Food and Nutrition Sciences
Vol. 2 No. 9 (2011) , Article ID: 8373 , 7 pages DOI:10.4236/fns.2011.29127
Maternal Body Composition and Its Relationship to Infant Breast Milk Intake in Rural Pakistan
![]()
1Pakistan Institute of Nuclear Science and Technology, Islamabad, Pakistan; 2MRC Human Nutrition Research, Cambridge, UK.
Email: les.bluck@mrc-hnr,cam.ac.uk
Received July 8th, 2011; revised August 26th, 2011; accepted September 5th, 2011.
Keywords: Stable isotopes, Breast Milk Intake, Maternal Body Composition
ABSTRACT
Some women in rural Pakistan are chronically undernourished, and consequently underwei-ght. Concerns have been expressed that the degree of undernourishment might be suffici-ently severe to affect lactation performance. We have obtained data on maternal body composition and infant breast milk intake using stable isotope methods in a group of thirty three mother and infant pairs at approximately six months of age. The maternal body mass index ranged from 16.6 to 29.1 kg·m−2. In this population we found that exclusive breast-feeding tended to be associated with lower maternal body fat, and that there was no evidence for compromised lactational performance due to malnourishment. Finally we note that when our data is combined with that from other studies there may be a generalised negative correlation between breast milk intake and maternal body fat.
1. Introduction
Body composition, specifically the relative quantities of fat and lean tissue, is an important indicator of general health. There exist prediction equations which allow the percentage of body weight due to fat to be calculated from simple anthropomorphic measures and characteristics such as weight, height, sex and age [1,2]. In many cases these predictive equations are simplified so that the simple measure of body mass index, BMI = (weight)/ (height)2, is used. Adults with BMI > 25 kg·m−2 are classed as overweight, and those with BMI > 30 kg·m−2 as obese [3] regardless of sex. However a major limitation of BMI is that it cannot differentiate between increased weight for height due to lean tissue or fat [4].
It is a common belief that the body composition of a lactating mother affects breast milk output. Nutritionally human milk is the ideal food in the early stages of life, and the current recommendation is that exclusive breast feeding should be practiced for the first six months of infant life [5]. It has been estimated that the universal adoption of this practice with continued partial breast feeding for a further six months could prevent 13% of childhood mortality under five years of age [6]. The gestational increase in maternal fat deposits is expected to be lost during the period of lactation, and although lactation performance is remarkably resistant to maternal energy deficit it can be compromised by extreme long-term caloric insufficiency [7]. In the setting of a village in rural Pakistan, where we have observed a wide range of BMI in the population of lactating women, there are concerns that some mothers living under harsh conditions may be chronically undernourished and that this may cause breast milk production to be insufficient [8]. We therefore decided to investigate the relationship between maternal body composition and breast-milk intake in this small population.
Precise quantification of the amount of breast milk received by a suckling infant can be difficult. Test weighing methods have the disadvantage that they interfere with the usual feeding practices, and special measures are required to assess night time feeding sessions [9]. Stable isotope methods, on the other hand, do not interfere with the subject’s routine behavior. The dose-to-the-mother method [10] not only gives estimates of both breast milk and water flux from other foods consumed by the baby, but also gives precise information on maternal body composition. Therefore it is the ideal methodology for investigating the relationship between breast feeding and the nutritional status of the mother. The objective of this study was to use this technique to investigate the relationship between maternal body composition (percentage body fat) and lactation performance in this group of Pakistani mothers.
2. Subjects and Methods
2.1. Subjects
The data reported here were obtained in a subset of lactating women participating in wider-ranging study into the effects of post-natal depression in the rural area of Sohawa in North Pakistan. The subjects recruited were housewives in family units living on small holdings, and routinely occupied in housework. Occasionally they were required to assist in gathering crops, but otherwise stayed at home. The women habitually wore full dress, with only their hands and face exposed to sunlight. They were not suffering from any known disease, non-smokers, not addicted to pan (Betel leaf (Piper betle) mixed with the seed of the tropical palm, Areca catechu, lime, and menthol which acts as a stimulant) or any other substance, and reporting either exclusive or partial breast feeding (use of formula or cow’s milk). The subset studied here had infants in the age range 150 - 230 days at the start of the breast milk intake measurement.
