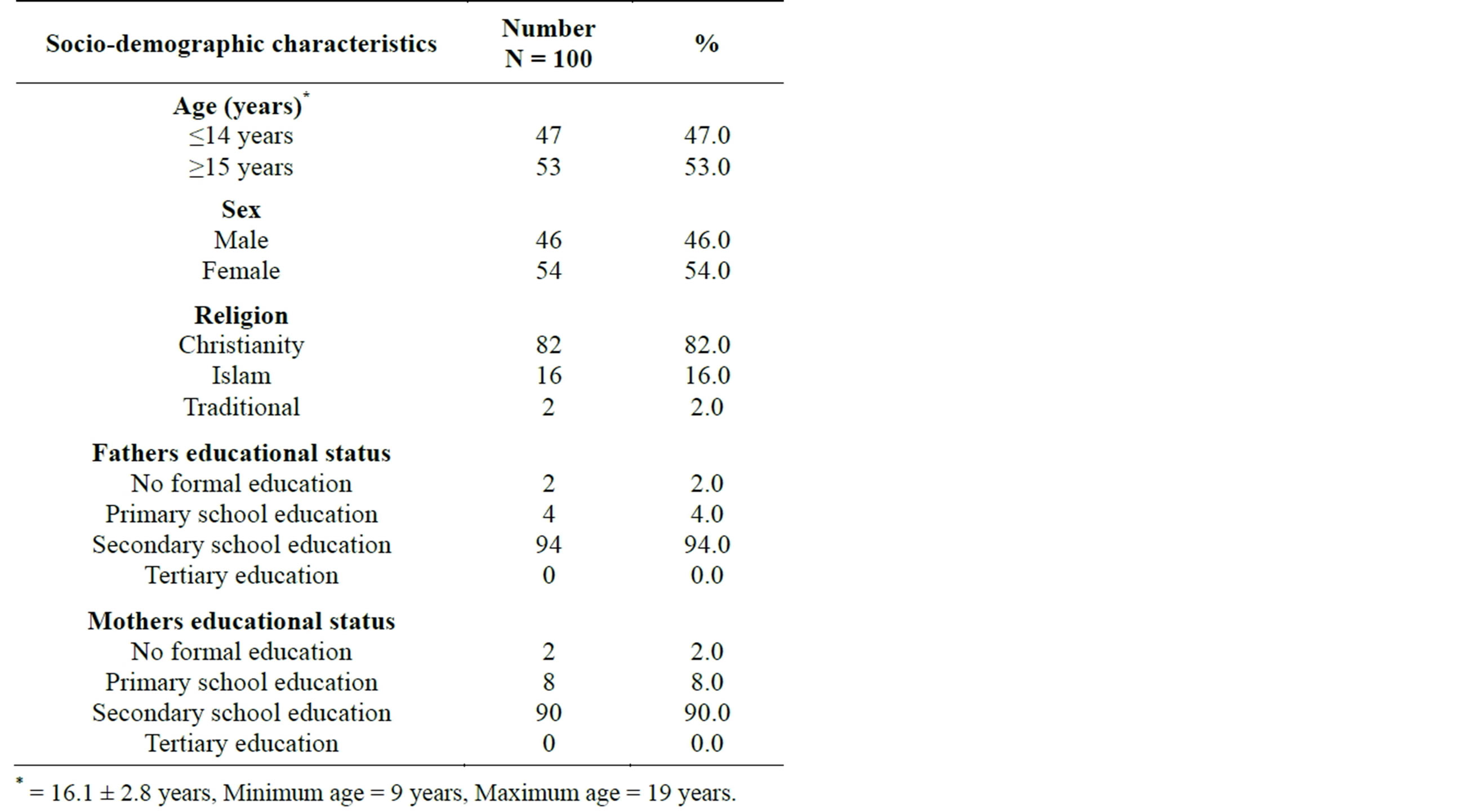
Table 1. Socio-demographic characteristics.
