Advances in Infectious Diseases
Vol.4 No.1(2014), Article ID:43403,4 pages DOI:10.4236/aid.2014.41004
Spondylodiscitis Caused by Streptococcus dysgalactiae Subspecies Equisimilis: A Case Report of an Increasingly Recognized Pathogenic Organism
Sara Beça1*, Sandra Xerinda2, António Sarmento2
1Department of Internal Medicine, Hospital Pedro Hispano, Matosinhos, Portugal
2Department of Infectious Diseases—Nephrology Research and Development Unit (FCT-225), Faculty of Medicine, University of Porto, Centro Hospitalar São João, Porto, Portugal
Email: *beca.sara@gmail.com
Copyright © 2014 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/


Received 19 November 2013; revised 19 December 2013; accepted 26 December 2013
ABSTRACT
Streptococcus dysgalactiae subspecies equisimilis (SDSE) is a β-hemolytic Streptococcus that possesses genetic and clinical similarities to Streptococcus pyogenes. It is increasingly recognized as the etiological microorganism of invasive diseases. We report a case of a 74-year-old male who was admitted to this hospital with lower back and neck pain and infected with leg ulcer. The diagnosis of spondylodiscitis C2-C3 and L1-L3 caused by Streptococcus dysgalactiae subsp. equisimilis was made. The present case demonstrates the risk of older patients of developing invasive disease upon skin infection with Streptococcus dysgalactiae subsp. equisimilis, even when risk factors are absent or well controlled (as was diabetes mellitus in this case), suggesting that the pathogenic potential of SDSE should not be underestimated.
Keywords:Spondylodiscitis; Vertebral Osteomyelitis; Streptococcus dysgalactiae Subspecies Equisimilis; Diabetes Mellitus

1. Introduction
Streptococcus dysgalactiae subspecies equisimilis (SDSE) is a β-hemolytic large-colony-forming species that usually possesses Lancefield group G carbohydrate antigens (less frequently it may have A, C, or L group antigens) [1] . It has been established as a possible component of the normal flora of the skin, oropharynx, gastrointestinal and genitourinary tracts, and for many years it was considered non-pathogenic [2] . However, SDSE isolates possessing group G antigen have recovered increasingly from invasive streptococcal infections [2] .
The closest species for SDSE is S. pyogenes. There is a range of genes showing a high degree of homology with corresponding genes of S. pyogenes, including genes encoding virulence factors. As a result, both microorganisms show similar pathogenicity [3] . Patients with SDSE infections were reported to be older than those with group A or group B Streptococcus infections and frequently have underlying diseases [1] [2] . Patients affected by SDSE often present with skin and soft tissue infection and streptococcal toxic shock syndrome [1] . Few cases of spondylodiscitis due to SDSE have been described so far. Here, we present a case of spondylodiscitis caused by SDSE, highlighting the pathogenic potential of group G streptococci in healthy adults.
2. Case Report
A 74-year-old caucasian man presented to hospital with a week history of lower back and neck pain. There was no history of trauma and he was taking anti-inflammatory medications with a scarce effect. Two days before these symptoms he noted pain and erythema of the right leg.
Careful history taking revealed a history of diabetes mellitus diagnosed 5 years earlier, well controlled only with diet (glycated hemoglobin 6.5%). He also had obesity, nephrolithiasis and history of cellulitis on the left leg many years ago.
On admission he was alert, his temperature was 38.2˚C, the blood pressure was 152/89 mmHg and the heart and lung sounds were unremarkable. There were clinical signs of infection on the right leg with edema and small points of purulent discharge. Motor strength and sensory function were normal as well as deep tendon reflexes. A blood sample was taken and revealed mild normocytic anaemia (Hb 11.2 g/dL), white blood cells 9970/mm3 (neutrophil 80.5%), and elevated C-reactive protein (27.67 mg/dL) and erythrocyte sedimentation rate (105 mm/h). He had serum creatinine, liver enzymes and creatine kinase within normal values. Two peripheral blood cultures were performed on admission and amoxicillin-clavulanic acid was started.
