Open Journal of Obstetrics and Gynecology
Vol.3 No.4A(2013), Article ID:33234,8 pages DOI:10.4236/ojog.2013.34A004
Surgical and non-surgical education practices in female pelvic medicine and reconstructive surgery fellowships within the United States
![]()
1Department of Obstetrics and Gynecology, Mayo Clinic, Rochester, USA
2Department of Obstetrics and Gynecology, Hurley Medical Center, Michigan State University College of Human Medicine, Flint, USA
Email: *occhino.john@mayo.edu
Copyright © 2013 John A. Occhino et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received 9 March 2013; revised 10 April 2013; accepted 17 April 2013
Keywords: Education; Fellowship; Female Pelvic Medicine and Reconstructive Surgery; Surgical Procedures; Training
ABSTRACT
Data are scarce regarding surgical and non-surgical education in accredited Female Pelvic Medicine and Reconstructive Surgery (FPMRS) fellowships in the United States. We compared surgical and non-surgical and education among training programs and expected surgical comfort level with pelvic reconstructive procedures from the perspective of the fellow and program director. An online survey was distributed to program directors and fellows from the 39 accredited FPMRS fellowships at the time (2010). Domains evaluated in the survey were academic education requirements; surgical approaches to prolapse and to incontinence; other surgical procedures; and research and publication expectations. In total, forty fellows from 21 programs and directors from 27 programs responded. The most common surgical procedures performed for apical, anterior, and posterior prolapse were uterosacral ligament suspension, native tissue anterior colporrhaphy, and posterior colporrhaphy, respectively. Differences in perceived surgical comfort level were seen for coccygeus suspension, graftreinforced posterior colporrhaphy, rectus fascial sling, urethral bulking agent, cystoscopic ureteral stent placement and bowel repair. A greater proportion of program directors reported that fellows would be comfortable performing these procedures upon graduation than the proportion reported by the fellows themselves. Differences exist in FPMRS training nationwide, however, responding fellows appeared to be trained in multiple approaches to prolapse repair. Differences were seen in surgical comfort level as perceived by fellows and program directors.
1. INTRODUCTION
Training across surgical specialties has seen considerable change over the past decade. With the introduction of duty-hour restrictions in the United States, the increasing popularity and capabilities of surgical simulation, and the shift toward subspecialization, the environment in which residents and fellows acquire surgical knowledge provides many new challenges [1,2]. A movement away from a solely apprenticeship model to an integrated model that incorporates various educational modalities is expected to be the way of the future [3,4]. Such training likely will include laparoscopy simulation, surgical case evaluation, and didactic learning, because educational objectives are now required to include both technical skill and non-surgical patient treatment [5,6]. In the realm of gynecologic surgery, 2 major recognized fellowships have emerged: gynecologic oncology and female pelvic medicine and reconstructive surgery (FPMRS), commonly termed as urogynecology.
Since 2005, several studies have investigated FPMRS training from various points of view. However, these studies have focused primarily on the perspectives of obstetrics and gynecology residents and the residency program director, with limited evaluation of the FPMRS fellow themselves [7,8]. Overall, investigators have concluded that resident surgical training in a number of common pelvic reconstructive procedures is insufficient for independent surgical practice post residency [7,9]. Currently, little data are available regarding FPMRS fellows’ and fellowship program directors’ perspectives on surgical and non-surgical education and proficiency.
Certain core competencies are required for FPMRS fellowship program accreditation in the United States, such as surgical and non-surgical management of pelvic organ prolapse and urinary incontinence, education in pelvic anatomy and physiology, and coursework in statistics and epidemiology [10,11]. The approach to surgical correction of pelvic organ prolapse may vary substantially from program to program. There is yet to be standardization in surgical training and therefore variations among training programs may include a preference toward vaginal native tissue repair, vaginal repair with graft augmentation, use of prefabricated mesh kits, laparoscopic and robotic approaches, and open abdominal approach. We believe that graduating fellows are trained in the management of a variety of pelvic floor disorders, but we are seeking information on the predominant techniques taught by different programs for the management of these problems. Surgical training in FPMRS currently faces a time of marked change, with the recent recognition of the subspecialty by the American Board of Medical Subspecialties and institution of a formalized process for board certification. The objective of this study was to evaluate similarities and differences in surgical and nonsurgical education among accredited FPMRS fellowships in the United States and examine expected surgical comfort level of fellows from the perspective of program directors and fellow themselves.
