World Journal of AIDS
Vol.4 No.2(2014), Article
ID:46770,9
pages
DOI:10.4236/wja.2014.42018
Influence of Customized Demand Generation as a Strategy to Increase Uptake of Voluntary Counseling and Testing Services amongst Sex Workers in Mumbai and Thane
Samita Bhardwaj1*#, Sowmya Ramesh2*, Sanjeevsingh Gaikwad1*
1FHI 360, Mumbai, India
2Population Council, India Habitat Centre, New Delhi, India
Email: #sbhardwaj@fhi360.org, sramesh@popcouncil.org, sgaikwad@fhi360.org
Copyright © 2014 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/



Received 15 April 2014; revised 15 May 2014; accepted 25 May 2014
ABSTRACT
Background: To demonstrate that customized demand generation leads to increased voluntary HIV counseling and testing (VCT) among Sex Workers (SWs). Methods: FHI 360 Aastha implemented Vivek intervention among SWs in Mumbai and Thane, India using customized demand generation through outreach services for VCT. Program monitoring data and integrated counseling and testing center tracking sheets were used to assess the intervention effect. Results: Higher proportion of registered SWs tested during: 1) Vivek months than other months (17% vs. 5%, p < 0.001); 2) Post-initiation non-Vivek months than pre-Vivek months (4.7%, vs. 1.5% p < 0.001). Conclusions: Customized demand generation approach is successful in increasing HIV testing.
Keywords:HIV Prevention, VCT, SWs, Customized Demand Generation, Outreach Operationalization

1. Background
In India, about 2.5 million people, aged between 15 and 49, are estimated to be living with HIV, making it the country with the third largest number of infected people in the world. Most HIV infections in India occur through heterosexual transmission [1] . Specific HIV prevalence rates within various populations in India show disproportionately higher incidence of the infection among Most at risk populations (MARPs), particularly female sex workers (FSWs); men who have sex with men (MSM) and injecting drug users (IDUs). HIV Sentinel Surveillance data (2010-2011) indicates that 7.1% of IDU, 4.4% of MSM and 2.7% of FSW are HIV positive, while the prevalence among ANC clinic attendees, considered proxy for general population, is low at 0.40% [2] . To gain control over the spread of HIV in the country, effective interventions are needed for these MARPs [1] . Scaling-up of Voluntary Counseling and Testing (VCT) for HIV has been one of the key interventions for reducing this epidemic [3] . However, NACO estimates that only 50% of those currently infected with HIV are aware of their status and therefore there is still significant work to be done in this area [4] .
Voluntary counselling and testing helps decrease HIV transmission since delivery of prevention messages is an integral part of VCT services and if found positive, this can lead to timely linkages to care and treatment with the added benefit of decreasing onward transmission. Also, knowing the HIV status is the first step in the care, support and treatment cascade.
Early HIV infection detection is also potentially very important because this disease stage, although constituting only a brief period in the natural history of HIV (generally defined as about the first 6 months after infection), has a disproportionate effect on disease spread because it is characterized by a high viral load and thus a high per-contact transmission risk [5] . Thus early diagnosis is critical for HIV prevention and wider VCT roll-out is needed to ensure that PLHIV stay healthy and access the care they need by timely knowledge of their HIV status. Timely initiation of ART could reduce HIV transmission, especially in the asymptomatic period. Further, several studies have demonstrated that voluntary counselling and testing is associated with the adoption of safer sexual behaviours [6] -[11] . Despite the recognized benefits of HIV testing in prevention, care and treatment, global experiences suggest comparatively lower uptake of VCT amongst MARPs [9] .
Since 2004, FHI 360 has been implementing Aastha, a Bill & Melinda Gates Foundation supported HIV/STI prevention project for sex workers in two districts, viz., Mumbai and Thane in the state of Maharashtra, India. Clinics established in Aastha NGOs provide a complete package of services including STI prevention and management, condom distribution, syphilis screening, voluntary HIV counseling and testing, strategic behavior counseling and peer-led community mobilization services. In March 2009, Integrated Counseling and Testing Centers (ICTCs) were set up in the project clinics in collaboration with National AIDS Control Organization (NACO) as a Public Private Partnership Initiative.