The subjects were recruited at the local community health clinic with the help of their health workers. The purpose of the study and the requirements of the participants were explained, and written consent was obtained from each mother. This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects were approved by the Pakistan Institute of Nuclear Sciences and Technology (PINSTECH) ethics committee.
2.2. Breast Milk Intake Protocol
On the day of dosing (day 0) the participants were visited at home by members of the study team, and the mother’s height (±5 mm) and weight (±100 g) recorded for the purposes of calculating body composition. The infant’s weight (±100 g) was recorded using a digital balance, and the length (±5 mm) measured using a graduated length board obtained locally. These measurements were performed by trained members of the research group. A baseline saliva sample (3 mL) was collected from the mother by asking her to chew a small piece of cotton wool to stimulate saliva secretion, and then spit into a syringe barrel preloaded with another piece of cotton wool to act as a filter. The syringe plunger was then replaced, and the saliva sample squeezed into a collection tube (Sterilin Ltd, Caerphilly, UK). A baseline urine sample (5 mL) was collected from the infant (which if they had been not been potty-trained was obtained by placing cotton-wool pads in the nappy), and then the mother was given a dose of 7 g of D2O (CIL, Andover, MA) in 63 g of local drinking water.
Members of the study team returned to the family home 1, 2, 3, 4, 13 and 14 days post dosing in order to collect further maternal saliva and infant urine samples. Care was taken to ensure that at least one hour had elapsed between the mother consuming food or drink and the saliva collection. All samples were frozen on the day of collection and ultimately transported frozen at −30˚C to the PINSTECH laboratory for mass spectrometric analysis. At the final visit the baby’s weight was remeasured so that corrections for growth could be applied to the breast-milk intake calculation.
2.3. Sample Isotopic Analysis
After thawing at ambient temperature the samples were centrifuged for 15 minutes, and the supernatant transferred to an Eppendorf tube. An aliquot of 8 μL was taken and reduced to hydrogen gas using the zinc shot method [11]. Isotopic composition of the hydrogen was measured using a gas isotope ratio mass spectrometry (Varian MAT GD-150, Bremen, Germany).
Maternal body composition and infant breast-milk intake was calculated as described previously [12]. Briefly, the mother and baby are modelled as two compartments with flow (due to breast milk) from the mother to the baby. This model allows the estimation of four primary parameters: maternal body composition, maternal water turnover, infant water turnover water flux from mother to infant and water flux from mother to infant. By making simple assumptions regarding breast milk composition breast milk intake by the infant can be derived from the last of these four parameters. In addition by subtracting the flux from the mother to the infant from the infant water turnover the amount of water derived from sources other than breast-milk (i.e. complementary feeding) can be obtained. The ratio between water derived from breastmilk and the total water obtained orally can be taken as representing the fraction of feed due to breast milk.
The curve fitting was accomplished by minimizing the proportional residuals between observed data points and those predicted using a two-compartment model [13] using the non-linear fitting function in Excel (Microsoft Inc, Redmond, WA). Results which showed total infant fluid turnover greater than 1.2 or less than 0.3 L·day−1 were considered implausible and excluded from further analysis. Further statistical analysis was performed using either the built-in functions in Excel or SPSS for windows (SPSS Inc, Chicago, IL). Unless otherwise stated, the results are quoted as mean ± standard deviation.
3. Results
3.1. Anthropometry
A total of 37 mother/infant dyads were studied. Of these 4 could not be satisfactorily described by the model (implausible values for water intake), reducing the size of the dataset to 33. The average maternal age at the time of measurement was 29.7 (range 18 - 38) years, height 1.56 ± 0.05 m, weight 53.7 ± 8.0 kg and body mass index (BMI) 22.0 ± 3.5 kg·m−2. Parity data was not available. According to WHO criteria four of the mothers were underweight (BMI < 18.5 kg·m−2) and eight were classed as overweight (BMI 25 - 30 kg·m−2), with the remainder in the normal weight range.
The infants (20 boys/13 girls) had an average age of 186 ± 20 days, and at the start of the measurement period had length 65 ± 3cm and weight 6.9 ± 0.8 kg. The average weight increase during the two week measurement period was 0.27 ± 0.18 kg. Two of the 33 infants lost weight during the experimental period. Generally the infants were small for age when compared with the WHO growth curves [14], but there was no apparent difference in the infants growth based on maternal weight (Figure 1—data shown only for male infants since none of the underweight mothers had girls).