2. METHODS
In February 2010, there were 39 accredited FPMRS fellowship programs listed on the American Board of Obstetrics and Gynecology and American Board of Urology Web sites. A 33-question, internet-based survey was distributed via email to FPMRS program directors from all US accredited American Board of Obstetrics and Gynecology/American Board of Urology FPMRS fellowships. They were contacted by e-mail and asked to participate in the survey. A link to the survey was provided in the e-mail, along with a request for further distribution to their respective fellows, as a comprehensive list of fellow emails was not available. An e-mail reminder was provided to all non-responding fellowship directors and those with non-responding fellows 2 weeks later.
Having fellowship directors and fellows complete the survey allowed for comparison of their responses on identical topics. Information regarding required educational courses, additional degrees, and off-service rotations was obtained solely through program director responses.
Fellow and program director surveys were identical except the fellow survey evaluated expected surgical competence of themselves upon graduation, while the director’s survey evaluated expected competence of the fellows upon graduation. Each question was multiple choice with a section for write-in documentation if an answer was not listed (Figure 1). Specifically, the survey evaluated surgical procedure preferences for repair of primary and recurrent pelvic organ prolapse in the anterior, apical, and posterior compartments. Training in laparoscopy and robotics was also addressed. General educational questions included the option or requirement for completion of a master’s degree during the fellowship, anticipated number of publications on completion, and required off-service clinical rotations. Career plans after completion of the fellowship were evaluated with respect to planning a career in academics, private practice, or a hybrid of the two areas. The study was approved by the Mayo Clinic Institutional Review Board.
