Open Journal of Radiology
Vol.1 No.2(2011), Article ID:16516,5 pages DOI:10.4236/ojrad.2011.12007
Treatment of Organized Hematoma of the Sphenoid Sinus with Pre-Operative Embolization and Endoscopic Resection
1Department of Otolaryngology-Head and Neck Surgery, University of Washington, Seattle, USA
2Department of Pathology, University of Washington, Seattle, USA
E-mail: pbhama@gmail.com
Received September 20, 2011; revised October 26, 2011; accepted November 16, 2011
Keywords: Sphenoid Sinus Mass, Organizing Hematoma, Sinus Mass, Chronic Epistaxis
Abstract
The differential diagnosis for expansile masses of the sphenoid sinuses includes both benign and malignant lesions. We herein present a case of a 79-year-old female who presented with chronic epistaxis and an expansile soft tissue mass centered in the sphenoid sinus with erosion of the skull base. Endoscopic resection of the lesion was performed, with histopathological examination revealing organized hematoma. To our knowledge, this is the first reported case of sphenoid sinus organizing hematoma treated with pre-operative embolization followed by endoscopic excision.
1. Introduction
Organized hematoma of the paranasal sinuses is a rare non-neoplastic condition most commonly involving the maxillary sinuses. It results from transformation of an existing hematoma via neovascularization and fibrosis. The initial hematoma may be the result of trauma, vessel damage, or vascular disease [1]. Albeit benign, organizing hematoma may be locally destructive, and can erode through bone. Thus, patients may present with symptoms mimicking a benign neoplasm, or even a malignancy. In cases when organized hematoma does not erode through bone it may mimic benign disease processes such as paranasal sinus mucocele, chronic sinusitis, and sinonasal polyposis [2]. Because of the proximity of the sphenoid sinus to the sella turcica, sphenoid sinus organized hematoma may even be mistaken for pituitary adenoma.
Complete resection is necessary to exclude the presence of any neoplastic cells and to control the source of bleeding that caused the mass. Endoscopic approaches for resection of these lesions have been described in the literature [3]. Preoperative embolization of feeding arteries for organized hematoma of the maxillary sinus has also been described [4], although this approach has never been reported with the sphenoid sinus.
2. Case Report
A 79-year-old female with a past medical history of atrial fibrillation, hypertension, chronic anticoagulation, and hypothyroidism presented to her primary care physician (PCP) with a 5-week history of occipital and frontal headaches. Several days prior to her presentation, she began to note diplopia in all gazes and intermittent left sided epistaxis. An MRI was ordered by the PCP, and demonstrated an expansile mass likely centered in the left sphenoid sinus, and the patient was referred to otolaryngology. A non-contrast CT obtained for pre-operative evaluation revealed erosion of the roof, left anterior and posterior walls of the sphenoid sinus. The mass abutted the cavernous sinuses bilaterally. There was some heterogeneity of the lesion itself (Figure 1). She underwent endoscopic left sided sphenoidotomy under image guidance with biopsy of the mass several weeks later. Intraoperatively, a fleshy mass was noted in the sphenoid sinus, surrounded by polypoid mucosa. Histopathological examination from the operative biopsy was inconclusive.