3.2. Maternal Body Composition and Breast Milk Intake
From the isotope data the mean maternal lean body mass was 35.67 ± 4.6 kg, and the body fat 33 ± 9% of total body weight. As expected the fraction of body mass due to fat was highly correlated with BMI, r2 = 0.38, p < 10−4. The mean water turnover of the mothers was 3.4 ± 1.0 L·day−1. Breast milk intake was determined to be 637 ± 247 g·day−1 (range 62 - 1090 g·day−1). Water consumed orally other than breast milk ranged from 0 to 890 g g·day−1, with total infant water consumption determined
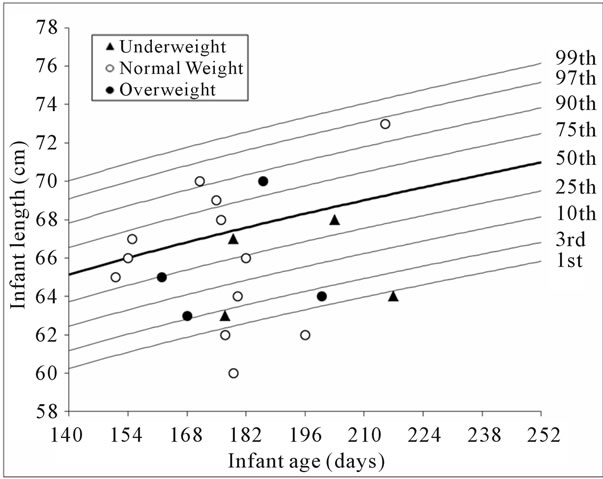
Figure 1. Comparison of the infant boys’ height and weight with the current WHO growth curves. Data are plotted for the nominally underweight (BMI < 18.5 kg·m−2), normal weight and overweight (BMI > 25 kg·m−2) mothers.
to be 803 ± 209 g·day−1. Breast milk accounted for 80% ± 24% of infant total water consumption; however the distribution was highly skewed towards exclusive breast feeding (Figure 2) with an interquartile range 72% - 96%.
No association was found between breast milk intake and infant age (Figure 3), or between the fraction of feed due to breast milk and infant weight. Infant weight, however, was positively correlated with total water intake (r2 = 0.25, p~0.001).
A plot of the fraction of feed consumed by the infant which is breast milk against the body composition of the mother is given in Figure 4. This indicates that in this population the introduction of complementary foods be-
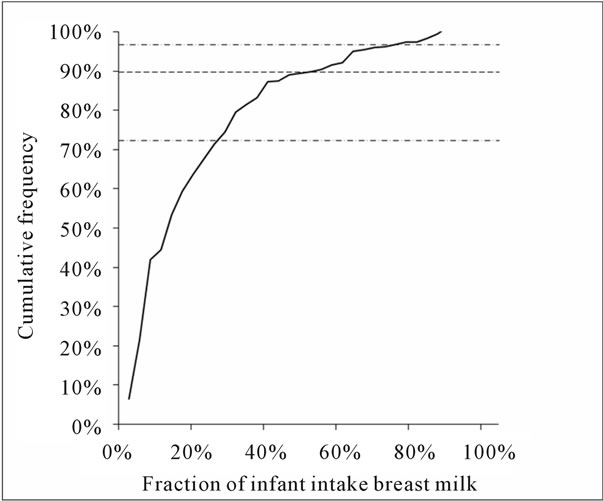
Figure 2. Distribution of degree of exclusivity of breast feeding.
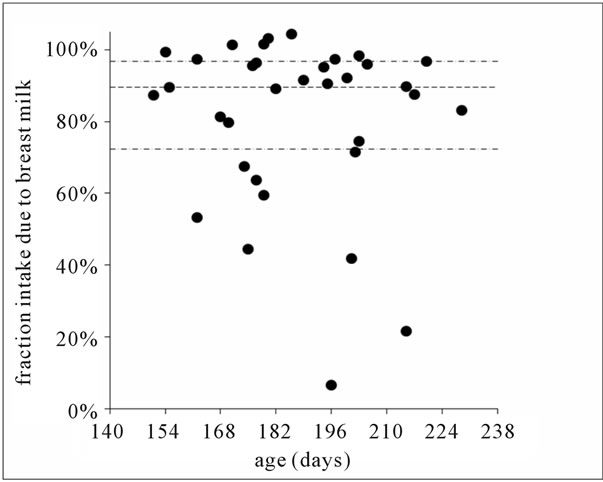
Figure 3. Fraction of ingested water from breast milk against infant age. This indicates that systematic age-related introduction of complementary food had not begun in the group under study.