After 1 month, the survey was closed and responses were analyzed. Differences between the perceptions of directors and fellows on various procedures were compared through χ2 or Fisher exact test where appropriate.
3. RESULTS
3.1. Population Characteristics
Of the 39 accredited FPMRS fellowship programs listed on the American Board of Obstetrics and Gynecology (ABOG) and American Board of Urology (ABU) web sites, 27 program directors (69%) and 40 fellows (approximately 37%) completed the online survey. The estimated number of FPMRS fellows nationwide was 108; however, a comprehensive list was not available through ABOG/ABU. The fellows who responded represented 21 different programs, or 54% of the 39 accredited programs at the time of the survey. Almost all of the responding fellows (39 (97.5%)) completed residency training in obstetrics and gynecology. The remaining fellow had a urology background. Fifteen (37.5%) were firstyear fellows; 9 (22.5%), second-year fellows; and 16 (40.0%), third-year fellows. Two of the 15 first-year fellows (12.5%) had not begun clinical rotations at the time of survey completion, leaving 95% (38/40) of responding fellows having fellowship clinical experience.
3.2. Surgical Training
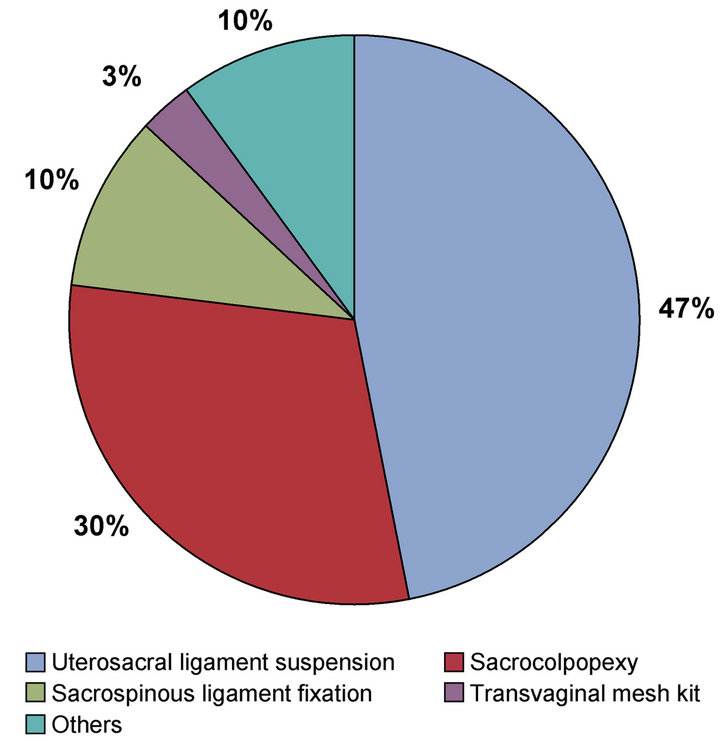
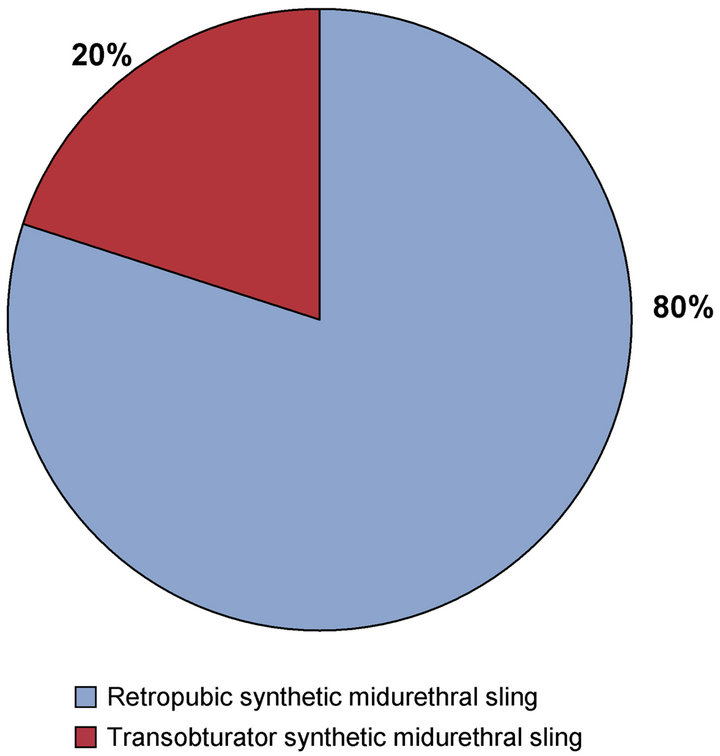
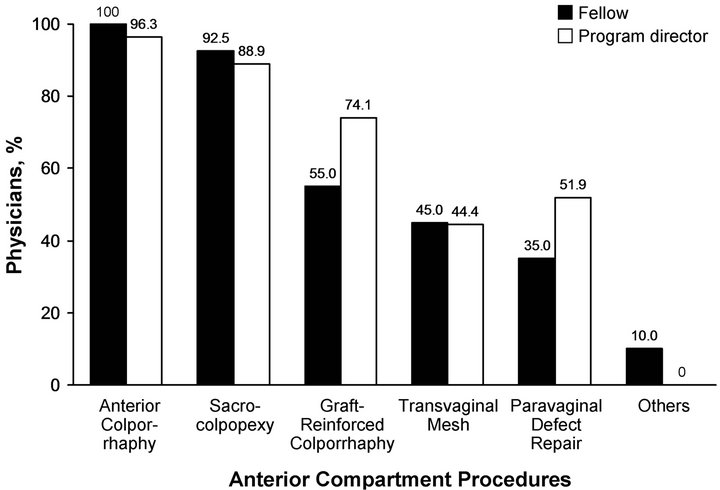
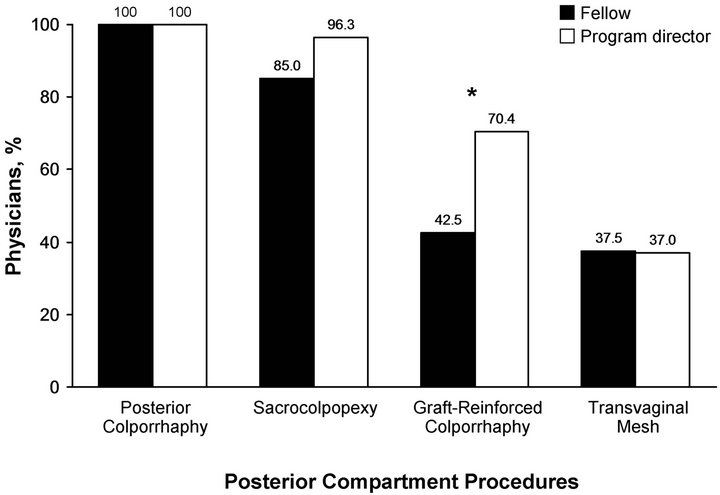
Responses from fellows were used to determine the most common surgical procedures for treatment of pelvic organ prolapse. Apical compartment prolapse was most commonly treated with transvaginal uterosacral ligament suspension followed secondly by sacrocolpopexy (Figure 2(a)). Anterior and posterior compartment prolapses were most commonly treated with colporrhaphy (Figures 2(b) and (c)). Midurethral sling was the most common treatment for stress urinary incontinence, with 80% of fellows primarily using retropubic slings and 20% using transobturator slings (Figure 2(d)). The median number of surgeries performed per week by the fellow as the primary surgeon was 3 to 5 per compartment; however, this number varied from the category “0 - 2” to “≥9” (Figure 3). Fellows were asked which procedures
Figure 1. Copy of the fellowship education survey.