The patient suffered a cerebrovascular accident on the third post-operative day, and was admitted to an outside institution for treatment. The patient returned to our clinic 4 months later with persistent symptoms of headaches, diplopia and epistaxis. A repeat CT was performed
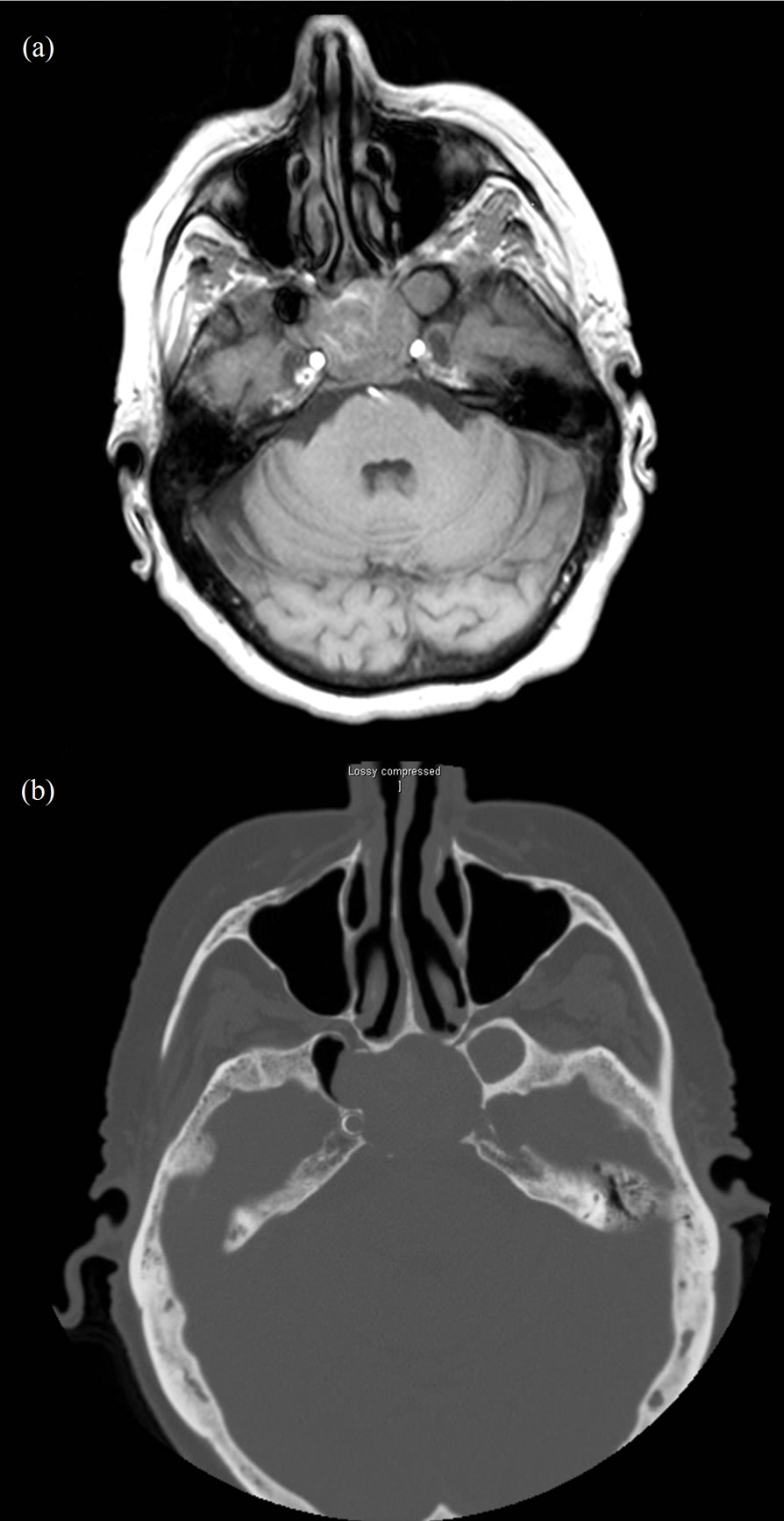
Figure 1. Initial pre-operative imaging. (a) Pre-operative T1 magnetic resonance imaging. (b) Axial non-contrast computed tomography.