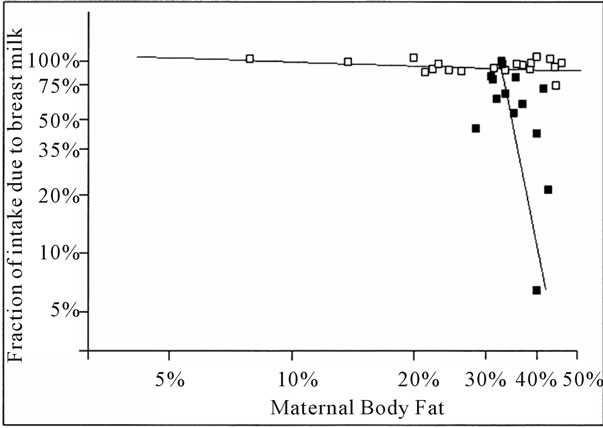
Figure 4. The relationship between the infant diet and maternal body composition. The solid lines are generated by linear regression at the extrema, and the comparative distances of any given data point from the two lines used to classify into EBF (Exclusively Breast-Fed, open points) or PBF (Partially Breast-Fed, solid points).
fore seven months is most likely for mothers with higher degrees of body fat. The plot is used to assign each mother to either an exclusive breast feeding (EBF) or partial breast-feeding (PBF) behaviour. This is done by fitting straight lines to the regions of the extrema, and using the normal distance from these lines as indices for the classification; i.e. a data point lying closer to the line constructed from the points from the lower right quadrant of the figure is classed as PBF, and conversely one nearer to the line drawn from the points in the upper left quadrant is classed as EBF. On this basis 19 of the 33 mothers are designated EBF.
4. Discussion
The analysis was performed in order to determine the association between maternal body composition and breast feeding performance in rural Pakistan. In the population of 37 mothers studied in this work 4 were classed as underweight and 8 overweight. The stable isotope methodology used is particularly suited to investigation of their lactation performance in comparison with their normal-weight peers because it provides simultaneous assessment of the “degree of fatness” of the mother and the average daily quantity of breast milk consumed by her offspring. The primary finding of this work is that the underweight women were more likely to be exclusive breast feeders, and since their children exhibited similar growth to those of their normal weight counterparts, the well-being of their children does not appear to be compromised.
An inverse relationship between breast milk output and maternal body fat has been reported previously [13, 15,16]; the current data reinforces these observations, and furthermore indicates that high levels of maternal body fat are associated with decreased breast-milk intake and increased use of other foods. It is unknown whether these factors are all due to slightly increased affluence, or if the introduction of complementary foods with concomitant reduction in breast feeding reduces the energy cost to the mother, allowing her to increase weight.
Many published estimates of energy requirements of infants are based on infants receiving breast milk substitutes, but these are overestimates for predominantly breastfed infants [17]. However a recently published report [18] gives an average energy requirement of about 330 kJ·kg−1·day−1 for exclusively (or near-exclusively) breastfed infants aged six months. Assuming an energy density for breast-milk of about 2.9 kJ·kg−1 [8] this equates to 790 ± 90 g·day−1 breast milk. Using the simple classification scheme demonstrated in Figure 4 to identify the EBF mothers, this group can be studied in isolation. The energy difference between recommended and estimated energy intake is 287 ± 435 kJ·day−1 (13% of estimated requirement).
The dose-to-the-mother method has been used in some other populations at risk of malnutrition, however the effect of maternal body composition has not always been considered. Data have been obtained in The Gambia [10], Papua New Guinea [19], Ethiopia [20], Mexico [15,21], Malawi [16], Bangladesh [22], Brazil [13], and Kenya [8], and is summarized for exclusive breast feeding in Table 1.
From these data milk intake in Pakistan is lower than observed in many other similar settings. This may be in part due to the children being smaller. It has been shown that lactation performance is robust against moderate maternal undernourishment, although it will inevitably be compromised by very low energy intakes [23,24], as is probably the case for the Kenyan subjects described in Table 1. Eliminating these data on this basis there is a significant inverse correlation between breast milk intake and maternal body composition even when subjects are of differing ethnicity (Figure 5).