 (a)
(a)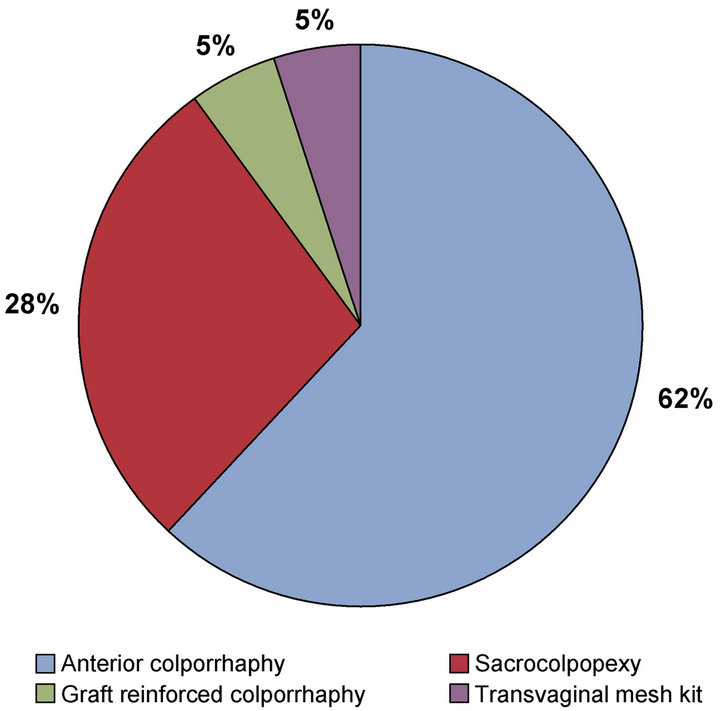 (b)
(b)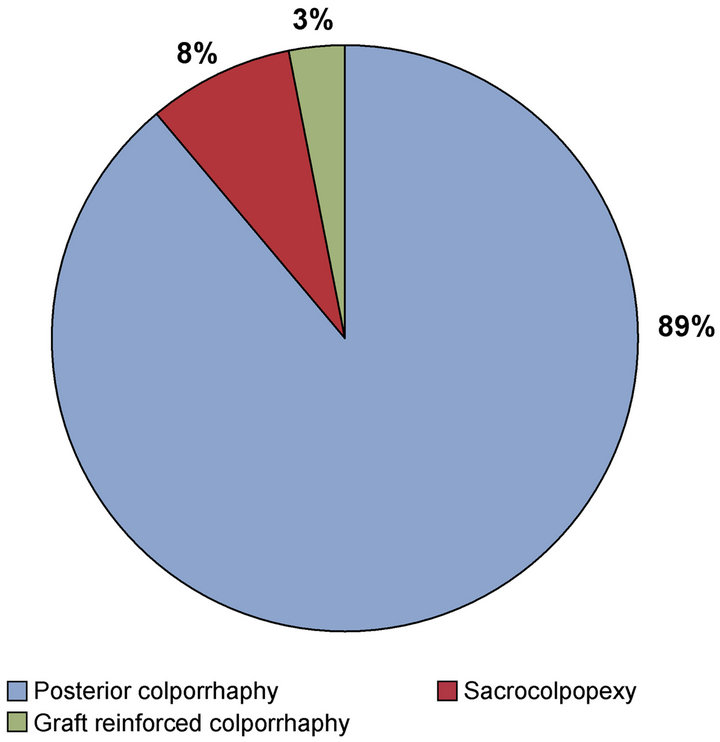 (c)
(c)
 (d)
(d)
Figure 2. The most common prolapse procedures by compartment, as reported by fellows: (a) Procedures for apical prolapse; (b) Procedures for anterior compartment prolapse; (c) Procedures for posterior compartment prolapse; (d) Procedures for stress urinary incontinence (see following page).