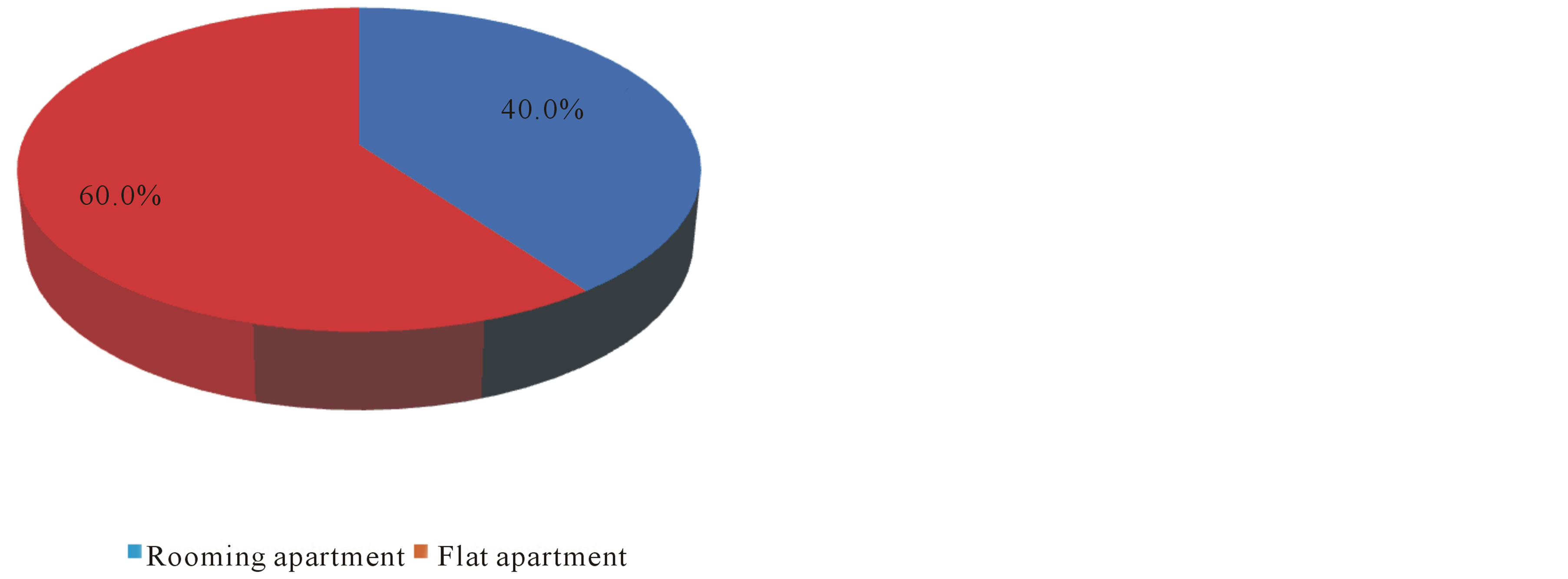
Figure 1. Type of house apartment used among participants.

Figure 2. Number of persons living in a room. Mean ± SD = 7.0 ± 3.5, Minimum = 1, Maximum = 15.

Figure 3. Positivity of Helicobacter pylori among students.
pylori compared to 35.6% of those who were under 14 years old with no significant difference. More females (62.7%) were tested positive to H. pylori infection compared to 37.3% of their male colleagues with no significant difference. Respondents’ father and mothers educational qualification did not show any significant difference on the positivity of H. pylori infection as presented in Table 2.
3.3. Effect of Housing Condition, Sources of Drinking Water and Hygiene Practices on H. pylori Positivity
Table 3 presents the housing condition of the participants. It was revealed that slightly more than half (52.5%) of those infected with H. pylori lived in flat apartment compared to those who were living in rooming apartment with no significant difference. Also, 50.8% of the students reported that 4 - 6 persons were sleeping in a room, this proportion were tested positive of H. pylori. Association between number of person living in a room and H. pylori positivity was not statistically significant. About half (50.8%) of students living in poorly ventilated room H. pylori positive compared to those who lived in well ventilated room, this was not statistically significant (p > 0.05).
