 Vol.3, No.4, 236-243 (2013) Journal of Diabetes Mellitus http://dx.doi.org/10.4236/jdm.2013.34036 The association of depression and perceived stress with beta cell function between African and Haitian Americans with and without type 2 diabetes Fatma G. Huffman1*, Maria Vallasciani1, Joan A. Vaccaro1, Joel C. Exebio1, Gustavo G. Zarini1, Ali Nayer2, Sahar Ajabshir1 1Department of Dietetics and Nutrition, Florida International University, Miami, USA; *Corresponding Author: huffmanf@fiu.edu 2Division of Nephrology and Hypertension, University of Miami, Miami, USA Received 16 October 2013; revised 10 November 2013; accepted 17 November 2013 Copyright © 2013 Fatma G. Huffman et al. This is an open access article distributed under the Creative Commons Attribution Li- cense, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. ABSTRACT Background: Diabetes and diabetes-related com- plications are major causes of morbidity and mortality in the United States. Depressive symp- toms and perceived stress have been identified as possible risk factors for beta cell dysfunction and diabetes. The purpose of this study was to assess associations between depression symp- toms and perceived stress with beta cell func- tion bet ween African and Haitian Americans with and without type 2 diabetes. Participants and Methods: Informed consent and data were avail- able for 462 participants (231 African Americans and 231 Haitian Americans) for this cross-sec- tional study. A demographic questionnaire de- veloped by the Primary Investigator was used to collect information regarding age, ge nder, smok- ing, and ethnicity. Diabetes status was deter- mined by self-report and confirmed by fasting blood glucose. Anthropometrics (weight, and height and waist circumference) and vital signs (blood pressure) were taken. Blood samples were drawn after 8 - 10 hours over-night fasting to measure lipid panel, fasting plasma glucose and serum insulin concentrations. The homeo- static model assessment, version 2 (HOMA2) computer model was used to calculate beta cell function. Depression was assessed using the Beck Depression Inventory-II (BDI-II) and stress levels were assessed using the Perce ived S tress Scale (PSS). Results: Moderate to severe de- pressive symptoms were more likely for persons with diabetes (p = 0.030). There were no differ- ences in perceived stress betw een ethnicity and diabetes status (p = 0.283). General linear mod- els for participants with and without type 2 dia- betes using beta cell function as the dependent variable showed no association with depressive symptoms and perceived stress; however, Hai- tian Americans had significantly lower beta cell function than African Americans both with and without diabetes and adjusting for age, gender, waist circumference and smoking. Further re- search is needed to compare these risk factors in other race/ethnic groups. Keywords: Beta Cell Function; HOMA-IR2; Type 2 Diabetes; Haitian Americans; African Am ericans; Depressive Symptoms; Perceived Stress 1. INTRODUCTION Diabetes and diabetes related complications are major causes of morbidity and mortality in the United States affecting approximately 25.8 million people, or 8.3% of the US population in 2010; these numbers are expected to rise by 2050 [1]. Approximately 43% of the popula- tion had some hyperglycemic condition and were at risk of developing diabetes [2]. As diabetes progresses, insu- lin sensitivity and beta cell function decline; albeit, the mechanisms of reductions are not fully understood [3]. Stress and depression may be risk factors for diabetes. There is evidence suggesting that beta cells have the ability to adapt to the hormonal changes produced by stressful events; however in the long term, psychological stress may induce pancreatic islet cell failure [4-6]. Insulin resistance is associated with hyperactivation of the hypothalamic-pituitary-adrenal (HPA) axis and ex- cess plasma cortisol levels that may lead to depression [7]. Other studies supported these findings, and added that increased pro-inflammatory cytokines and distur- Copyright © 2013 SciRes. OPEN AC CESS  F. G. Huffman et al. / Journal of Diabetes Mellitus 3 (2 013) 236-243 237 bances of serotonin levels increased the risk of develop- ing diabetes [8,9]. Individuals had a 37% higher risk of developing diabetes if they suffered from depressive symptoms [7,8,10]. Conversely, other studies encoun- tered no association between hyperglycemia and insulin resistance with depression [9,11,12]. Further research is needed to clarify if there are any associations between markers of diabetes and