5. Conclusions
We have shown that in a small cohort in rural Pakistan, leaner babies with the highest breast milk intake have leaner mothers, which may have been due to greater fat mobilization in those women who have not yet introduced complementary foods. Comparison with similar cohorts studied in other communities worldwide reinforces the observation that breast milk intake and maternal body fat are inversely correlated.
6. Acknowledgements
The data were collected for a national project titled, “Ef-
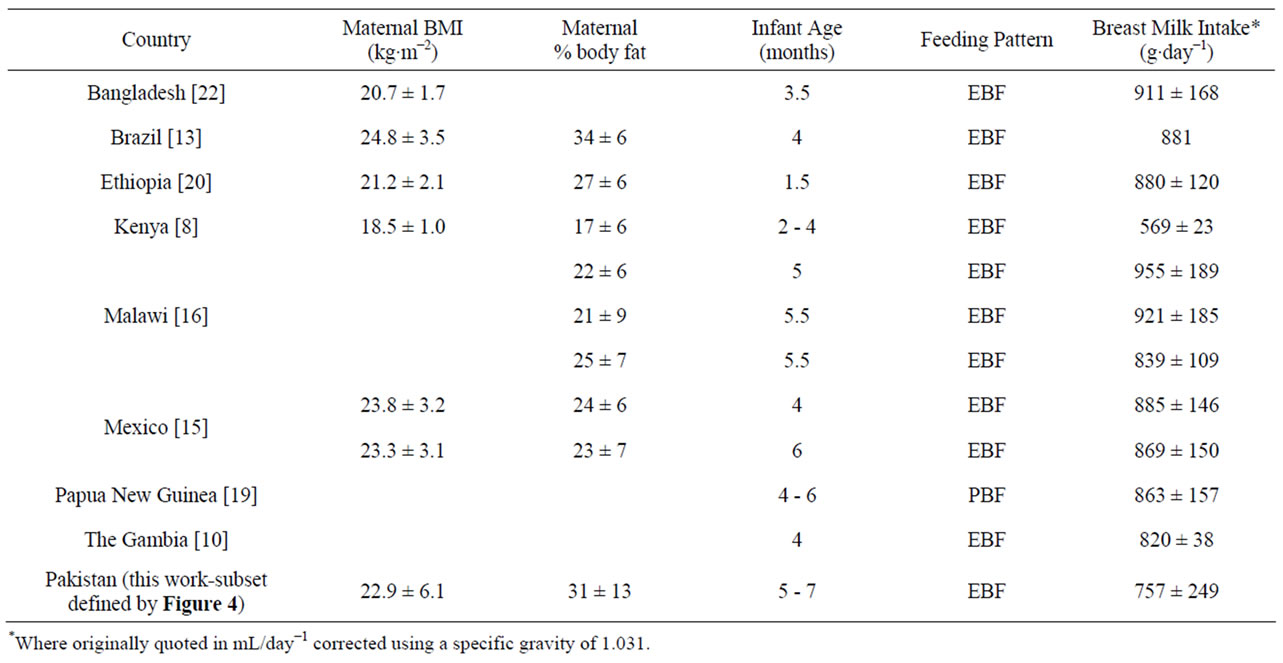
Table 1. Comparison of milk intake measurements made using the dose-to-the-mother method in a number of settings. EBF—exclusively breast-fed, PBF—partially breast-fed.
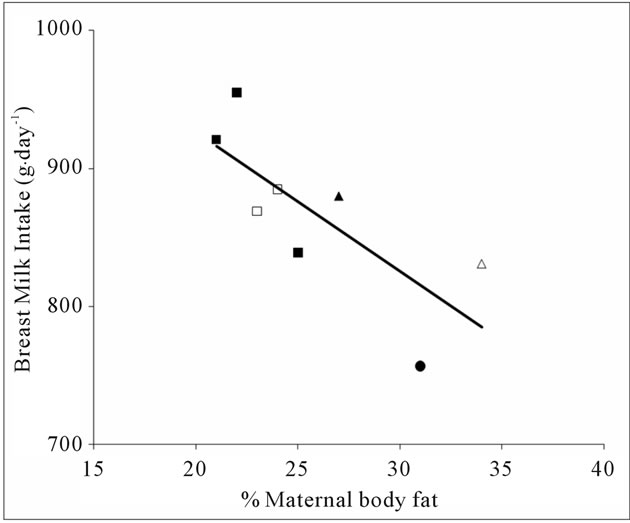
Figure 5. Cross-national comparison of breast milk intake as a function of maternal composition Solid squares—data from Malawi [16], Open squares—Mexico [15], Solid triangles—Ethiopia [20], Open triangles—Brazil [13], Solid circle—from this data.