(Figure 2), demonstrating enlargement of the sphenoid sinus mass, with extension into the cavernous sinus, left cerebral fissure, medial greater sphenoid wings, and into the nasopharynx and posterior ethmoid sinuses. The patient returned to the OR for repeat endoscopic biopsy under image guidance. Intraoperative findings included a necrotic-appearing mass in the posterior left nasal cavity emanating from the sphenoethmoid recess. Over 50% of the mass was decompressed, and the remainder was left in place to minimize operative time and avoid injury to the exposed internal carotid arteries and dura on both sides. Histopathologic analysis with flow cytometry was again inconclusive, demonstrating non-viable tissue with foci of granulation tissue, blood, and inflammatory de-
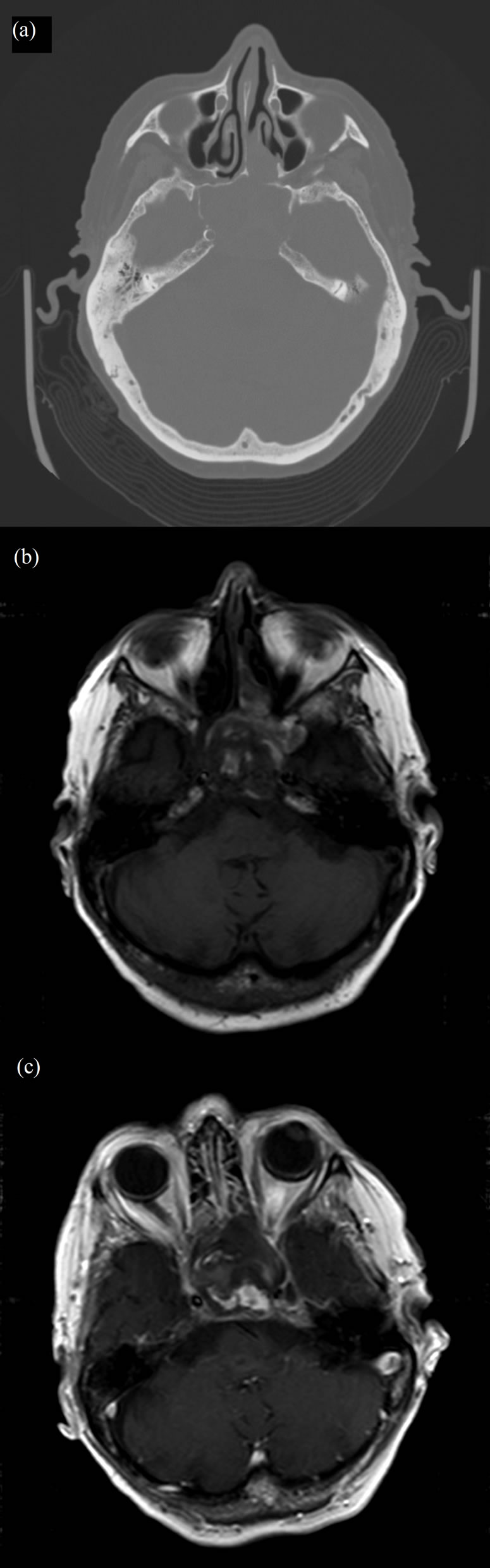
Figure 2. Pre-operative imaging. (a) Computed tomography. (b) T1 magnetic resonance imaging pre-gadolinium. (c) T1 magnetic resonance imaging post-gadolinium.
bris.
Post-operatively, the patient noted improvement in her headaches, and visual changes. She denied any further epistaxis. However, several months later she began to develop recurrent headaches and intermittent diplopia, epistaxis, as well as fatigue. She was then referred to the senior author for consultation. A repeat CT was performed demonstrating persistent sphenoid sinus mass with erosion of the clivus and extension to the carotid walls. She was taken to the OR for repeat debulking and biopsy of the mass via endoscopic image guidance.
Over 80% of the mass was successfully removed though a small rim was left adherent to the skull base. Histopathologic examination with flow cytometry was again inconclusive and demonstrated fibrinous inflammatory debris and organizing thrombus. At that time, the presumptive diagnosis was a hemangioma. The patient was also referred to rheumatology at that time to rule out other possible etiologies. The rheumatology service diagnosed her disease as a process similar granulomatosis with polyangiitis (Wedener’s) and therefore elected to treat her with Methotrexate.