Sources of drinking water and hygiene practices of the participants are shown in Table 4. Equal proportion (38.9%) of those infected with H. pylori drank boiled and tap water respectively while boiled (36.6%) and filtered (31.7%) water were the main sources for drinking for those who were negative to H. pylori test. No significant association existed between respondent sources of water and H. pylori positivity. Majority (83.1%) of those positive for H. pylori used water only for cleaning-up after defecation while 68.3% of those with negative H. pylori
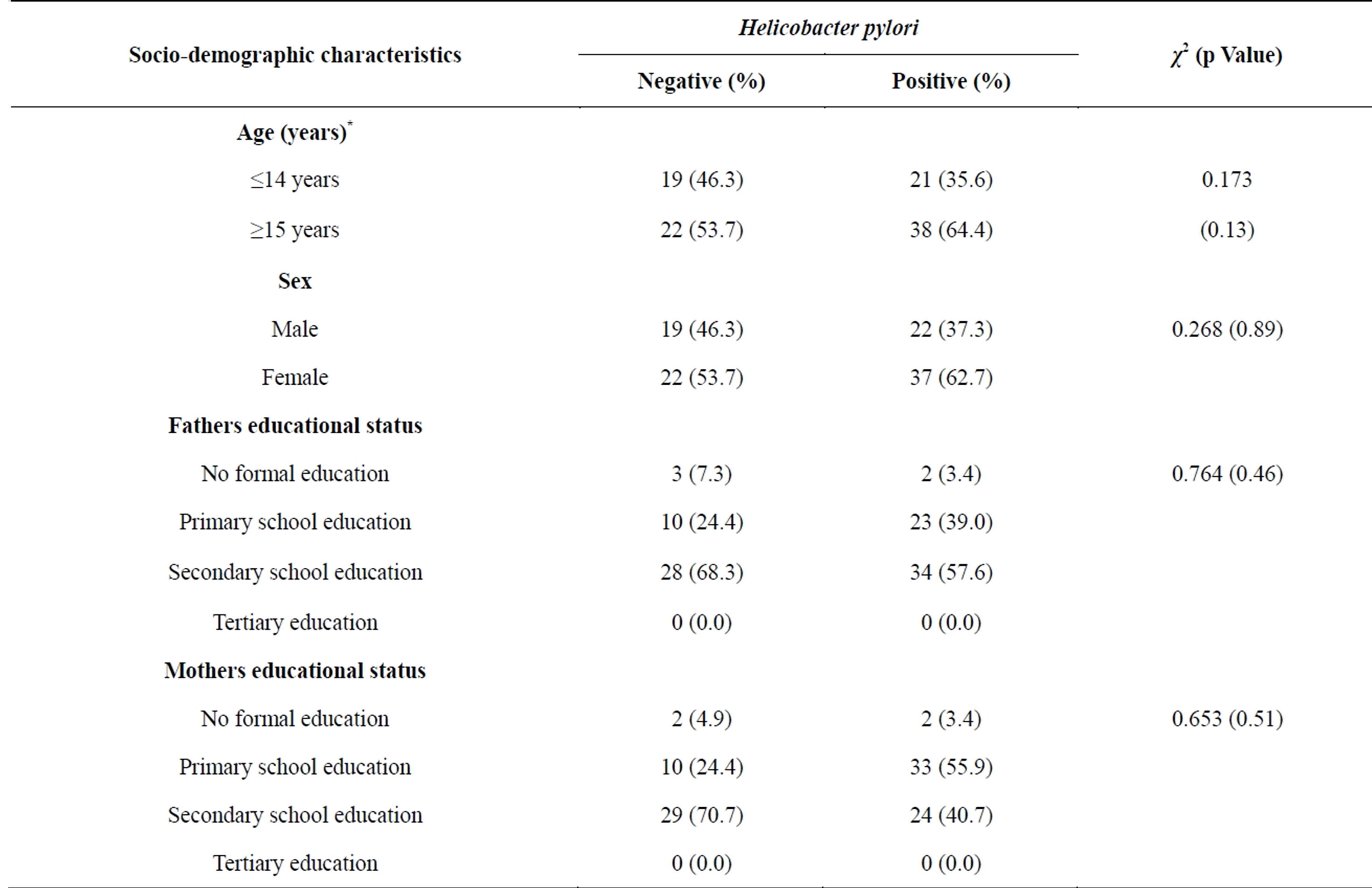
Table 2. Comparison of socio-demographic characteristics and Helicobacter pylori positivity.