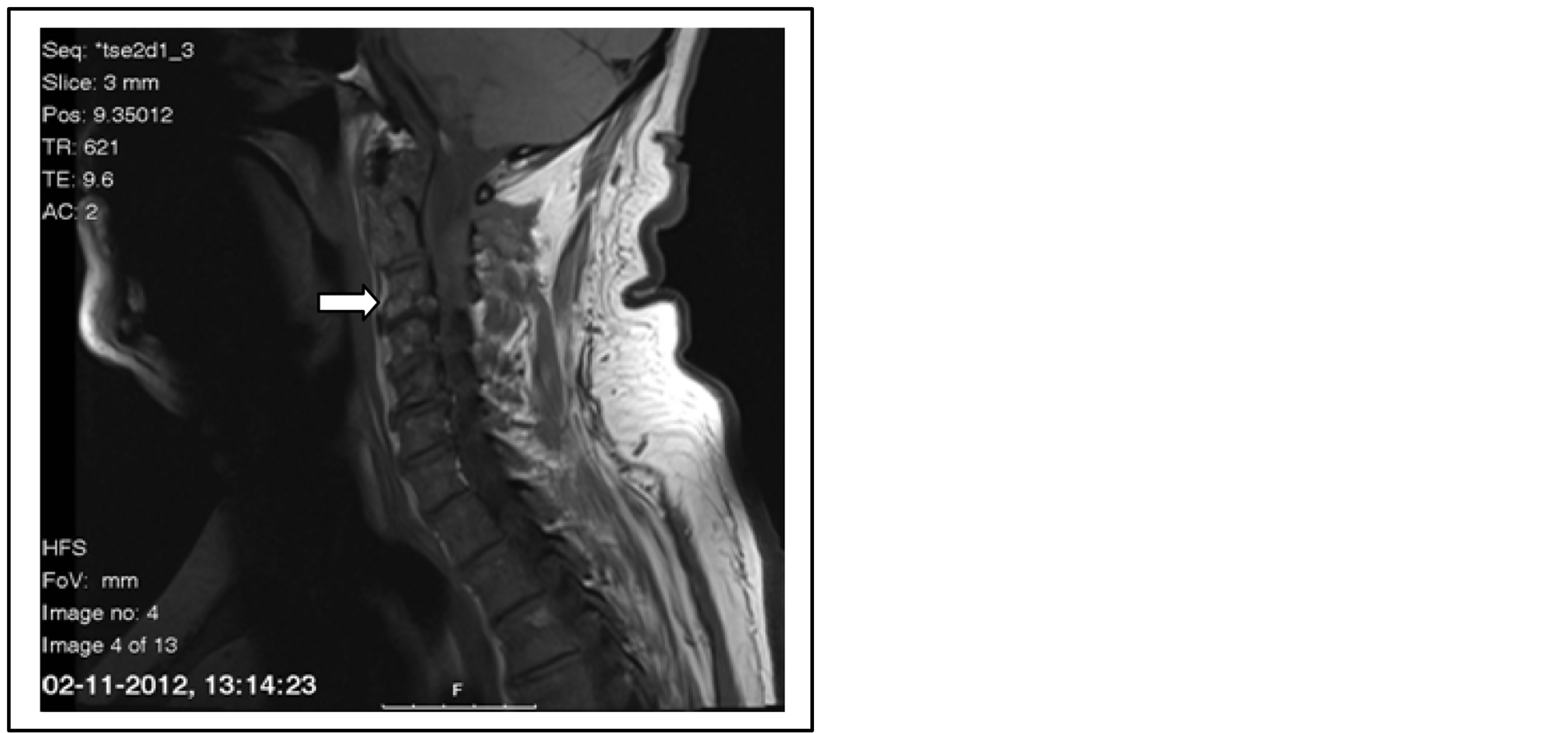
Magnetic resonance imaging (MRI) of the spine revealed signs suggestive of vertebral osteomyelitis at the level of C2-C3 with extension of the edema to the epidural space (Figure 1(a)) and signs of spondylodiscitis at the level L2-L3 (Figure 1(b)). There was no loculation of inflammatory infiltrate. A test for HIV was negative. Transthoracic echocardiography was unremarkable.