She represented seven months later with persistent bloody nasal drainage, mid facial pain/pressure, and complete nasal congestion. She had stopped taking the methotrexate after only a couple weeks due to unacceptable side effects. Repeat CT was ordered demonstrating progression of the mass. The patient’s nasal bleeding became worse over the next several days, necessitating inpatient admission to control bleeding. She underwent endovascular particle embolization of the distal bilateral internal maxillary arteries without complication (Figure 3). She was taken to the OR the following day for endo-
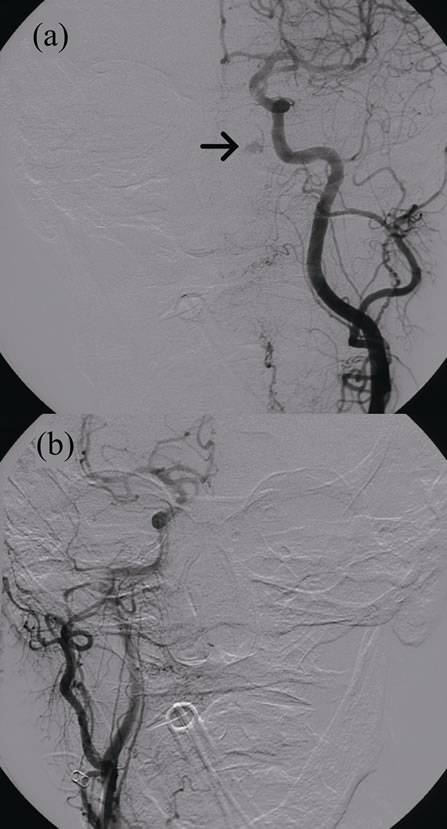
Figure 3. Embolization demonstrates a blush in the region of the sphenoid sinus (arrow). (a) Left (b) Right.
scopic resection of the mass under image guidance. Intraoperatively, the mass was found to begin at the level of the left maxillary os anteriorly, and extend to the clivus posteriorly, which had been completely eroded. The posterior, superior, and lateral walls of the sphenoid sinus were eroded. A near-total resection was achieved. A 3 cm × 3 cm defect in the skull base was noted, without CSF leak, and was reinforced with DuraGen (Integra, Plainsboro, NJ). Histopathologic analysis revealed findings consistent with an organized hematoma (Figure 4). She was discharged home on the third post-operative day after an uneventful recovery.
During her 9-month post-operative visit, she was found to be doing quite well. Her epistaxis has completely resolved. Fiberoptic nasal endoscopy revealed only polypoid mucosa in the sphenoid sinus without evidence of recurrence of the organizing hematoma. However, she returned to clinic 2 months later for follow-up and was found to have recurrence of her mass in the sphenoid sinus. After examination in the clinic, she began to bleed from the mass, and was therefore admitted for observation and MRI to rule-out encephalocele. Imaging did not demonstrate encephalocele, and the patient was thus discharged home the following day. She presented again several weeks later with epistaxis, and was therefore taken to the operating room for control of epistaxis and repeat excision of her organized hematoma. Histological review again demonstrated organizing hematoma. She recovered uneventfully, and on follow-up 4 months later was found to have no evidence of recurrence on fiberoptic examination. During this time period she continued to be anticoagulated with Coumadin, and had poorly controlled hypertension.
3. Discussion
To our knowledge, only one case of organized hematoma of the sphenoid sinus has been described in the literature to date. The authors of that study were suspicious that the lesion represented a pituitary neoplasm. Endoscopic subtotal transsphenoidal excision of the lesion was performed. The mass was adherent to exposed dura and the prominence of the carotid artery, and therefore, the authors left behind some fibrous attachments, similar to the situation we encountered. They reported no recurrence at three-month follow-up. Embolization was not used in this patient’s treatment [3]. Our reasoning for using embolization was to attenuate intraoperative bleeding, but after recognizing the theorized pathogenesis of organized hematoma, we have concluded that embolization may have actually decreased risk for recurrence.