depression. The association of beta cell dysfunction with depres- sion and perceived stress is controversial. African and Haitian Americans were selected for this study for sev- eral reasons. First, there is not much evidence of how perceived stress and depressive symptoms are associated with markers of diabetes in these populations. Second, most studies do not distinguish ethnic differences among Blacks. Yet, Blacks are high-risk groups for developing diabetes and diabetes complications [13]. Several studies have indicated that depression and perceived stress may be more pronounced in Blacks as compared to the gen- eral population [14]. Finally, due to the geographical location of South Florida, we have accessed Haitian and African Americans. Therefore, the primary aim of study is to assess if there is any association between depression symptoms and perceived stress with beta cell function between African and Haitians Americans with and with- out type 2 diabetes. The results could be important to increase awareness of depression and perceived stress symptoms in Blacks at risk for diabetes and diabetes- related complications. 2. PARTICIPANTS AND METHODS 2.1. Participants This cross-sectional study was conducted between Af- rican and Haitian Americans with and without type 2 diabetes. The Institutional Review Board at Florida In- ternational University approved this study and initial data were collected 2008-2009. Written consent was obtained from the participants upon explaining the purpose and protocol of the study. For African Americans, recruitment was based on response to flyers sent from random selec- tion of generated mailing lists that were purchased from Knowledge Base Marketing, Inc., Richardson, TX 75081. These mailing lists included African Americans with and without diabetes from Miami-Dade and Broward Coun- ties, Florida. During a 1-year period, approximately 7550 letters were mailed to African Americans, with and without type 2 diabetes. Approximately 6% (n = 477) of the letters were returned due to unknown address. Re- sponse rate was 4% (n = 256). There was no mailing list available for Haitian Ameri- cans. Haitian Americans (n = 259) were recruited from multiple community sources including local diabetes educators and community health practitioners in Mi- ami-Dade and Broward Counties; Florida International University (FIU) faculty, staff and students; several resi- dential rental facilities; and advertisements that were placed in local Haitian newspapers, churches, supermar- kets and restaurants. In addition, radio advertisements on local Creole stations were aired. When the recruitment goal was achieved, recruitment efforts were stopped. Participants were interviewed on the phone. The pur- pose of the study was explained and the gender and age of the subjects were assessed. In addition, age of diagno- sis and treatment modality was obtained from those indi- viduals who reported having diabetes. Eligible individu- als’ participation was requested at the Human Nutrition Laboratory at Florida International University. Subjects participating in the study were asked not to smoke, con- sume any food or beverages except water, and not en- gage in any unusual physical activity for at least eight hours prior to their blood collection. Laboratory results revealed that twelve participants (African Americans = 4; Haitians = 8) who reported not having diabetes were re- classified as having type 2 diabetes in accordance to the American Diabetes Association standards (ADA). These participants were referred to their physicians. 2.2. Socio-Demographic Data A standardized demographic questionnaire developed by the Primary Investigator was used to collect informa- tion regarding race/ethnicity, diabetes status, age, gender, smoking, and education level. Race/ethnicity was self- reported and confirmed by interview. Diabetes status was confirmed by laboratory results (see methods). Anthro- pometric measures were taken in the Nutrition Labora- tory. Waist circumference was measured to the nearest 1 cm at a level midway between the lower rib margin and the iliac crest with a non-stretchable tape all around the body in a horizontal position. Weight measurements were taken using a SECA clinical scale and calibrating after each participant (SECA Corp, Columbia, MD). Height and weight were measured with a subject standing erect without shoes. BMI was calculated as weight (kg)/height (m2). 