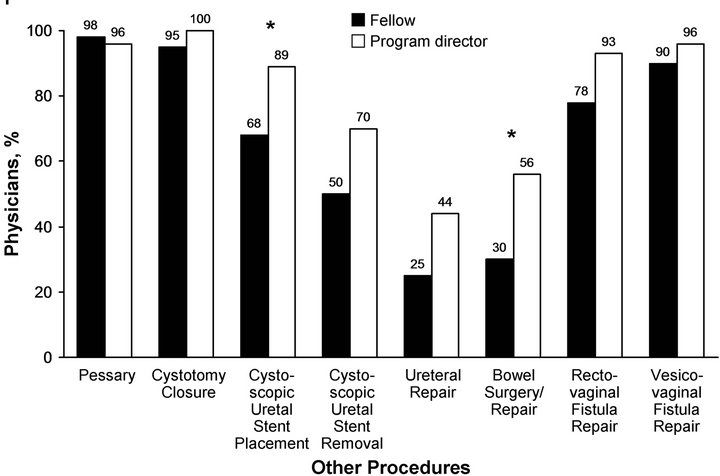
for apical prolapse, anterior prolapse, posterior prolapse, stress urinary incontinence, and refractory urgency, frequency, and urge incontinence they expected to feel comfortable performing on completion of their fellowship. Other common urogynecologic procedures were also evaluated (e.g., pessary fitting, ureteral stent placement). Program directors were asked identical questions regarding the surgical comfort level of their graduating fellows, and the answers were compared. Significant differences were seen in responses to the following questions: “other” procedures for apical prolapse (“other” defined as apical procedures aside from uterosacral ligament suspension, sacrospinous ligament fixation, sacrocolpopexy, and transvaginal mesh kit), graft-reinforced posterior colporrhaphy, rectus fascia sling, urethral bulking agent, bladder instillation, cystoscopic ureteral stent placement, and bowel surgery/repair (Figures 4 (a)-(f)). In all instances, a greater proportion of program directors reported that fellows would be comfortable performing these procedures upon graduation than the proportion reported by the fellows themselves. Training in laparoscopic and robotic surgery as part of fellowship curriculum was noted by 69.2% and 75.0% of fellows, respectively. The majority of programs required off-service rotations, with 89% requiring time with urology and colorectal surgery. Other rotations included gastroenterology, physical medicine and rehabilitation, geriatrics, plastic surgery, and gynecologic oncology. De-

Figure 3. Description of the average number of surgeries performed by fellows per week.
spite no fellowship programs incorporating an intensive care unit rotation, 28% of fellowship directors believed that this rotation would be beneficial.
3.3. Educational/Didactic Requirements
Educational components beyond surgical training varied across fellowship programs, and program director responses were used for the evaluation of these components. Of the responding programs, 52% offered a master’s degree as part of the fellowship. Formal education in statistics and epidemiology was reported in 100% and 89% of programs. Formal classes in research protocol development were offered at 63% of fellowships, with less common offerings including anatomy in 30% and medical ethics in 22% of programs.
3.4. Post-Training Employment
Similar expectations for employment after fellowship graduation were noted between fellows and program directors. Fifty-two percent of fellows and 44% of program directors anticipated fellows would pursue academic careers, while 40% of fellows and 52% of directors anticipated pursuit of a hybrid of academic and private practice. Only 8% of fellows and 4% of directors anticipated pursuit of private practice.
3.5. Obstetric Call Coverage and Academic Productivity
The survey’s final questions addressed obstetrical call and anticipated publications. Just over half (52%) of responding fellows provided obstetrical call during their fellowship. This service was an institutional requirement in 67%, an institutional option in 9%, and locum tenens in 29% of the programs. With respect to academic productivity, the median number of expected publications during fellowship was identical between fellows and program directors at 4 to 7 (answer options were ≤3, 4 - 7, 8 - 10, and >10).
4. DISCUSSION
Graduate medical education has been met with many challenges in recent years, with changes affecting trainees at both residency and fellowship levels. Changing of resident duty hours, decreasing financial reimbursement, and continual strides to improve patient safety have made the challenge of teaching medicine, and in particular surgery, even harder. Such external influences have changed the current paradigm of medical and surgical education across nearly all specialties, with more emphasis being put on simulation and virtual surgery trainers. As the field of medicine becomes more subspecialized, residencies and fellowships must continue to maintain high-quality education.