Table 3. Housing condition and H. pylori positivity.
used same with no significant difference. High proportion (84.7%) of students who had H. pylori and 92.7% who were tested negative practiced hand washing after defecation with water and soap, this was not statistically significant. About 72.9% of those who were positive to H. pylori test and 75.6% of those tested negative practiced hand washing everyday while 8.5% did not do so among those who were H. pylori positive. Association between frequency of hand washing after defecation and H. pylori positive.
3.4. H. pylori Infection and Perceived Symptoms
H. pylori infection and perceived symptoms were compared as shown in Table 5. There was no significant association between experience of pain in the upper abdomen in the previous 4 weeks and H. pylori positivity. About similar proportion, 57.6% of those tested positive and 56.1% who were tested negative did not experience pain in the upper abdomen in the previous 4 weeks. Moreover, among those who experienced pain in the upper abdomen in the previous 4 weeks, 64.0% of those tested positive and 66.7% of those who were negative did not do so frequently (p > 0.05).
4. DISCUSSION
This study documents the prevalence of H. pylori among public secondary school students in Ikeja Local Government, Lagos state, Nigeria. Data from this study revealed the H. pylori positivity ratio of 59.0% (59/100). This finding is similar to Tayfun, et al. [21] in a study conducted among students detected H. pylori positivity at quite a high rate (63%). However, Özden, et al., [22] had emphasized that H. pylori positivity ratio has been

Table 4. Sources of drinking water, hygiene practices and H. pylori positivity.
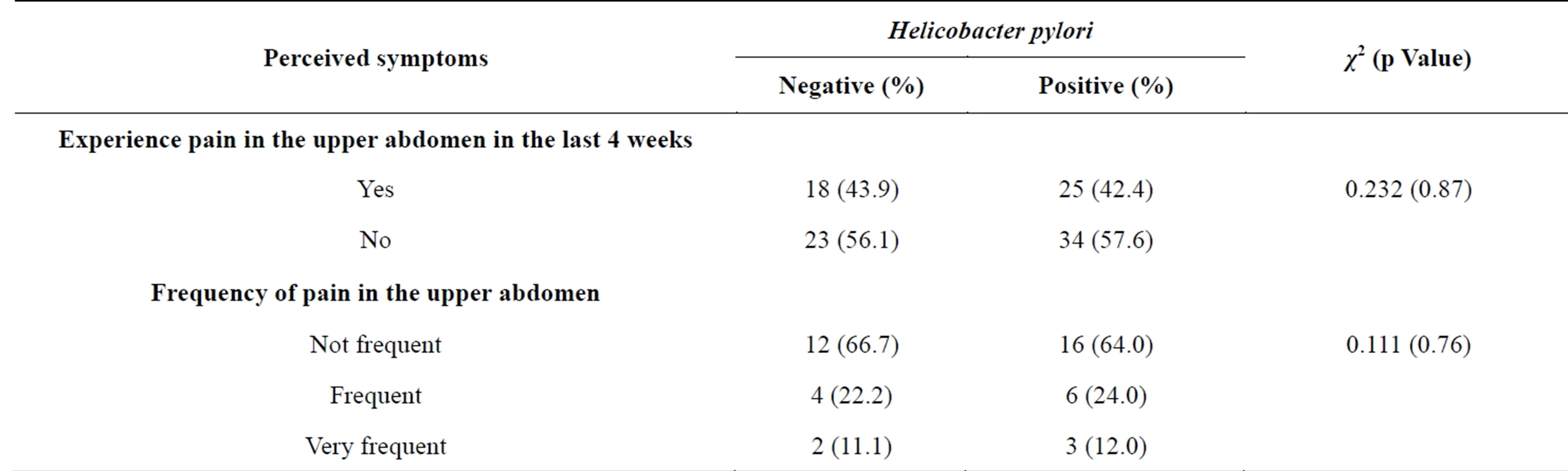
Table 5. Comparison of H. pylori infection and perceived symptoms.