In the next few days, fever persisted and the inflammatory signs of the right leg worsened with formation of an
 (a)
(a)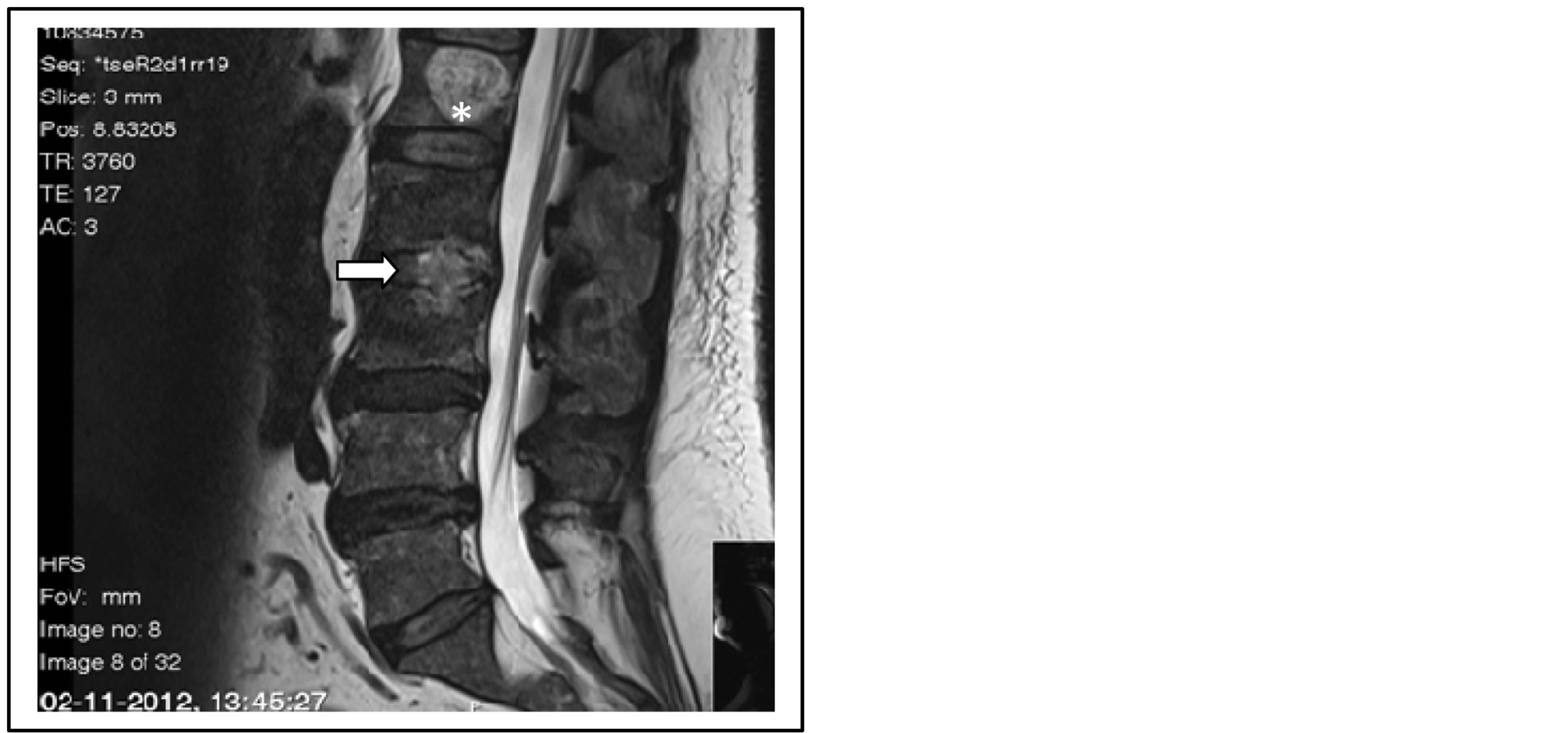 (b)
(b)
Figure 1. (a) Septic arthritis at the level of C2-C3. (b) Signs of spondylodiscitis at the level L2-L3. *Hemangioma at the level of L1.
abscess. The abscess was drained and broad-spectrum antibiotic coverage with meropenem and vancomycin was initiated. The patient was transferred to the department of neurosurgery where it was considered that only medical treatment was required.
Blood cultures subsequently grew SDSE. Isolates were resistant to tetracycline, erythromycin and clindamycin and susceptible to penicillin, cefotaxime, levofloxacin and co-trimoxazole. Antibiotic was changed to penicillin and gentamicin. During the first days, he maintained fever and infection parameters fluctuated. He repeated MRI two weeks after initiation of antibiotic that showed similar aspects noticed on the first MRI. He was transferred to the Infectious Diseases Department.
Penicillin (20 million of Units/day, divided in 6 doses) was continued for 6 weeks and gentamicin (dose adjusted according to plasma drug level) for 5 weeks. There was clinical improvement with no further episodes of fever, with significant reduction of the pain and normal neurological status. Leg ulcer also healed completely. The infection parameters declined. A repeat MRI of the spinal column was done after four weeks of therapy. It showed less inflammatory infiltrate on the epidural space. The patient was discharged and continued in ambulatory 2 weeks of therapy with amoxicillin plus clavulanic acid as well as functional rehabilitation.
3. Discussion
Vertebral osteomyelitis is an uncommon cause of back pain in adults. It usually results from hematogenous seeding of the bone. Skin and soft tissue infections, urinary tract infections, endocarditis, respiratory tract infections and indwelling catheter-associated infections are the most common primary sources [4] .
Staphylococcus aureus is responsible for 50% - 75% of all cases, but other organisms are occasionally implicated such as coagulase-negative Staphylococci, Enterobacteriaceae, Streptococci and, depending on the geographical area, Mycobacterium tuberculosis and Brucella spp. could also have etiological importance [4] .