The aim of this study was to evaluate surgical and nonsurgical aspects of training in FPMRS fellowships in the United States. We sought to determine similarities and differences in approaches to common problems of this area of medicine that are encountered by pelvic surgeons (e.g., pelvic organ prolapse, urinary incontinence). We also evaluated expected surgical competency on fellow graduation from the viewpoint of the student (fellow) and the teacher (fellowship program director). Published data are limited on this topic. In 2008, Kenton et al. [9] evaluated the comfort level of recent obstetrics and gynecology graduates in performing reconstructive pelvic surgery procedures on residency completion. They compared responses from graduates with the expectations of the residency director and found inconsistencies. Findings showed residency directors more often expected their graduates to feel comfortable performing various pelvic reconstructive surgery procedures independently than did the graduates themselves.
These results are similar to those found in the present study of FPMRS fellows and several urogynecologic procedures. The results included various techniques for apical suspension, graft-reinforced posterior colporrhaphy, rectus fascia sling, urethral bulking agents, cystoscopic ureteral stent placement, and bowel surgery and repair. Trends in laparoscopy continue to change in the field of urogynecology. We found that more fellows are getting trained in robotic surgery than traditional laparoscopy (75% vs 69%). Reasons for this finding were not investigated, but one can speculate that increased availability of the robotic surgical system has had a role in this change. Currently, many institutions are implementing a formal robotic surgery curriculum into gynecologic surgery education [12,13].
Off-service rotation requirements varied among programs. Most included urology and colorectal surgery; however, variability was considerable in the time spent on these rotations, with a range from less than 2 weeks
 (a)
(a)
 (b)
(b)
 (c)
(c)
 (d)
(d)
 (e)
(e)
 (f)
(f)
Figure 4. Perspectives of program directors vs fellows regarding expected competency in performing the procedures on completion of fellowship. (a) Apical prolapse; (b) Anterior compartment prolapse; (c) Posterior compartment prolapse; (d) Stress urinary incontinence; (e) Recurrent urinary urgency, frequency, and/or urge incontinence; (f) Other procedures. Asterisk indicates a statistically significant difference (P < 0.05).
to more than 9 weeks. Less common requirements included rotations in plastic surgery and gynecologic oncology. Although no responding programs had a rotation in intensive care medicine, 28% of program directors believed it would be beneficial for their fellows. Similar to other obstetrics and gynecology fellowships, FPMRS includes an emphasis on research and education. Most institutions required minimal classes in statistics and epidemiology, while other centers required a complement of academic courses that culminated in a master’s degree. Pelvic anatomy was offered at only 30% of responding institutions, despite changing trends in anatomy education during medical school and residency [14].
We found similarities among training programs as well. Vaginal apex suspension was accomplished by uterosacral ligament suspension or sacrocolpopexy in more than 75% of programs. Most programs used traditional colporrhaphy for the management of posterior compartment prolapse. Midurethral slings were the only procedures recorded for treatment of stress urinary incontinence, with the majority using retropubic, synthetic slings.
The FPMRS stands at a crossroads of contemporary medical change because it is the first obstetrics and gynecology fellowship to receive accreditation from the Accreditation Council of Graduate Medical Education instead of ABOG.
General requirements for surgical and nonsurgical education must be met in order to have a formalized fellowship; however, there exists much variability in what graduates are being taught. This variability extends from surgical approaches to pelvic prolapse repair to formal class work in medical ethics. A more thorough understanding of what current fellows and program directors believe are the strengths and weaknesses of their programs should be achieved. It also is necessary to understand the variations in surgical and non-surgical education, because this understanding will allow us to improve the training of future fellows [15]. Universally accepted educational objectives and program requirements are also necessary to formalize a written and oral board examination.
Study strengths include a novel evaluation of the FPMRS fellowship from the perspective of the fellow and the fellowship director, because prior research had been focused at the residency level only. There are no current available data assessing surgical and non-surgical teaching in accredited FPMRS fellowships. Also, the study findings provided insight into the clinical and nonclinical aspects of fellowship, both of which are important for a complete understanding of the state of contemporary training. Weaknesses include the small numbers of responses, particularly with the fellows and urology-based programs. However, because fellows and directors were given the option of identifying their current program in the final question of the survey, it is known that at least 21 fellowship programs were represented by the fellows responding, which is greater than 50% of the accredited programs.