decreasing over the years. Previous study has documented the distribution of H. pylori (+) frequency according to age groups to be: 96% in the 7 - 12 age group; 83% in the 13 - 18 age group; 75% in the 19 - 24 age group; 96% in the 25 - 29 age group; 91% in the 30 - 34 age group; 83% in the 35 - 39 age group; and 94% in the 40 - 65 age group [23]. This study revealed that high proportion of participants (15 years and above) were infected with H. pylori compared to 35.6% of those who were less or equal to 14 years old with no significant difference. Also, our findings concur with Özden et al. [22] who noted a high proportion (78.5%) of H. pylori (+) cases in their studies and did not find a significant difference between age groups and gender distributions.
Moreover, in a study by Ito, et al., [15] indicated that males are at significant risk for the infection of H. pylori while Replogle et al., [18] noted that the infection risk is the same for males and females. This study found that, although not significantly difference, large percentage of female were tested positive to H. pylori infection compared to 37.3% of their male colleagues. Students father and mothers educational qualification did not show any significant difference on the positivity of H. pylori infection. This is an indication that respondents fathers and mothers educational status had no influence on the H. pylori positivity of their children. Data on the housing condition of the participants revealed that slightly more than half (52.5%) of those infected with H. pylori lived in flat apartment compared to those who were living in rooming apartment with no significant difference. These findings evidently show that living in either rooming or flat apartment has no influence on the positivity of H. pylori among the study participants. Barik [11] noted that in developing countries, overcrowded conditions that create closer contacts between mothers and children and between siblings sharing the same bed might be the main reason for the high infection rates reported. It was stressed further that spouse-to-spouse transmission has also a major role for H. pylori infection and continuous contact is required for the establishment of such infection. In this study however, 50.8%of the students reported that between 4 - 6 persons were sleeping in a room, this proportion was tested positive of H. pylori. Also, no significant association existed between 4 - 6 persons sleeping in a room and H. pylori positivity. This shows that 4 - 6 person living in a room did not translate into H. pylori positivity.
Information on the sources of drinking water revealed that several proportion of those infected with H. pylori drink tap water. This is similar to the findings of Alemayehu [3], that few participants use water source other than pipe and practice hand washing without soap and observed no significant association between these variables and H. pylori positivity. It was emphasized that it might be as a result of increased awareness about hygienic practices and environmental health conditions through health extension program throughout the country. Large percentage of those tested positive of H. pylori used water only for clean-up after defecation. This is an indication that high level of hygiene s being maintained by those tested with positive of H. pylori. Infection with H. pylori has been attributed to environmental factors such as hygiene practices and diet which may play key role in the acquisition of infection and the expression of clinical disease [19]. This study found that most of students who had H. pylori and 92.7% who were tested negative did hand washing after defecation with water and soap. This is an evident that the study population were aware of the menace caused by inadequate hygiene practices especially poor hand washing practice after visiting toilet [24]. noted that the initial acquisition of H. pylori infection causes acute gastritis with hypochlorhydria which may cause abdominal pain, nausea and vomiting that resolve within a few days. In this study, no significant association between experience of pain in the upper abdomen in the last 4 weeks and H. pylori positivity was observed. In addition, large proportion of participants who were tested positive of H. pylori infection did not experience pain in the upper abdomen in the last 4 weeks.