Despite the widespread availability of VCT tests through project-supported static clinics in Mumbai and Thane districts and recommendations for regular screening, project-monitoring data indicated that only 1.5% of SWs in the project catchment areas accepted routine VCT in the static clinics from the time it was opened in project clinics over a period of 10 months.
Studies have enumerated several individual level and contextual factors that influence the decision to undergo HIV testing [6] [9] [12] -[16] . Traditional VCT-related barriers, such as low perceived risk for HIV infection [6] , lack of access to free testing [15] , general negative perception of test services, stigmatizing beliefs coupled with fear of discrimination if diagnosed as HIV-positive [14] , shortage of counselors and their competency, concerns about confidentiality and delays in returning HIV test results [6] [17] continue to hamper effective access to and uptake of VCT in many countries. In addition, heterogeneous typologies based on the solicitation sites, workplace, gender, language, culture and controlled by stakeholders such as brothel owners, madams and pimps, restricted service hours of the facilities, distance of the counseling and testing centers and stigma and discrimination faced by SWs from service providers further contribute to the low uptake rate of HIV testing among HRGs [18] . Addressing some of these barriers could greatly improve HIV testing uptake among HRGs. To counter these barriers to access and uptake, an approach named Vivek (conscience) was implemented by FHI 360 Aastha to increase early and regular uptake of counseling and testing for HIV.
In this paper, we describe and demonstrate that customized demand generation strategies through outreach operationalization of voluntary counseling and testing services for HIV lead to improved access and increased uptake of HIV testing among Sex Workers (SWs).
2. Methods
2.1. Procedure/Intervention
Vivek was an intensification of voluntary counseling and testing services for a period of one month operationalized in outreach settings for male and female sex workers. It is a synchronization of demand generation through strategic behavior change communication and improvement of access through outreach activities. Vivek intervention was conducted during 4 different timelines including the months of January 2010 (Vivek 1), July 2010 (Vivek 2), December 2010 (Vivek 3) and June 2011 (Vivek 4).
Vivek was a unique strategy as it was customized to each typology based on specific barriers to that particular group. It addressed those barriers which included optimum timings and location for implementing the strategy that led to improved access to VCT services.
The flow of events which was followed during implementation of Vivek was as follows:
1) SBC and Outreach activities: Outreach clinics were preceded by intensive Strategic behavioral Communication (SBC) activities such as 1-1 communication to motivate and create demand amongst SWs for VCT. SBC included use of interactive communication materials with the MARPs to increase awareness for regular testing and generate demand. Community engagement was a key component of Vivek’s strategic planning for HIV services which included sensitization of the stakeholders on the significance of counseling and testing for HIV. Communities took a lead in organizing these outreach clinics which were conducted in bars, homes and brothels at convenient times.
Outreach planning included the presence of an outreach team comprised of a Peer Educator (PE), outreach worker (ORW) and community volunteers (CVs) of the site/s. The outreach team used SBC materials, to help in demand generation for HIV testing. Planning operations included updated line listing which enumerates the number of SWs who are active and available for program services in an area and updated individual tracking sheet which provides information on the SWs HIV testing status. All micro sites had peer presence, updated estimate of active population in each micro site, suitable date, time and location for sex worker of each micro site. A micro site is defined as a concise geographical area that has around 50 - 60 enumerated SWs to which is assigned one Peer Educator (PE).
2) Activities at the clinics (pretest, testing, post test, referral): Clinical planning included presence of a trained clinic team comprising of a doctor, nurse, counselor and a laboratory technician. Logistic requirements included uninterrupted supply of HIV testing kits, gloves, needles and syringes, vacutainers and micro tips. The flow of events at clinic was:
a) pre-test counseling and informed consent; b) testing; c) post-test counselling; and d) referral to Care and Support services. All identified PLHIV SWs were linked systematically with government care and treatment services while those tested negative are provided post test counseling and advised for 6 monthly re-testing.