2.3. Blood Collection Twenty milliliters (mL) of venous blood was collected from each participant after at least 8 hours of fasting by a certified phlebotomist using standard laboratory tech- niques. Two tubes were used to collect the blood samples: a tube containing ethylenediamine tetra-acetic acid (EDTA) to analyze hemoglobin A1c and a Vaccutainer Serum Separator Tube (SST) to analyze glucose. Gly- cated hemoglobin, reported as A1C percentages, was measured from whole blood samples, with the Roche Tina Quant method by Laboratory Corporation of Amer- Copyright © 2013 SciRes. OPEN A CCESS  F. G. Huffman et al. / Journal of Diabetes Mellitus 3 (2 013) 236-243 238 ica (LabCorp, FL, US). Glucose levels were measured by hexokinase enzymatic method after complete coagulated blood had been centrifuged at 2500 RPM for 30 minutes and placed into one labeled plastic tube. Serum insulin levels were assessed by Human Insulin ELISA kit from Millipore (St Charles, MZ, US). 2.4. Determination of Beta Cell Function We calculated beta cell function using the homeostatic model assessment, version 2 (HOMA2) computer mode, which is based on the Oxford University HOMA2 calcu- lator (www.ocdem.ox.ac.uk) [15]. It accounts for varia- tions in peripheral and hepatic glucose resistance [16]. The new version, HOMA2 is designed to better match human physiology; it is an update of the HOMA1 based on modern insulin assays. The computer model, HOMA2, can be used to calculate beta cell function from radio- immunoassay insulin and paired fasting plasma glucose across a range of 1 - 2200 pmol/l for insulin, and 1 - 25 mmol/l for glucose [15]. For data analysis, subjects un- dergoing insulin treatment or have values <45 mg/dL or >450 mg/dL for plasma glucose and insulin <2.88 μIU/mL or >57.60 μIU/mL were excluded. 2.5. Psychosocial Factors Depressive symptoms were assessed using the Beck Depression Inventory-II (BDI-II) [17]. This is a self- reported, 21-item questionnaire that measures the pres- ence and severity of depressive symptoms using a 0 to 3 self-rating scale (0 being least depressed and 3 being most depressed). Summing scores for each question cal- culated a final BDI-II score. Moderate to severe symp- toms of depression was defined as BDI-II score ≥16. A cutoff point ≥16 yielded a sensitivity of 0.73 and a speci- ficity of 0.93 [18]. Stress levels were assessed using the Perceived Stress Scale (PSS) [19]. This is a 10-item scale that measures the subjects’ response to life stressors using a 4-point scale ranging from never (1) to always (4). The 10-item PSS has a higher psychometric quality than the 14-item version and it has been validated [19]. 2.6. Statistical Analysis Statistical analyses were performed using The Statis- tical Package for Social Sciences (SPSS), version 20. Data were presented as a mean ± standard deviation for general characteristics. A p value of <0.05 was consid- ered significant. Prior to analyses, all continuous vari- ables were tested for normality by the Kolmosorov- Simirnov test. Beta cell function was natural log trans- formed to achieve normality within diabetes status. De- pressive symptoms, was converted into a binary variable based on a clinical cut off [9,20]. General linear models were used to test the relationships of depression and per- ceived stress with beta cell function, as the outcome. Due to significant differences in beta cell function by diabetes status, separate models were run for each group (with and without diabetes). The clinically important covariates tested for the adjusted models were ethnicity, age, gender, ethnicity, waist circumference, education, and smoking status. A separate model for beta cell func- tion in participants with diabetes was conducted with the adjustment covariates to which ‘years with diabetes’ was added. The same general linear models were run for per- ceived stress and depressive symptoms with insulin re- sistance as the dependent variable. 3. RESULTS For this study, we had complete data for N = 462,234 without diabetes and 228 with diabetes (231 African Americans and 231 Haitian Americans). The general characteristics of the study population by ethnicity and diabetes status are shown in Tabl e 1. Haitian Americans with diabetes as compared to the other groups, were the oldest (mean age 57.8 ± 10 years), had the lowest level of education and beta cell function, as well as the highest fasted plasma glucose, hemoglobin A1C and depression score. There were no differences in perceived stress among the groups. African Americans had a high rate of ever-smoking (approximately 40%) as compared to Hai- tian Americans (approximately 6%). A difference of the means by ANOVA and post-hoc analysis showed a significant difference in depression score by ethnicity and diabetes