The exact etiology for organized hematoma of the sinonasal cavities is not known, but several authors have
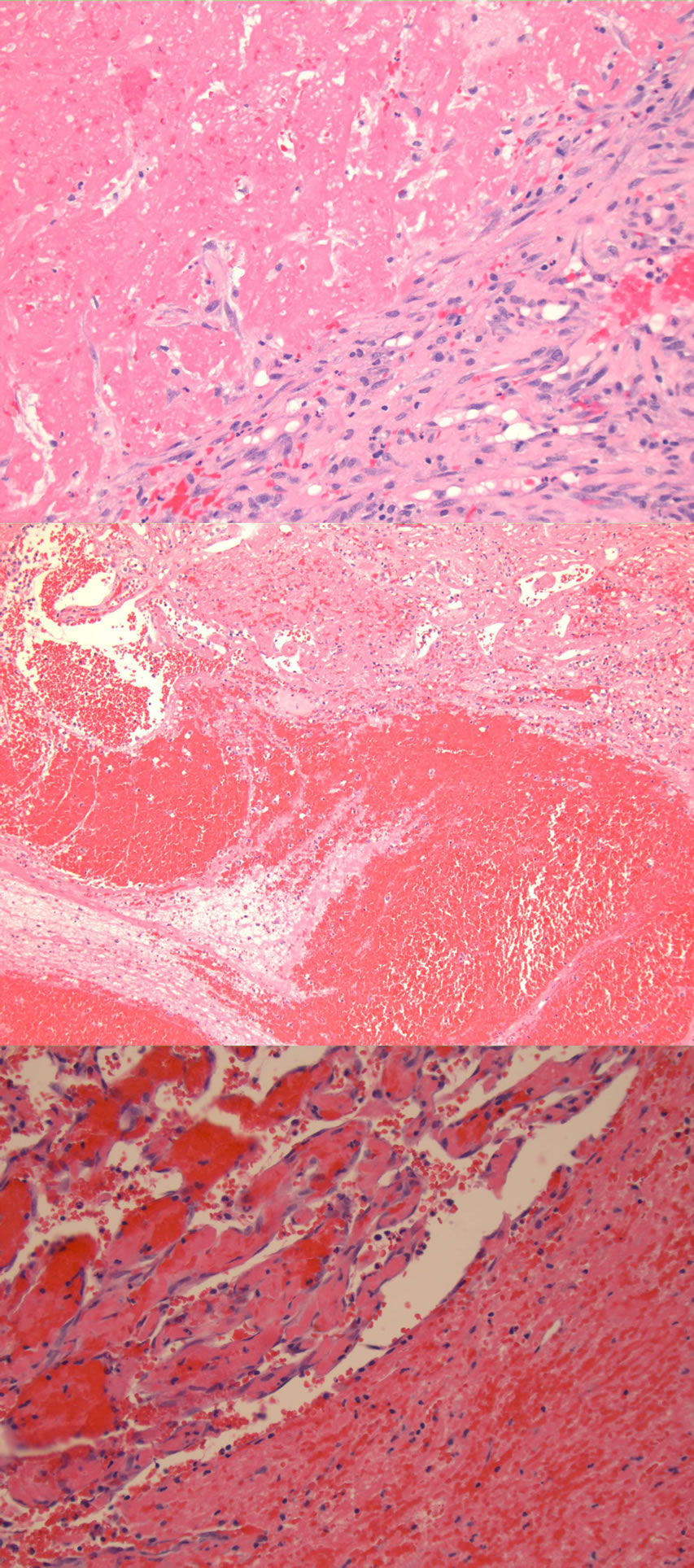
Figure 4. Pathology: Grossly, the tissue submitted for pathology was hemorrhagic and friable. On microscopic exam, the specimens consisted of predominantly blood clot with lines of Zahn and areas with cellular organization. Some areas were very cellular and resembled granulation tissue with sparse admixed inflammation. Other foci of organization had the appearance of papillary endothelial hyperplasia.
suggested that propagation of the hematoma follows several steps basic steps. Regardless of the initial etiology of bleeding, the enclosed hematoma cannot be absorbed due to the lack of ventilation and drainage. Fibrosis occurs, along with neovascularization, eventually leading to more intracapsular bleeding, and proliferation of the hematoma [3]. It seems plausible that embolization of the arteries supplying blood flow to the region could help prevent neovascularization, thereby halting the process. The patient described in this paper was anticoagulated on a long-term basis, which could possibly account for her initial bleeding. Moreover, she remained anticoagulated and had relatively poorly controlled hypertension during much of her post-operative course, which may have contributed to her epistaxis and likely recurrence of the mass.