fect of Maternal Depression on Intake of Breast milk in Infants” which was funded by Higher Education Commission of Pakistan, HEC NRPU Grant Number 472. The authors also acknowledge the International Atomic Energy Agency (IAEA) for funding the award of a Fellowship to MS Nafeesa Nazlee under IAEA Technical Cooperation project PAK/6/018 which made the writing of this manuscript at HNR possible.
NN did the fieldwork, contributed to the data analysis, and co-wrote the manuscript, RB contributed to study design, contributed to data analysis and critically reviewed the manuscript, ZL did the mass spectrometric analysis and critically reviewed the manuscript. LB contributed to the data analysis and co-wrote the manuscript.
None of the authors have any conflict of interest to disclose.
REFERENCES
- J. S. Garrow and J. Webster, “Quetelet Index (w/h−2) as a Measure of Fatness,” International Journal of Obesity, Vol. 9, No. 2, 1985, pp. 147-153.
- A. S. Jackson, P. R. Stanforth, J. Gagnon, T. Rankinen, A.S. Leon, D. C. Rao, J. S. Skinner, C. Bouchard and J. H. Wilmore, “The Effect of Sex, Age and Race on Estimating Percentage Body Fat from Body Mass Index: The Heritage Family Study,” International Journal of Obesity, Vol. 26, No. 6, 2002, pp. 789-796.
- S. B. Racette, S. S. Deusinger and R. H. Deusinger, “Obesity: Overview of Prevalence, Etiology, and Treatment,” Physical Therapy, Vol. 83, No. 3, 2003, pp. 276- 288.
- S. Meeuwsen, G. W. Horgan and M. Elia, “The Relationship between BMI and Percent Body Fat, Measured by Bioelectrical Impedance, in a Large Adult Sample is Curvilinear and Influenced by Age and Sex,” Clinical Nutrition, Vol. 29, No. 5, 2010, pp. 560-566. doi:10.1016/j.clnu.2009.12.011
- WHO, “Global Strategy for Infant and Young Child Feeding,” World Health Organization, Geneva, 2003.
- G. Jones, R. W. Steketee, R. E. Black, Z. A. Bhutta, S. S. Morris and G. Bellagio, “Child Survival Study, How Many Child Deaths Can We Prevent This Year?” Lancet, Vol. 362, No. 9377, 2003, pp. 65-71. doi:10.1016/S0140-6736(03)13811-1
- A. M. Prentice, A. A. Paul, A. Prentice, A. Black and T. J. Cole, “Cross-Cultural Differences in Lactaional Performance, in Human Lactation 2: Maternal and Environmental Factors,” M. Hamosh and A. S. Goldman, Eds., Planum, New York, 1986, pp. 13-44.
- G. A. Ettyang, W. D. V. Lichtenbelt, F. Esamai, W. H. M. Saris and K. R. Westerterp, “Assessment of Body Composition and Breast Milk Volume in Lactating Mothers in Pastoral Communities in Pokot, Kenya, Using Deuterium Oxide,” Annals of Nutrition and Metabolism, Vol. 49, No. 2, 2005, pp. 110-117. doi:10.1159/000084744
- S. M. Imong, D. A. Jackson, L. Wongsawasdii, S. Ruckphaophunt, A. Tansuhaj, P. Chiowanich, M. W. Woolridge, R. F. Drewett, J. D. Baum and K. Amatayakul, “Predictors of Breast-Milk Intake in Rural Northern Thailand,” Journal of Pediatric Gastroenterology Nutrition, Vol. 8, No. 3, 1989. pp. 359-370. doi:10.1097/00005176-198904000-00017
- W. A. Coward, T. J. Cole, M. B. Sawyer, A. M. Prentice and A. K. Orrewing, “Breast-Milk Intake Measurement in Mixed-Fed Infants by Administration of Deuterium-Oxide to Their Mothers,” Human Nutrition-Clinical Nutrition, Vol. 36, No. 2, 1982, pp. 141-148.