3) QA activities and monitoring: The ICTCs were capacitated with infrastructure, training and the introduction of monitoring tools such as the EQAS (external quality monitoring) and other internal reporting formats such as daily monitoring sheet. The EQAS and other internal quality improvement tools helped to maintain quality during the Vivek campaign. A quality assurance mechanism for Vivek at every level was facilitated through monitoring, improving and training staff members.
The difference between Vivek and non-Vivek periods was the strong coordination mechanism and synchronisation between clinical planning and outreach efforts. Figure 1 provides a conceptual framework of typology specific VCT services.
Brothel based sex workers reside and solicit clients from a fixed place (brothels). Control by the stakeholders such as brothel owners, madams and pimps posed a challenge for SWs in accessing VCT services. Vivek ensured that sensitization with the key stakeholders is conducted at various forums and levels. The outreach team organized suitable infrastructure for HIV counseling and testing in a nearby room in a brothel for VCT services. Appropriate SBC activities for this typology focused on being healthy for ensuring better life for SW’s children, and on being financially secure and hope for a better life.
Bar girls operate from bars and solicit clients either at their work or through pimps. In order to make VCT services accessible to bar girls, the outreach team organized suitable infrastructure for HIV counseling and testing in bar settings. VCT services were made available at green rooms (places where bar girls dress up; changing room/dressing room) inside the bars with audio-visual privacy with prior permissions from the bar managers. Appropriate SBC activities for this typology focused on “beauty as a hook” which essentially provides beauty tips for bar girls and emphasizes the need of staying healthy as a means of staying beautiful which is an important need of the bar girls.
Street based sex workers or floating SWs can be found throughout the districts. Preferred locations are railway and bus stations, main roads, highways, beaches, near the red light areas. These women are extremely mobile, moving from one hotspot to another in search of clients. Since they are available largely on the streets, pro-

Figure 1. Conceptual framework of typology specific VCT services. BB: Brothel based SWs; SB: Street based SWs; HB: Home based SWs; MSW: Male sex worker; BG: Bar girls.
vision of VCT services were made either at a nearby location where privacy was possible (local doctor’s clinic, sex worker’s house) or through a mobile van/ambulance which provided separate spaces for counseling and testing were hired for the period. Home based FSWs provide sexual services at lodges or any other location taken by their clients. Their professional identity is hidden from their families and they operate as part of a network and are managed by an individual. Due to the hidden nature of home-based SWs, Vivek strategy with this typology included strong networking with stakeholders. Outreach clinics were operationalized with general health services for SWs and their children. This typology essentially has families and children at home and the identified need for this typology was school admissions, opening bank accounts, Government ration cards which are needed to avail subsidized food items from Government stores, offering literacy classes and other vocational training in crafts such as tailoring and making jewelry, candle, incense sticks, chocolates and bags, among others. Hence Vivek identified the felt need of this typology and addressed those needs.
Male Sex Workers (MSWs) provide sexual services to another man/woman, cruising from one place to another and soliciting clients at any suitable public place, including streets corners, highways, bus stops/depots, public gardens, railways stations and other such pick up points. MSWs find it difficult to access VCT services due to stigma and discrimination by the service providers. Vivek conducted intensive SBC sessions with the service providers to address the issue of stigma and discrimination. Outreach clinics were conducted in hotspots where MSWs were easily accessible.
2.2. Data and Statistical Analyses
Data used to assess the effect of Vivek intervention during the period March 2009-June 2011were drawn from two sources: program monitoring data and ICTC tracking sheet. SWs that accessed services from Aastha program were assigned a unique identification number to track their service utilization during the program. The Aastha program developed and defined program monitoring indicators and established managerial information system (MIS) to gather data periodically on different indicators related to program inputs and outputs. Similarly, the program developed ICTC tracking sheet that collected information on SW particulars like SW Identification number, eligibility and particulars of HIV testing. Program monitoring and the ICTC tracking sheet data were collected on a monthly basis by the program implementing non-governmental organization (NGO) at the site level which were aggregated in table formats and consolidated by FHI360. The staff from FHI360 provided technical support to the implementing NGO to ensure integrity and quality of data as well as flow of data and maintenance of MIS.