5. CONCLUSION
As FPMRS journeys into a new era of accreditation and formalized training, a better understanding of the current state of fellowship education and the variation of practice and educational opportunities nationwide is necessary to establish the best-possible teaching and learning environment for future trainees.
REFERENCES
- Goff, B.A. (2008) Changing the paradigm in surgical education. Obstetrics & Gynecology, 112, 328-332. doi:10.1097/AOG.0b013e3181802163
- Karram, M.M. (2008) The future of surgical training in the field of urogynecology and female pelvic floor surgery. International Urogynecology Journal and Pelvic Floor Dysfunction, 19, 1591. doi:10.1007/s00192-008-0746-0
- Julian, T.M. and Rogers, R.M. (2006) Changing the way we train gynecologic surgeons. Obstetrics & Gynecology Clinics of North America, 33, 237-246. doi:10.1016/j.ogc.2006.01.005
- Walter, A.J. (2006) Surgical education for the twentyfirst century: Beyond the apprentice model. Obstetrics & Gynecology Clinics of North America, 33, 233-236. doi:10.1016/j.ogc.2006.01.003
- Beard, J.D., Marriott, J., Purdie, H. and Crossley, J. (2011) Assessing the surgical skills of trainees in the operating theatre: A prospective observational study of the methodology. Health Technology Assessment, 15, 1-162.
- Schreuder, H.W., Oei, G., Maas, M., Borleffs, J.C. and Schijven, M.P. (2011) Implementation of simulation in surgical practice: Minimally invasive surgery has taken the lead: The Dutch experience. Medical Teacher, 33, 105-115. doi:10.3109/0142159X.2011.550967
- Schimpf, M.O., Feldman, D.M., O’Sullivan, D.M. and LaSala, C.A. (2007) Resident education and training in urogynecology and pelvic reconstructive surgery: A survey. International Urogynecology Journal and Pelvic Floor Dysfunction, 18, 613-617. doi:10.1007/s00192-006-0203-x
- Sultana, C.J., Kenton, K., Ricci, E. and Rogers, R.G. (2007) The state of residency training in female pelvic medicine and reconstructive surgery. International Urogynecology Journal and Pelvic Floor Dysfunction, 18, 1347-1350. doi:10.1007/s00192-007-0329-5
- Kenton, K., Sultana, C., Rogers, R.G., Lowenstein, T. and Fenner, D. (2008) How well are we training residents in female pelvic medicine and reconstructive surgery? American Journal of Obstetrics & Gynecology, 198, 567. e1-e4.
- Drutz, H.P. (2010) IUGA guidelines for training in female pelvic medicine and reconstructive pelvic surgery (FPM-RPS): Updated guidelines 2010. International Urogynecology Journal, 21, 1445-1453.
- The American Board of Obstetrics and Gynecology, Inc. and The American Board of Urology, Inc. (2011) General and special requirements for graduate medical education in the subspecialty of female pelvic medicine and reconstructive surgery. http://www.med.uc.edu/obgyn/Libraries/Documents/GSR-FPM_4-11_Internet_Version.sflb.ashx
- Lee, P.S., Bland, A., Valea, F.A., Havrilesky, L.J., Berchuck, A. and Secord, A.A. (2009) Robotic-assisted laparoscopic gynecologic procedures in a fellowship training program. Journal of the Society of Laparoendoscopic Surgeons, 13, 467-472. doi:10.4293/108680809X12589998403921
- Geller, E.J., Schuler, K.M. and Boggess, J.F. (2011) Robotic surgical training program in gynecology: How to train residents and fellows. Journal of Minimally Invasive Gynecology, 18, 224-229. doi:10.1016/j.jmig.2010.11.003
- Heisler, C.A. (2011) Importance of adequate gross anatomy education: The impact of a structured pelvic anatomy course during gynecology fellowship. Anatomical Sciences Education, 4, 302-304. doi:10.1002/ase.235
- Blaivas, J.G. and Appell, R.A. (2000) Female pelvic medicine and reconstructive surgery fellowships. Neurourology and Urodynamics, 19, 635-636. doi:10.1002/1520-6777(2000)19:6<635::AID-NAU1>3.0.CO;2-4
NOTES
*Corresponding author.