- C. Kendall and T. B. Coplen, “Multisample Conversion of Water to Hydrogen by Zinc for Stable Isotope Determination,” Analytical Chemistry, Vol. 57, No. 7, 1985, pp. 1437-1440. doi:10.1021/ac00284a058
- J. C. K. Wells, R. Bilal, K. A. Abbass, Z. Latif, S. Roohi and A. Hafeez, “Breast-Milk Intake in Exclusively Breastfed Pakistani Infants: An Estimation by Deuterium Dilution Method,” Pakistan Paediatric Journal, Vol. 31, No. 3, 2007, pp. 111-119.
- H. Haisma, W. A. Coward, E. Albernaz, G. H. Visser, J. C. K. Wells, A. Wright and C. G. Victoria, “Breast Milk and Energy Intake in Exclusively, Predominantly, and Partially Breast-Fed Infants,” European Journal of Clinical Nutrition, Vol. 57, No. 12, 2003, pp. 1633-1642. doi:10.1038/sj.ejcn.1601735
- WHO, “WHO Child Growth Standards,” World Health Organization, Geneva, 2006.
- S. F. Villalpando, N. F. Butte, W. W. Wong, S. Floreshuerta, M. D. Hernandezbeltran, E. O. Smith and C. Garza, “Lactation Performance of Rural Mesoamerindians,” European Journal of Clinical Nutrition, Vol. 46, No. 5, 1992, pp. 337-348.
- L. Galpin, C. Thakwalakwa, J. Phuka, P. Ashorn, K. Maleta, W. W. Wong and M. J. Manary, “Breast Milk Intake Is Not Reduced More by the Introduction of Energy Dense Complementary Food than by Typical Infant Porridge,” Journal of Nutrition, Vol. 137, No. 7, 2007, pp. 1828-1833.
- N. C. de Bruin, H. J. Degenhart, S. Gal, K. R. Westerterp, T. Stijnen and H. K. A. Visser, “Energy Utilization and Growth in Breast-Fed and Formula-Fed Infants Measured Prospectively during the First Year of Life,” American Journal of Clinical Nutrition, Vol. 67, No, 5, 1998, pp. 885-896.
- SACN, “SACN Energy Requirements Working Group Draft Report,” 2010. http://www.sacn.gov.uk/pdfs/5nov_sacn_energy_drafting_group_draft.pdf
- A. K. Orr-Ewing, P. F. Heywood and W. A. Coward, “Longitudinal Measurements of Breast-Milk Output by a H2(2)-O Tracer Technique in Rural Papua-New-Guinean Women,” Human Nutrition-Clinical Nutrition, Vol. 40C, No. 6, 1986, pp. 451-467.
- Z. Getahun, R. Elsom, H. Gsellasie, L. J. C. Bluck, Y. Taffese, A. Wright and G. Jennings, “Breast Milk Intake Measured by Deuterium Kinetics in Mother-Infant Pairs in Addis Ababa,” Ethiopia Journal Health and Development, Vol. 13, No. 3, 1999, pp. 271-280.
- L. Barbosa, N. F. Butte, S. Villalpando, W. W. Wong and E. O. Smith, “Maternal Energy Balance and Lactation Performance of Mesoamerindians as a Function of Body Mass Index,” American Journal of Clinical Nutrition, Vol. 66, No. 3, 1997, pp. 575-583.
- S. E. Moore, A. M. Prentice, W. A. Coward, A. Wright, E. A. Frongillo, A. J. C. Fulford, A. P. Mander, L. A. Persson, S. E. Arifeen and I. Kabir, “Use of Stable-Isotope Techniques to Validate Infant Feeding Practices Reported by Bangladeshi Women Receiving Breastfeeding Counseling,” American Journal of Clinical Nutrition, Vol. 85, No. 4, 2007, pp. 1075-1082.
- A. M. Prentice, R. G. Whitehead, S. B. Roberts and A. A. Paul, “Long-Term Energy-Balance in Childbearing Gambian Women,” American Journal of Clinical Nutrition, Vol. 34, No. 12, 1981, pp. 2790-2799.
- R. G. Whitehead, A. A. Paul, A. E. Black and S. J. Wiles, “Recommended Dietary Amounts of Energy for Pregnancy and Lactation in the United Kingdom,” Food and Nutrition Bulletin, Supplement 5, 1981, pp. 259-265.