status. Haitian Americans with diabetes scored higher (had more signs of depres- sion) (mean = 10.9 ± 7.77) than Haitians and African Americans without diabetes (mean = 7.7 ± 7.85, p = 0.001); mean = 7.1 ± 7.50, respectively (p < 0.001). The difference in depression score between Haitian and Afri- can Americans with diabetes was not significant (p = 0.156). The Chi-Squared test was used to assess depression across diabetes status. Moderate to severe depressive symptoms, an overall score of 16 or more, were more likely for the combined group of African Americans and Haitian Americans with diabetes, than without diabetes (p = 0.030). This relationships held for mild-moderate depressive symptoms or more (a score of 12 or more) (p = 0.029). There were no differences in perceived stress between ethnicity and diabetes status (p = 0.283). Ad- justed general linear models with beta cell function as the dependent variable were run separately for participants with and without diabetes. Education was tested and not retained. The final model was adjusting for age, gender, waist circumference, and smoking. Depression and per- ceived stress were not associated with beta cell function for either model with (F7,220 = 3.14, p = −0.003) or Copyright © 2013 SciRes. OPEN A CCESS  F. G. Huffman et al. / Journal of Diabetes Mellitus 3 (2 013) 236-243 Copyright © 2013 SciRes. OPEN A CCESS 239 Table 1. General characteristics of the study participants by ethnicity and diabetes. Variable AA with T2D AA without T2D HA with T2D HA without T2Dp Age (years) 54.4 ± 10.1 50.7 ± 8.5 57.8 ± 10.0 54.2 ± 11.0 <0.001 FPG (mg/dL) 147.3 ± 66.0 95.8 ± 12.9 162.6 ± 84.5 99.5 ± 16.6 <0.001 Hemoglobin A1c (%) 7.6 ± 1.9 5.9 ± 0.4 8.5 ± 2.6 5.9 ± 0.5 <0.001 Insulin (pmol/L) 16.3 ± 15.8 12.2 ± 8.9 8.9 ± 8.7 9.9 ± 5.6 <0.001 Beta cell function (HOMA2) 63.5 ± 53.9 108.5 ± 47.4 42.2 ± 46.2 93.3 ± 42.9 <0.001 Insulin resistance (HOMA2) 2.1 ± 1.5 1.6 ± 1.2 1.4 ± 1.0 1.3 ± 0.7 <0.001 Depression score* (0 - 63) 9.5 ± 9.7 7.1 ± 7.5 10.9 ± 7.8 7.7 ± 7.8 <0.001 Perceived stress (0 - 40) 20.4 ± 5.8 20.2 ± 5.7 20.1 ± 5.7 19.1 ± 6.2 0.282 Waist circumference (cm) 114.6 ± 17.5 102.1 ± 14.5 99.2 ± 11.4 96.2 ± 12.5 <0.001 Gender - - - - 0.841 Female 67 (52.3) 59 (50.0) 76 (55.1) 60 (50.4) Male 61 (47.7) 59 (50.0) 62 (44.9) 59 (49.6) Smoked >100 cigarettes (yes) 47 (36.7) 48 (40.7) 9 (6.5) 7 (5.9) <0.001 Education - - - - <0.001 <High school 22 (17.2) 16 (13.6) 74 (53.6) 48 (40.3) High school 41 (32.0) 37 (31.4)) 29 (21.0) 25 (25.0) Some college 48 (37.5) 42 (35.6) 19 (13.8) 23 (19.3) College or more 17 (13.3) 23 (19.5) 16 (11.6) 23 (19.3) Moderate to severe depressive symptoms (≥16) 23 (18.0) 15 (12.7) 23 (16.7) 12 (10.1) 0.268 AA: African Americans; HA: Haitian Americans; T2D: type 2 diabetes mellitus; FPG: fasting plasma glucose; HOMA2: homeostatic model assessment, version 2. Continuous variables are given as means ± SD and categorical variable are shown as number (%). *Depression score measures depressive symptoms. without (F7,226 = 5.32, p < 0.001) diabetes. Haitian Americans with diabetes [b = −0.431 (−0.693, −0170) p = 0.001] and without diabetes [b = −0.151 (−0.277, −0.024) p = 0.020] had lower beta cell function as com- pared to African Americans. Years with diabetes, a factor in beta cell function, was not significantly correlated with ethnicity (Spearman’s Rho = −0.054, p = 0.428); however, we ran a general linear model with just those with diabetes entering years of having diabetes with the other adjustment variables with beta cell function as the dependent variable. The relationship with ethnicity and beta cell function remained. Haitian Americans had poorer beta cell function than African Americans [b= −0.391 (−0.685, −0.098), p = 0.009]. We tested insulin resistance as the dependent variable for the same models and found neither depressive symptoms, nor perceived stress was indicative of insulin metabolism (data not shown). 