The denominator used for the analysis included all sex workers registered with the program. The program protocol indicates that if a person tests negative for HIV in a given month, then he/she is not eligible for a repeat test for the next three months. Therefore from the denominator we subtracted sex workers who were tested in the last 3 months and included those who had tested in the month prior to previous 3 months. The numerator was obtained from the ICTC tracking sheet, since only this data provided typology wise testing information.
Percentages were used to present the results. Trend analysis was conducted to assess the effect of Vivek intervention. The differences in percentages between pre-Vivek (March 2009 to December 2009: from opening of Integrated Counselling and Testing Centers (ICTCs) in the project clinics through the month prior to the month Vivek intervention was initiated) and post-initiation non-Vivek intervention months (February-June 2010; August-November 2010 and January-May 2011; time period after the initiation of Vivek intervention excluding the intervention months); non-Vivek (time period between March 2009 and June 2011 excluding the Vivek intervention months) and Vivek intervention months (months when Vivek intervention was implemented) (Table 1) were tested using Z tests. All analyses were carried out using STATA version 11.1 (StataCorp, College Station, TX, USA).
2.3. Ethical Considerations
Data for this study did not include any personal identifiers. FHI 360 provided general oversight and approval for the collection and analysis of routine programmatic data for examining the effect customized demand generation as a strategy to increase uptake of voluntary counselling and testing services amongst sex workers.
3. Results
A total of 17,005 (72.6%: among those registered with the program) SWs were tested for HIV at least once from March 2009 to July 2011. The proportion of SWs tested in each month during the intervention period is presented in Figure 2 and by typology in Figure 3. The trend indicates an increase in HIV testing over the intervention period. Overall, voluntary HIV testing was higher in Vivek intervention months than non-Vivek months both at baseline prior to the intervention and in intervals between intervention months; 17% SWs were tested for HIV during Vivek months versus 3% in non-Vivek months (P < 0.001) (Table 2). A similar trend in voluntary HIV testing was observed across all typologies. Compared to all other typology of SW, a higher proportion of MSWs underwent voluntary testing (Figure 3).
Further, the results also indicates that as compared to the period before Vivek was initiated, a significantly higher proportion of SWs underwent voluntary testing during post initiation non-Vivek months (1.5% vs. 4.7%, p-value < 0.001) (Table 3) and this increase was observed across all typologies (Table 3).
4. Discussions
Our findings demonstrate that customized operationalization of outreach testing strategies dramatically increased
Table 1. Months during which Vivek intervention was implemented between March 2009-June 2011.
Note: PV: Pre-Vivek; V: Vivek; NV: non-Vivek; PINV: Post initiation non-Vivek.

Figure 2. Trends in HIV testing among sex workers in Mumbai-Thane district: March 2009-January 2011.
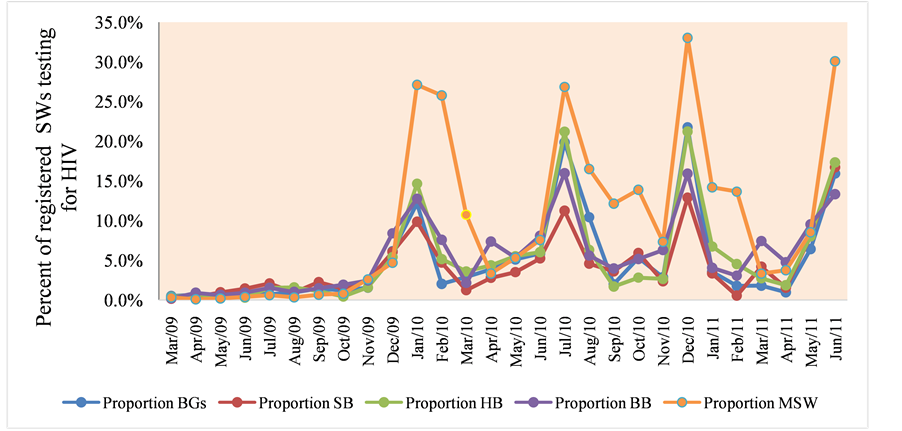
Figure 3. Trends in HIV testing among sex workers in Mumbai-Thane district by typology: March 2009-January 2011. BB: Brothel based SWs; SB: Street based SWs; HB: Home based SWs; MSW: Male sex worker; BG: Bar girls.