Diagnosis of these lesions is difficult, as they can mimic neoplastic disease, both benign and malignant. Imaging is important to help define involved anatomic landmarks, and to assess for progression of disease, as in the case described above. Computed tomography (CT) of paranasal sinus organized hematoma may show bony erosion and mucoperiosteal thickening. CT with intravenous (IV) contrast can demonstrate heterogeneous enhancement in a patchy distribution, likely representing areas of neovascularization [5]. Magnetic resonance imaging (MRI) findings include paranasal sinus mucosal thickening, which enhances on T1 images with contrast, and is high-intensity of T2. Centrally, the lesion may have low intensity on T1 and high intensity on T2. Some authors have found that MRI is superior to CT for several reasons in determining the margins and extent of organizing hematomas [6].
Histopathological analysis reveals a relatively acellular fibrinous mass with some intact erythrocytes and a predominance of organizing blood clot. Spindle cell areas may represent reactive fibrosis. Vascular proliferation is present, and there is no evidence for neoplastic disease. These findings help distinguish organizing hematoma from malignant processes.
Organizing hematoma of the paranasal sinuses is a rare disease process with an etiology that has yet to be determined. Involvement of the sphenoid sinus is even more rare, with this case representing only the second report in the literature. Diagnosis can be difficult, as these lesions can mimic malignant processes by eroding through bone. Nonetheless, in patients with complaints of epistaxis and mass effect in the paranasal sinuses, organized hematoma should be considered in the differential diagnosis. Workup includes CT or MRI, and use of IV contrast can be particularly helpful in cases where organized hematoma is suspected. Treatment involves complete surgical excision. Pre-operative embolization may likely help decrease intraoperative bleeding and risk for recurrence.
4. Author Comments
G. E. D. “This publication was made possible by Grant Number KL2 RR025015 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH). Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NCRR or NIH”.
5. References
[1] B. Lee, H. Park and S. Heo, “Organized Hematoma of the Maxillary Sinus,” Acta Oto-Laryngologica, Vol. 123, No. 7, 2003, pp. 869-872. doi:10.1080/00016480310002492
[2] M. A. Salam and E. Whitehead, “Large Maxillary Antral Mucocele Presenting with Facial Asymmetry,” The Journal of Laryngology and Otology, Vol. 107, No. 5, 1993, pp. 451-452. doi:10.1017/S0022215100123412
[3] T. Nakagawa, Y. Kawai, T. Sakamoto and J. Ito, “Organised Haematoma of the Sphenoid Sinus Mimicking a Pituitary Tumour,” The Journal of Laryngology and Otology, Vol. 124, No. 1, 2010, pp. 83-85. doi:10.1017/S002221510900574X
[4] G. Omura, K. Watanabe, Y. Fujishiro, Y. Ebihara, K. Nakao and T. Asakage, “Organized Hematoma in the Paranasal Sinus and Nasal Cavity—Imaging Diagnosis and Pathological Findings,” Auris Nasus Larynx, Vol. 37, No. 2, 2010, pp. 173-177. doi:10.1016/j.anl.2009.06.009
[5] H. Lee, W. Smoker, B. Lee, S. Kim and K. Cho, “Organized Hematoma of the Maxillary Sinus: CT Findings,” American Journal of Roentgenology, Vol. 188, No. 4, 2007, pp. 370-373. doi:10.2214/AJR.05.1479
[6] E. Kim, H. Kim, S. Chung, et al., “Sinonasal Organized Hematoma: CT and MR Imaging Findings,” American Journal of Neuroradiology, Vol. 29, No. 6, 2008, pp. 1204- 1208. doi:10.3174/ajnr.A1042