4. DISCUSSION In the present study, we examined the associations between perceived stress/depressive symptoms and beta cell function in 462 African Americans and Haitian Americans with and without type 2 diabetes. To our knowledge, this is one of the few studies comparing beta cell function and psychosocial risk factors in two Black ethnicities with and without type 2 diabetes. We found no significant association of depression with beta cell function, for Blacks with or without diabetes. Our results agreed with those of Lawlor et al. [21], which demonstrated no association between insulin re- sistance, as measured by HOMA levels, and depressive symptoms in a prospective study of middle aged men. In contrast, Pearson et al. [7] concluded that depressive disorder was significantly associated with insulin resis- tance as measured by HOMA independent of demo- graphics, dietary and behavioral factors. It is important to note that the investigators measured depression disorder as opposed to depressive symptoms as measured by an index. There may be a bidirectional relationship between insulin metabolism and depression. Whether diabetes markers and its complications increase the risk of de- pression, or depression causes insulin resistance and consequently diabetes, is not known [9]. Moderate to  F. G. Huffman et al. / Journal of Diabetes Mellitus 3 (2 013) 236-243 240 severe depressive symptoms were positively associated with insulin resistance in males without diabetes for both a young cohort [9] and in older men [22]. In the present cross-sectional analysis, there was no relationship with perceived stress and beta cell function. It is important to note that risk factors for both stress and depression may overlap. Perceived overall stress caused by exposure to unfavorable environmental and lifestyle factors was positively related to insulin resistance, obe- sity, decreased adherence to treatment and medications, and therefore, poor diabetes outcomes [11,23,24]. Tho- mas et al. [10] suggested that some individuals were more susceptible to depression due to genetic as well as socioeconomic factors. In addition, racial discrimination has a negative impact on psychological well-being. The secretion of glucocorticoids during periods of stress causes hyperglycemia and it is associated with insulin resistance [25]. Novak et al. [26] found that men who reported permanent stress during many years had an in- creased risk of developing type 2 diabetes, independent of demographic, socioeconomic, clinical, and lifestyle factors. Conversely, perceived stress was associated with beta cell dysfunction in several studies [27,28]; however, stress was measured with physiological indicators as opposed to reported perceived stress. Stress may be more pronounced for minorities and economically disadvantaged individuals [14,29]. Living in a disadvantaged environment with limited access to health care produces a stressful environment and in- creases risk of depression and diabetes for African Americans living in poverty [14,29]. Several unhealthy behaviors used for coping with stress have been sug- gested that lead to negative health outcomes among Blacks [14]. Krishnan et al. [30] suggested that chronic stress may lead to insulin resistance and diabetes among Backs. In addition, perception of racism was related to increased levels of stress and poor diabetic outcomes. Wagner et al. [31] found that African Americans linked racism to decreased diabetes self-management and con- trol through negative emotions, physiological arousal, and inadequate coping mechanisms. Earlier studies, using HOMA1 were in agreement with our findings for obesity and insulin metabolism [32,33]. In our study, we found a positive relationship between waist circumference and insulin resistance and a negative relationship between waist circumference and beta cell function as measured by HOMA2. Chung et al. [5] re- ported that obesity measured by body mass index was negatively associated with beta cell function and posi- tively associated with insulin resistance as measured by HOMA1. Everson-Rose et al. [33] reported that associa- tions between depressive symptoms and insulin resis- tance were mediated through central adiposity and obe- sity, and that the relationship was significant among Af- rican American women. Although African American par- ticipants had higher beta cell function that Haitian Americans regardless of diabetes status, they also had a higher percent of obesity, as compared to Haitian Ame- ricans. Beta cell dysfunction may be a result of loss of beta cell mass, which contributes to hyperglycemia of type 2 diabetes, but is not clearly understood on a genetic and molecular level [3]. There is evidence stating that in order to maintain normal levels of blood glucose, African Americans have a compensatory increase in beta cell function; however, progressive loss of the ability to com- pensate for a decreased in insulin sensitivity increases the risk of type 2 diabetes [34]. The results of this study are in accordance with the lit- erature finding higher depression in persons with diabe- tes. Both African and Haitian Americans with diabetes were more likely to have moderate to severe depression than those without diabetes. Thomas et al. [10] reported that the