Table 2. HIV testing among sex workers during, non-Vivek and Vivek months, by typology in the period between March 2009-June 2011.
aNon-Vivek months: includes months (pre and post initiation of Vivek intervention) when Vivek intervention was not implemented. bVivek months: includes months when Vivek intervention was implemented. SW: Sex worker; FSW: female sex worker; MSW: male sex worker.
Table 3. HIV testing among sex workers during, pre Vivek and post initiation non-Vivek months, by typology in the period between March 2009-June 2011.
aPre-Vivek months: includes months before Vivek intervention was initiated. bPost initiation non-Vivek months: includes months after the initiation of Vivek intervention excluding the intervention months. SW: Sex worker; FSW: female sex worker; MSW: male sex work.
the uptake of Voluntary HIV counselling and testing services. Moreover, these results were consistent across all typologies. HIV testing is the gateway for HIV prevention as early initiation of ART and safer sexual behaviour could potentially reduce transmission together with other interventions [6] -[8] [12] . As voiced in earlier literature, addressing individual and contextual barriers and increasing demand facilitates HIV testing uptake [6] [15] [19] [20] .
During Vivek, demand creation mechanisms were integrated with SBC and counseling as part of a cohesive outreach strategy. The customization approaches directly addressed the main barriers voiced by the SWs. Various customization approaches such as sensitization of key stakeholders, organizing suitable infrastructure for testing in a nearby room in brothels or in the green rooms inside bars, organizing mobile vans for street based SWs, arranging for general health services for home based SWs and intensifying SBC sessions with service providers to address issue of stigma and discrimination for MSWs led to improved access and increased uptake of VCT services by all typologies of SWs.
Additionally, other services such as livelihood skills, general health access and attainment of social entitlements were provided which were well received. The intervention was planned with a broad range of stakeholders in a participatory manner, increasing the subsequent support and buy-in of the community.The coordination between clinic and outreach based on prior planning and joint focused intervention between clinic and outreach teams led to heightened uptake for HIV counseling and testing.
Our findings also indicate an increase in the uptake of HIV testing between pre Vivek months and in the post non-Vivek months. Despite the success of testing during Vivek months, an incremental increase in the post initiation non-Vivek periods were also observed. It is important to ensure that the gains achieved during Vivek and post initiation non-Vivek periods are maintained and further increased. Different customization approaches that were used in Vivek should be continued so that the momentum is maintained and 6 monthly HIV counseling and testing for HIV by SWs as expected in the National guidelines are continually achieved.
Due to intensified efforts, (17,005 out of 23,417) 72% of currently active SWs were tested at least once for HIV (not presented in tabular format). The findings in Vivek are consistent with previous studies where an increase in HIV testing rate was observed in community based VCT program [19] . Despite the widespread availability of VCT tests through project-supported static clinics, uptake of HIV testing was low. Barriers to HIV testing are often logistical and can be overcome with community-based strategies [15] . Evidence suggests that community-based VCTs are preferred over static or health facility-based clinics for HIV testing [15] [21] [22] as was observed in our study with a dramatic increase in the uptake of HIV testing during Vivek months.
The success of the Vivek model piloted under Aastha led to the replication of this approach in governmentfunded targeted intervention projects. All the sex workers who tested HIV positive and were willing to disclose their status were linked to care, support and treatment services. Those who tested HIV negative were also directed to post-test services for further counseling, referrals and support to motivate them to remain negative and practice safer sexual behaviors.