A thorough search of the literature (under the keywords “spondylodiscitis”, “vertebral osteomyelitis” in combination with “Streptococcus dysgalactiae or Streptococcus equisimilis”) revealed twelve published cases of spondylodiscitis involving SDSE as causative agents [4] -[11] . Not all of them had known underlying diseases recognized as risk factors. The present case demonstrates the risk of older patients of developing invasive disease upon skin infection with Streptococcus dysgalactiae subsp. equisimilis, even when other risk factors are absent or well controlled (as was diabetes mellitus in this patient), suggesting that the pathogenic potential of SDSE should not be underestimated.
Whenever possible, antimicrobial therapy of vertebral osteomyelitis should be directed against an identified microorganism, which highlights the value of microbiological investigation. SDSE antibiotic susceptibility testing described in literature revealed high susceptibility to penicillin and cephalosporins but resistance to erythromycin, clindamycin, fluoroquinolones and tetracycline [1] [2] . The isolate in the presented case had similar susceptibility characteristics.
There is no good-quality evidence to support the addition of gentamicin in this clinical setting. However, the addition of gentamicin to penicillin has produced a bactericidal effect against group C Streptococci in vitro, and it was presumed a similar effect in this situation [5] .
4. Conclusion
The present case demonstrates the risk of older patients of developing invasive disease upon skin infection with Streptococcus dysgalactiae subsp. equisimilis, even when other risk factors are absent or well controlled, suggesting that the pathogenic potential of SDSE should not be underestimated.
References
- Broyles, L.N., Van Beneden, C., Beall, B., Facklam, R., Shewmaker, P.L., Malpiedi, P., Daily, P., Reingold, A. and Farley, M.M. (2009) Population-Based Study of Invasive Disease Due to Beta-Hemolytic Streptococci of Groups Other than A and B. Clinical Infectious Diseases, Vol.48, 706-712. http://dx.doi.org/10.1086/597035
- Takahashi, T., Sunaoshi, K., Sunakawa, K., Fujishima, S., Watanabe, H. and Ubukata, K. (2010) Clinical Aspects of Invasive Infections with Streptococcus Dysgalactiae ssp. Equisimilis in Japan: Differences with Respect to Streptococcus Pyogenes and Streptococcus Agalactiae Infections. Clinical Microbiology and Infection, 16, 1097-1103. http://dx.doi.org/10.1111/j.1469-0691.2009.03047.x
- Richette, P., Pizzuti, P., Quillard, A., Raskine, L., Naveau, B. and Lioté, F. (2001) A Definite Case of Spondylodiscitis Caused by Streptococcus Equisimillis. Clinical and Experimental Rheumatology, 19, 587-588.
- Lestin, F., Mann, S. and Podbielsk, A. (2008) Spondylodiscitis and Paraspinal Abscess Caused by β-Haemolytic Group G Streptococci Spreading from Infected Leg Ulcers. Journal of Medical Microbiology, 57, 1157-1160. http://dx.doi.org/10.1099/jmm.0.2008/000240-0
- Kumar, A., Sandoe, J. and Kumar, N. (2005) Three Cases of Vertebral Osteomyelitis Caused by Streptococcus Dysgalactiae Subsp. Equisimilis. Journal of Medical Microbiology, 54, 1103-1105. http://dx.doi.org/10.1099/jmm.0.46061-0
- Tobias, J.H., Lee, P.Y. and Bruckner, F.E. (1992) Group G Beta-Haemolytic Streptococcal Vertebral Osteomyelitis. Journal of Infection, 25, 115-116. http://dx.doi.org/10.1016/0163-4453(92)93801-V
- Castellarin, M., Bonnet, C., Remy, M., Arnaud, M., Negrier, I., Bertin, P. and Treves, R. (1993) Spondylitis Due to Group G. Streptococcus. Journal of Rheumatology, 20, 758-759.
- Hall, M. and Williams, A. (1993) Group G Streptococcal Osteomyelitis of the Spine. British Journal of Rheumatology, 32, 342-345. http://dx.doi.org/10.1093/rheumatology/32.4.342
- Hayashi, Y., Ishii, Y., Arai, R., Obara, K., Kamada, A., Takizawa, H., Hase, I., Mashio, K., Yamada, I., Takemasa, A., Sugiyama, K., Fukushima, Y. and Fukuda, T. (2007) A Case of Group G Streptococcus Sepsis, Chest Wall Abscess, and Vertebral Osteomyelitis Mimicking a Primary Lung Cancer with Bone Metastasis. Nihon Kokyuki Gakkai Zasshi, 45, 76-80.
- Torikai, K., Yamasaki, Y., Nemoto, T., Ishii, O., Takagi, T., Takemura, H. and Matsuda, T. (2011) A Case of Acute Septic Osteomyelitis Onset Due to Streptococcus Dysgalactiae Subsp. Equisimilis in an Elderly Diabetic Patient. Kansenshogaku Zasshi, 85, 508-511.
NOTES

*Corresponding Author.