diagnosis of type 2 diabetes and its complica- tions was associated with increased depression disorder independent of education and gender in a group of low-income adults. Several studies explained that unfa- vorable environmental and lifestyle factors, in combina- tion with diabetes and its complications, could lead to depression in the general population. There are several possible explanations as to why environmental factors, together with diabetes, may increase the risk of depres- sion. Depression is mainly caused by a disruption of so- cial, psychological, behavioral, and biological factors [8]. Studies reported that poor eating habits, physical inactiv- ity, low socioeconomic status and education level, smok- ing, and limited access to health care services and healthy foods were risk factors for depression [7,8,11, 29,35-37]. We found Haitian Americans with diabetes to be more likely to have moderate to severe depressive symptoms than Haitian or African Americans without diabetes. Hai- tian American participants had a lower education level as compared to African Americans and this may be a con- tributing factor. Higher levels of depression were associ- ated with limited economic and social resources in a co- hort of African American women at risk for diabetes [29]. Many Black Americans live in precarious and stressful environments, and engaged in many unhealthy behaviors to be able to cope with stress and depression [14]. Therefore, overall stressful life events may outweigh diabetes-related stress and depression. We found no dif- ference in perceived stress between the Black ethnicities or by diabetes status. Moreover, in our study of self-rated health in this cohort, we found perceived stress was higher for individuals who were younger, female, less educated, and consumed higher calories, regardless of ethnicity or diabetes status [37]. This study has several limitations. First, this was not a Copyright © 2013 SciRes. OPEN A CCESS 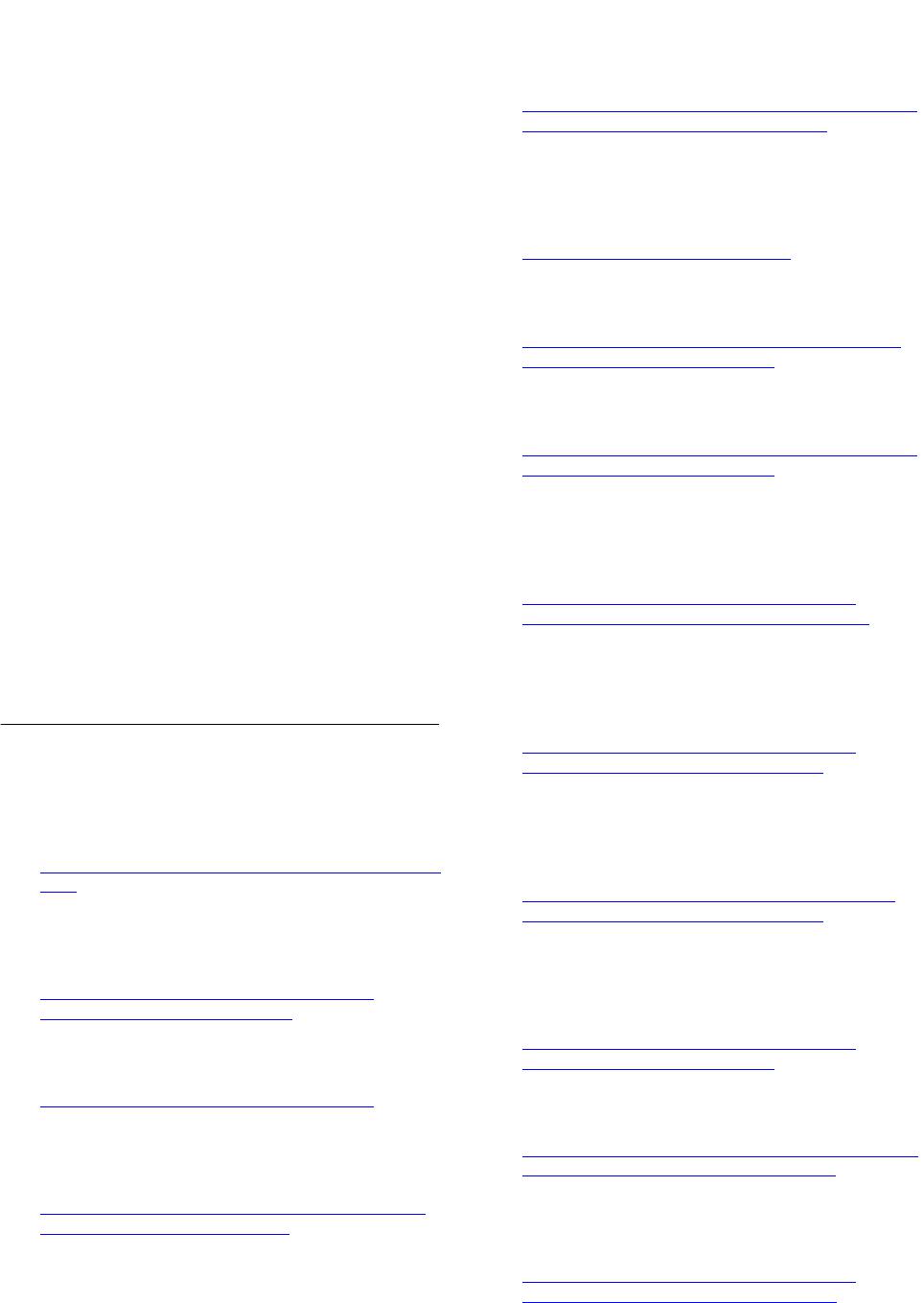 F. G. Huffman et al. / Journal of Diabetes Mellitus 3 (2 013) 236-243 241 population-based study and recruitment techniques dif- fered between African and Haitian Americans. Second the cross-sectional nature of the study limits the estab- lishment of causal relationships between variables. Third, depressive symptoms and perceived stress were self- reported, increasing subjectivity of the responses. Finally, although we included education, we did not measure or account for socioeconomic status, which may increase depressive symptoms and perceived stress in African and Haitian Americans. Despite these limitations, this study is one of the few providing data on the Black American population, differentiating Haitian and African Ameri- cans. 5. CONCLUSION In conclusion, Haitian Americans with type 2 diabetes were more likely to have severe depressive symptoms (BDS ≥ 16) than African and Haitian Americans without type 2 diabetes. Despite having smaller waist circumfer- ences, Haitian Americans had worse beta cell function than African Americans. These results suggest that early screening for insulin metabolism and depression may improve medical care of Blacks at risk for diabetes. 6. ACKNOWLEDGEMENTS This study was funded by NIH/NIDDK #1SC1DK083060-01 to cor- responding author. REFERENCES [1] Center for Disease Control and Prevention (CDC) (2013) Age-specific percentage of civilian, non-institutionalized population with diagnosed diabetes, by age, race and sex, United States, Modified, March. http://www.cdc.gov/diabetes/statistics/prevalence_nationa l.htm [2] Cowie, C., Rust, K., Ford, E., Eberhardt, M., Bryd-Holt, D., Li, C., et al. (2009) Full accounting of diabetes and pre-diabetes in the U.S. population in 1988-1994 and 2005-2006. Diabetes Care, 32, 287-294. http://www.ncbi.nlm.nih.gov/pubmed/19017771 http://dx.doi.org/10.2337/dc08-1296 [3] Kahn, S.E. (2003) The relative contributions of insulin resistance and beta-cell dysfunction to the pathophysiol- ogy of type 2 diabetes. Diabetologia, 46, 3-19. http://www.ncbi.nlm.nih.gov/pubmed/12637977 [4] Beaudry, J. and Ridell, M. (2012) Effects of glucocorti- coids and exercise on pancreatic B-cell function and dia- betes development. Diabetes Metabolism Research and Reviews, 28, 560-573. http://www.yorku.ca/mriddell/documents/dmrr2310.pdf http://dx.doi.org/10.1002/dmrr.2310 [5] Chung, J.-O., Cho, D.-H., Chung, D.-J. and Chung, M.-Y. (2012) Associations among body mass index, insulin re- sistance, and pancreatic B-cell function in Korean pa- tients with new-onset type 2 diabetes. Korean Journal of International Medicine, 27, 66-71. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3295991/ http://dx.doi.org/10.3904/kjim.2012.27.1.66 [6] Hasson, R., Adam, T., Pearson, J., Davis, J., Spruijt-Metz, D. and Goran, M. (2013) Sociocultural and socioeco- nomic influences on type 2 diabetes risk in overweight/ obese African American and Latino American children and adolescents. Journal of Obesity, Article ID: 512914. http://dx.doi.org/10.1155/2013/512914 [7] Pearson, S., Schmidt, M., Patton, G., Dwyer, T., Blizzard, L., Otahal, P. and Venn, A. (2010) Depression and insulin resistance. Diabetes Care, 33, 1128-1133. http://care.diabetesjournals.org/content/33/5/1128.long http://dx.doi.org/10.2337/dc09-1940 [8] Mezuk, B., Eaton, W., Albrecht, S. and Hill Golden, S. (2008) Depression and type 2 diabetes over the lifespan. Diabetes Care, 31, 2383-2390. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2584200/ http://dx.doi.org/10.2337/dc08-0985 [9] Timonen, M., Salmenkaita, I., Jokelainen, J., Laakso, M., Harkonen, P., Koskela, P., et al. (2007) Insulin resistance and depressive symptoms in young adult males: Findings from Finnish military conscripts. Psychosomatic Medi- cine, 69, 723-728. http://www.ncbi.nlm.nih.gov/pubmed/17942838 http://dx.doi.org/10.1097/PSY.0b013e318157ad2e [10] Thomas, J., Jones, G., Scarinci, I. and Brantley, P. (2003) A descriptive and comparative study of the prevalence of depressive and anxiety disorders in low-income adults with type 2 diabetes and other chronic illnesses. Diabetes Care, 26, 2311-2317. http://www.ncbi.nlm.nih.gov/pubmed/12882854 http://dx.doi.org/10.2337/diacare.26.8.2311 [11] Engum, A., Mykletun, A., Midthjell, K., Holen, A. and Dahl, A. (2005) Depression and diabetes: A large popula- tion-based study of sociodemographic, lifestyle, and clini- cal factors associated with depression in type 1 and type 2 diabetes. Diabetes Care, 28, 1904-1909. http://care.diabetesjournals.org/content/28/8/1904.full http://dx.doi.org/10.2337/diacare.28.8.1904 [12] Fisher, L., Mulan, J., Arean, P., Glasgow, R., Hessler, D. and Masharani, U. (2010) Diabetes depression but not cli- nical depression or depressive symptoms is associated with glycemic control in both cross-sectional and longi- tudinal analyses. Diabetes Care, 33, 23-28. http://www.ncbi.nlm.nih.gov/pubmed/19837786 http://dx.doi.org/10.2337/dc09-1238 [13] American Diabetes Association (2013) Living with dia- betes complications: African Americans and complica- tions. http://www.diabetes.org/living-with-diabetes/complicatio ns/african-americans-and-complications.html [14] Jackson, J., Knight, K. and Rafferty, J. (2010) Race and unhealthy behaviors: Chronic stress, the HPA axis, and physical and mental health disparities over the life course. American Journal of Public Health, 100, 933-939. http://www.ncbi.nlm.nih.gov/pubmed/19846689 http://dx.doi.org/10.2105/AJPH.2008.143446 Copyright © 2013 SciRes. OPEN A CCESS 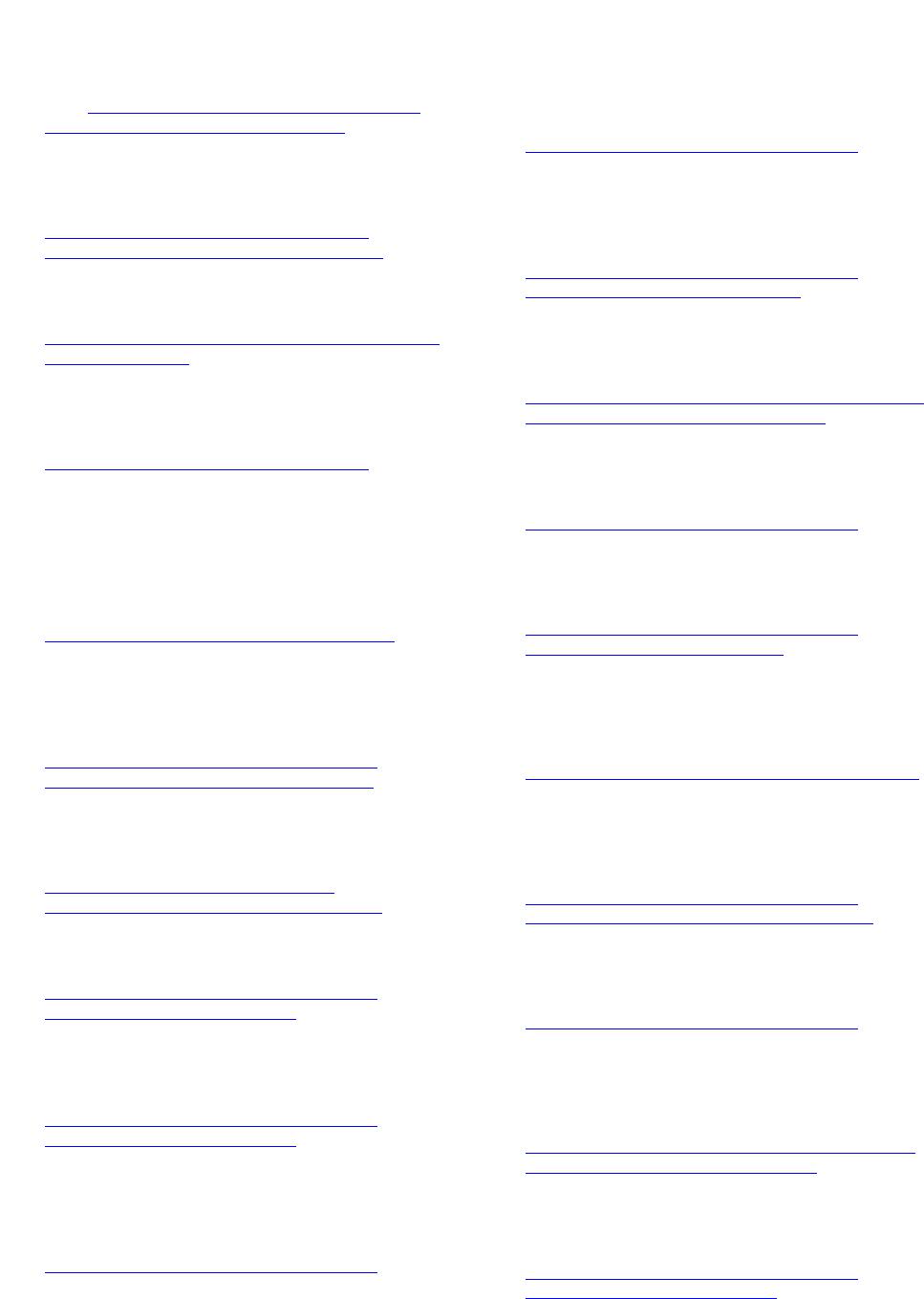 F. G. Huffman et al. / Journal of Diabetes Mellitus 3 (2 013) 236-243 242 [15] Wallace, T.M., Levy, J.C. and Matthews, D.R. (2004) Use and abuse of HOMA modeling. Diabetes Care, 27, 1487- 1495. http://www.ncbi.nlm.nih.gov/pubmed/15161807 http://dx.doi.org/10.2337/diacare.27.6.1487 [16] Rudenski, A., Matthews, D., Levy, J. and Turner, R. (1991) Understanding insulin resistance: Both glucose re- sistance and insulin resistance are required to model hu- man diabetes. Metabolism, 40, 908-917. http://www.ncbi.nlm.nih.gov/pubmed/1895955 http://dx.doi.org/10.1016/0026-0495(91)90065-5 [17] Beck, A.T., Steer, R.A. and Brown, G.K. (1996) Manual for the Beck Depression Inventory-II. Psychological Cor- poration, San Antonio. http://www.nctsn.org/content/beck-depression-inventory- second-edition-bdi-ii [18] Lustman, P.J., Clouse, R.E., Griffith, L.S., Carney, R.M. and Freedland, K.E. (1997) Screening for depression in diabetes using the Beck Depression inventory. Psycho- somatic M edicine , 59, 24-31. http://www.ncbi.nlm.nih.gov/pubmed/9021863 [19] Cohen, S. and Williamson, G. (1988) Perceived stress in a probability sample of the United States. The Social Psy- chology of Health, 13, 31-67. [20] Araya, R., Montero-Marin, J., Barroilhet, S., Fritsch, R. and Montgomery, A. (2013) Detecting depression among adolescents in Santiago, Chile: Sex differences. BMC Psychiatry, 13, 1-12. http://www.biomedcentral.com/1471-244X/13/122 [21] Lawlor, D., Ben-Shlomo, Y., Ebrahim, S., Smith, G., Stansfeld, S., Yarnell, J. and Gallacher, J. (2005) Insulin resistance and depressive symptoms in middle aged men: Findings from the Caerphilly prospective cohort study. BMJ, 330, 