5. CONCLUSION
Prevalence of Helicobacter pylori and related environmental factors among public secondary school students in Ikeja Local Government Area, Lagos has been determined and Helicobacter pylori positivity is high among the participants. High proportion of the participants drink tap water, practice hand washing after visiting toilets and no association existed between water sources, hand washing after visiting toilet, number of person living in a room and Helicobacter pylori positivity. Also, most of the study participants who were tested positive to Helicobacter pylori did not experience abdominal pain in the last 4 weeks. Although, no environmental factor is associated with H. pylori positivity, routine examination of school students is required to detect Helicobacter pylori in order to commence treatment immediately. In addition, awareness about the menace which might occur from H. pylori infection through health extension program should be increased throughout secondary school. This will prevent occurrence of this infection among secondary school students.
6. LIMITATIONS
It was initially planned to include students from private secondary schools in this study but authorities from the private school refused their students to participate in subjecting themselves to blood collection. Hence it was not possible to collect blood samples from the private school students regardless of showing the ethical clearance to the school authority. Also, despite having obtained approval from Ministry of Education, some parents in the public school held to certain superstitious beliefs about blood, refused signing consent forms and thus not allowing their children/wards to take part in the study. More so, cost of commercial kits was expensive.
ACKNOWLEDGEMENT
The Authors acknowledge the immense contribution of the Principals of the schools under study.
REFERENCES
- Johannes, G., Arnoud, H. and Ernst, J. (2006) Pathogenesis of Helicobacter pylori Infection. Journal of Clinical Microbiology, 19, 449-490.
- Nurgalieva, Z., Malaty, H., Graham, D., Almuchambetova, R., Machmudova, A., Kapsultanova, D., Osato, M., Hollinger, F. and Zhangabylov, A. (2002) Helicobacter pylori infection in Kazakhstan: Effect of water source and household hygiene. American Journal of Tropical Medicine, 67, 201-206.
- Alemayehu, A. (2011) Seroprevalence of Helicobacter pylori infection and its risk factors among adult patients with dyspepsia in hawassa teaching and referral hospital, south ethiopia. MSc Thesis, Addis Ababa University, Addis Ababa, 1-37.
- Perez-Perez, G.I., Rothenbacheri, D. and Brenner, H. (2004) Epidemiology of Helicobacter pylori infection. Helicobacter, 9, 1-6. http://dx.doi.org/10.1111/j.1083-4389.2004.00248.x
- Roma-Giannikou, E. and Shcherbakov, P.L. (2002) Helicobacter pylori infection in pediatrics. Helicobacter, 7, 50-55. http://dx.doi.org/10.1046/j.1523-5378.7.s1.8.x
- Herbarth, O., Krumbiegel, P., Fritz, G.J., Richter, M., Schlink, U. and Muller, D.M. (2001) Helicobacter pylori prevalence and risk factors among school beginners in a German urban center and its rural county. Environ Health Perspect, 109, 573-577. http://dx.doi.org/10.1289/ehp.01109573
- Amini, M., Karbasi, A. and Khedmat, H. (2009) Evaluation of eating habits in dyspeptic patients with or without Helicobacter pylori infection. Journal of Tropical Gastroenterology, 30,142-144.