Vivek interventions can increase the uptake of VCT, particularly in hard-to-reach areas, in both mobile populations and for women who are normally constrained from seeking VCT due to control by gatekeepers like brothel and bar managers. This increase in health seeking behavior was reflected in the rapid increase of HIV testing and counseling uptake in a short period of time, with subsequent drops when the intervention was not implemented. An integrated and uniquely tailored outreach strategy may prove to be a key component in the successful and sustained control of HIV epidemic.
5. Conclusion
In conclusion, the data presented in this study suggest that customized outreach approaches are valuable strategies to increase uptake of VCT. Vivek addressed barriers to VCT specific to SW from various work environments and addressed these with unique adaptation of existing Aastha program. Familiarity with the Aastha system helped sex workers in regularly accessing services of HIV testing and counselling. The constraints most commonly felt were overcome by customizing the services to the living and working conditions of the sex workers.
Competing Interests
None.
Authors’ Contributions
SG led the conceptualization and provided overall guidance with writing and editing the manuscript. SB conducted the intervention and wrote the manuscript. SR assisted with conceptualization of analytic approach and interpretation of study findings. All authors have read and approved this final submitted manuscript. All the authors contributed equally to this work.
Acknowledgements
Since 2004, FHI 360 has been implementing the Aastha project with the goal to reduce the incidence of STIs and HIV among female sex workers (FSWs) and their regular partners in the Mumbai and Thane districts of Maharashtra state in India. The authors wish to acknowledge the Implementing Partners and all the sex workers who participated in the initiative. The authors would also like to acknowledge the Bill & Melinda Gates Foundation, who have funded this project through Avahan, its India AIDS Initiative. However, the views expressed herein are those of the authors and do not reflect the official policy or position of the Bill & Melinda Gates Foundation and Avahan. Also this paper was written as part of a mentorship program within the Knowledge Network project coordinated by the Population Council, which is a grantee of the Bill and Melinda Gates Foundation through Avahan, the foundation’s India AIDS Initiative.
References
- National AIDS Control Organization (NACO) (2008) HIV Sentinel Surveillance and HIV Estimation in India 2007—A Technical report. National AIDS Control Organization (NACO), New Delhi.
- National AIDS Control Organization (NACO) (2012) HSS Sentinel Surveillance 2010-11—A Technical Brief. National AIDS Control Organization (NACO), New Delhi.
- UNAIDS (2008) 2008 Report on the Global AIDS Epidemic. UNAIDS, Geneva.
- National AIDS Control Organization (NACO) (2008) Annual Report NACO 2008-09. National AIDS Control Organization (NACO), New Delhi.
- Hollingsworth, T.D., Anderson, R.M. and Fraser, C. (2008) HIV-1 Transmission, by Stage of Infection. The Journal of Infectious Diseases, 198, 687-693. http://dx.doi.org/10.1086/590501
- Chakrapani, V., Shanmugam, M., Michael, S., Velayudham, J. and Newman, P.A. (2008) HIV Testing Barriers and Facilitators among Populations At-Risk in Chennai, India. Chennai, India: Indian Network for People living with HIV (INP+).
- Denison, J.A., O’Reilly, K.R., Schmid, G.P., Kennedy, C.E. and Sweat, M.D. (2008) HIV Voluntary Counseling and Testing and Behavioral Risk Reduction in Developing Countries: A Meta-Analysis, 1990-2005. AIDS and Behavior, 12, 363-373. http://dx.doi.org/10.1007/s10461-007-9349-x
- Vanichseni, S., Choopanya, K., Des Jarlais, D.C., Plangsringarm, K., Sonchai, W., et al. (1992) HIV Testing and Sexual Behavior among Intravenous Drug Users in Bangkok, Thailand. Journal of Acquired Immune Deficiency Syndromes, 5, 1119-1123.
- Obermeyer, C.M. and Osborn, M. (2007) The Utilization of Testing and Counseling for HIV: A Review of the Social and Behavioral Evidence. American Journal of Public Health, 97, 1762-1774. http://dx.doi.org/10.2105/AJPH.2006.096263
- Bunnell, R., Ekwaru, J.P., Solberg, P., Wamai, N., Bikaako-Kajura, W., et al. (2006) Changes in Sexual Behavior and Risk of HIV Transmission after Antiretroviral Therapy and Prevention Interventions in Rural Uganda. AIDS, 20, 85-92. http://dx.doi.org/10.1097/01.aids.0000196566.40702.28
- Hong, Y., Zhang, C., Li, X., Fang, X., Lin, X., et al. (2012) HIV Testing Behaviors among Female Sex Workers in Southwest China. AIDS and Behavior, 16, 44-52. http://dx.doi.org/10.1007/s10461-011-9960-8
- Bond, L., Lauby, J. and Batson, H. (2005) HIV Testing and the Role of Individualand Structural-Level Barriers and Facilitators. AIDS Care, 17, 125-140.
http://dx.doi.org/10.1080/09541020512331325653 - Chakrapani, V., Newman, P.A. and Shunmugam, M. (2008) Secondary HIV Prevention among Kothi-Identified MSM in Chennai, India. Culture, Health & Sexuality, 10, 313-327.
http://dx.doi.org/10.1080/13691050701816714 - Kalichman, S.C. and Simbayi, L.C. (2003) HIV Testing Attitudes, AIDS Stigma, and Voluntary HIV Counselling and Testing in a Black Township in Cape Town, South Africa. Sexually Transmitted Infections, 79, 442-447. http://dx.doi.org/10.1136/sti.79.6.442
- Morin, S.F., Khumalo-Sakutukwa, G., Charlebois, E.D., Routh, J., Fritz, K., et al. (2006) Removing Barriers to Knowing HIV Status: Same-Day Mobile HIV Testing in Zimbabwe. Journal of Acquired Immune Deficiency Syndromes, 41, 218-224. http://dx.doi.org/10.1097/01.qai.0000179455.01068.ab
- National AIDS Control Organization (NACO) (2005) UNGASS India Report: Progress Report on the Declaration of Commitment on HIV/AIDS. United Nations General Assembly Special Session on HIV/AIDS, New Delhi.
- Creek, T.L., Ntumy, R., Seipone, K., Smith, M., Mogodi, M., et al. (2007) Successful Introduction of Routine Opt-Out HIV Testing in Antenatal Care in Botswana. Journal of Acquired Immune Deficiency Syndromes, 45, 102-107. http://dx.doi.org/10.1097/QAI.0b013e318047df88
- FHI 360 (2011) New Dimensions to HIV/AIDS Programming in Aastha II. FHI 360, Mumbai.
- Sweat, M., Morin, S., Celentano, D., Mulawa, M., Singh, B., et al. (2011) Community-Based Intervention to Increase HIV Testing and Case Detection in People Aged 16 - 32 Years in Tanzania, Zimbabwe, and Thailand (NIMH Project Accept, HPTN 043): A Randomised Study. The Lancet Infectious Diseases, 11, 525-532. http://dx.doi.org/10.1016/S1473-3099(11)70060-3
- Dandona, L., Sisodia, P., Ramesh, Y.K., Kumar, S.G., Kumar, A.A., et al. (2005) Cost and Efficiency of HIV Voluntary Counselling and Testing Centres in Andhra Pradesh, India. The National Medical Journal of India, 18, 26-31.
- Baiden, F., Akanlu, G., Hodgson, A., Akweongo, P., Debpuur, C., et al. (2007) Using Lay Counsellors to Promote Community-Based Voluntary Counselling and HIV Testing in Rural Northern Ghana: A Baseline Survey on Community Acceptance and Stigma. Journal of Biosocial Science, 39, 721-733. http://dx.doi.org/10.1017/S0021932006001829
- Fylkesnes, K. and Siziya, S. (2004) A Randomized Trial on Acceptability of Voluntary HIV Counselling and Testing. Tropical Medicine & International Health, 9, 566-572. http://dx.doi.org/10.1111/j.1365-3156.2004.01231.x
NOTES

*These authors contributed equally to this work.
#Corresponding author.