- Asrat, D., Nilsson, I., Mengistu, Y., Ashenafi, S., Ayenew, K., Abu Al-Soud, W, Wadstrom, T. and Kassa, E. (2004) Prevalence of Helicobacter pylori infection among adult dyspeptic patients in Ethiopia. Annals of Tropical Medicine Parasitology, 98, 181-189. http://dx.doi.org/10.1179/000349804225003190
- Haluszki, O., Tokar, J.L. and Greenwald, B.D. (2000) Stomach-stomach cancer. Current Problems in Cancer: Endoscopic Oncology, 29, 33-112.
- Hopkins, R.J., Vial, P.A., Ferreccio, C., Ovalle, J., Prado, P. and Sotomayor, V. (1999) Seroprevalence of Helicobacter pylori in Chile: Vegetables may serve as one route of transmission. Journal of Infectious Disease, 168, 222- 226. http://dx.doi.org/10.1093/infdis/168.1.222
- Barik, A.S. (2009) Helicobacter pylori infection in developing countries: The burden for how long? Saudi Journal of Gastroenterology, 15, 201-207. http://dx.doi.org/10.4103/1319-3767.54743
- Crew, K.D. and Neugut, A.I. (2006) Epidemiology of gastric cancer. World Journal of Gastroenterology, 12, 354-362.
- Parsonnet, J. (1995) The incidence of Helicobacter pylori infection. Alimentary Pharmacology & Therapeutics, 9, 45-51.
- Muñoz, N. and Pisani, P. (1994) Helicobacter pylori and gastric cancer. European Journal of Gastroenterology & Hepatology, 6, 1097-1103. http://dx.doi.org/10.1097/00042737-199412000-00005
- Uemura, N., Okamoto, S. and Yamamoto, S. (2001) Helicobacter pylori infection and the development of gastric cancer. The New England Journal of Medicine, 345, 784- 789. http://dx.doi.org/10.1056/NEJMoa001999
- Gunaid, A.A., Hassan, N.A. and Murray-Lyon, I. (2003) Prevalence and risk factors of Helicobacter pylori infection among Yemeni dyspeptic patients. Saudi Medical Journal, 24, 512-517.
- Ito, L.C., Oba-Shinjo, S.M. and Marie, S.K.N. (2003) Lifestyle factors associated with atrophic gastritis among Helicobacter pylori seropositive Japanese-Brazilians in São Paulo. International Journal of Clinical Oncology, 8, 362- 368. http://dx.doi.org/10.1007/s10147-003-0355-3
- Replogle, M.L., Glaser, S.L. and Hiatt, R.A. (1995) Biologic sex as a risk factor for Helicobacter pylori infection in healthy young adults. American Journal of Epidemiology, 142, 856-863.
- Linda, M.B. (2000) Helicobacter pylori: Epidemiology and routes of transmission. Epidemiologic Reviews, 22. http://epirev.oxfordjournals.org
- Federal Republic of Nigeria (2009) Legal notice on publication of 2006 census final results Official Gazette, 96, B1-42. http://placng.org/Legal%20Notice%20on%20Publication%20of%202006%20Census%20Final%20Results.pdf
- Yücel, T., Aygin1, D., Sen, S. and Yücel, O. (2008) The prevalence of Helicobacter pylori and related factors among university students in Turkey. Japanese Journal of Infectious Diseases, 61, 179-183.
- Özden, A., Bozdayı, G. and Özkan, M. (2004) Changes in the sero-epidemiological pattern of Helicobacter pylori infection over the last 10 years in Turkey. Turkish Journal of Gastroenterology, 15, 156-158.
- Brown, L.M., Thomas, T.L. and Ma, J.L. (2002) Helicobacter pylori infection in rural China: Demographic, lifestyle and environmental factors. International Journal of Epidemiology, 31, 638-645. http://dx.doi.org/10.1093/ije/31.3.638
- Shmuely, H., Obure, S., Passaro, D., Abuksis, G., Yahav, J. and Fraser, G. (2003) Association between dyspeptic symptoms and Helicobacter pylori infection in Nakuru, Kenya. Journal of Emerging Infectious Disease, l9, 020374.