705-706. http://www.ncbi.nlm.nih.gov/pubmed/15684022 http://dx.doi.org/10.1136/bmj.38377.616921.F7 [22] Timonen, M., Laakso, M., Jokelainen, J., Rajala, U., Meyer-Rochow, V.B. and Keinänen-Kiukaanniemi, S. (2005) Insulin resistance and depression: Cross sectional study. BMJ, 330, 17-18. http://www.bmj.com/content/330/7481/17 http://dx.doi.org/10.1136/bmj.38313.513310.F71 [23] Pyykkönen, A., Raikkonen, K., Tuomi, T., Eriksson, J., de Groop, L. and Isomma, B. (2010) Stressful life events and the metabolic syndrome. Diabetes Care, 33, 378-384. http://www.ncbi.nlm.nih.gov/pubmed/19880581 http://dx.doi.org/10.2337/dc09-1027 [24] Räikkönen K., Matthews, K. and Kuller, L. (2007) De- pressive symptoms and stressful life events predict meta- bolic syndrome among middle-aged women. Diabetes Care, 30, 872-877. http://www.ncbi.nlm.nih.gov/pubmed/17392548 http://dx.doi.org/10.2337/dc06-1857 [25] Kim-Dorner, S., Simpson-Mackenzie, C., Poth, M. and Deuster, P. (2009) Psychological and physiological corre- lates of insulin resistance at fasting and in response to a meal in African Americans and Whites. Ethnicity & Dis- ease, 10, 104-110. http://www.ncbi.nlm.nih.gov/pubmed/19537218 [26] Novak, M., Björck, L., Giang, K., Heden-Stahl, C., Wi- helmsen, L. and Rosengren, A. (2013) Perceived stress and incidence of type 2 diabetes: A 35-year follow-up study of middle-aged Swedish men. Diabetic Medicine, 30, e8-e16. http://www.ncbi.nlm.nih.gov/pubmed/23075206 [27] Kruyt, N., van Westerloo D. and DeVries, H. (2012) Stress induced hyperglycemia in healthy bungee jumpers without diabetes due to decreased pancreatic B-cell func- tion and increased insulin resistance. Diabetes Technol- ogy & Therapeutics, 14, 311-314. http://www.ncbi.nlm.nih.gov/pubmed/22283617 http://dx.doi.org/10.1089/dia.2011.0171 [28] Shiloah, E., Witz, S., Abramovitch, Y., Cohen, O., Buchs, A., Ramot, Y., et al. (2003) Effect of acute psychotic stress in nondiabetic subjects on B-cell function and insu- lin sensitivity. Diabetes Care, 26, 1462-1467. http://care.diabetesjournals.org/content/26/5/1462.full.pdf http://dx.doi.org/10.2337/diacare.26.5.1462 [29] De Groot, M., Auslander, W., Williams, J., Sherraden, M. and Haire-Joshu, D. (2003) Depression and poverty among African American women at risk for type 2 diabetes. An- nals of Behavioral Medicine, 25, 172-181. http://www.ncbi.nlm.nih.gov/pubmed/12763712 [30] Krishnan, S., Cozier, Y., Rosenberg, L. and Palmer, J. (2010) Socioeconomic status and incidence of type 2 diabetes: Results from the Black women’s health study. American Journal of Epidemiology, 171, 564-570. http://www.ncbi.nlm.nih.gov/pubmed/20133518 http://dx.doi.org/10.1093/aje/kwp443 [31] Wagner, J., Osborn, C., Mendenhall, E., Budris, L., Belay, S. and Tenner, H. (2011) Beliefs about racism and health among African American women with diabetes: A quail- tative study. Journal of the National Medical Association, 103, 224-232. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3082367/ [32] Chang, S., Kim, H., Yoon, K., Ko, S., Kwon, H., Kim, S., et al. (2004) Body mass index is the most important de- termining factor for the degree of insulin resistance in non-obese type 2 diabetic patients in Korea. Metabolism, 53, 142-146. http://www.ncbi.nlm.nih.gov/pubmed/14767863 http://dx.doi.org/10.1016/S0026-0495(03)00314-7 [33] Everson-Rose, S., Meyer, P., Powell, L., Pandey, D., Tor- rens, J., Kravitz, J., et al. (2004) Depressive symptoms, insulin resistance, and risk of diabetes in women at mid- life. Diabetes Care, 27, 2856-2862. http://www.ncbi.nlm.nih.gov/pubmed/15562197 [34] Torrens, J., Skurnick, J., Davidow, A., Korenman, S., Santoro, N., Soto-Greene, M., et al. (2004) Ethnic differ- ences in insulin sensitivity and B-cell function in pre- menopausal or early perimenopausal women without dia- betes. Diabetes Care, 27, 354-361. http://care.diabetesjournals.org/content/27/2/354.full.pdf http://dx.doi.org/10.2337/diacare.27.2.354 [35] Fisher, L., Skaff, M., Mullan, J., Arean, P., Mohr, D., Masharani, U., et al. (2007) Clinical depression versus distress among patients with type 2 diabetes. Diabetes Care, 30, 542-548. http://www.ncbi.nlm.nih.gov/pubmed/17327318 http://dx.doi.org/10.2337/dc06-1614 Copyright © 2013 SciRes. OPEN A CCESS  F. G. Huffman et al. / Journal of Diabetes Mellitus 3 (2 013) 236-243 Copyright © 2013 SciRes. OPEN A CCESS 243 [36] Miller, S. (2011) Diabetes and psychological profile of younger rural African American women with type 2 dia- betes. Journal of Health Care for the Poor and Unde- served, 22, 1239-1252. http://www.ncbi.nlm.nih.gov/pubmed/22080706 [37] Huffman, F., Vaccaro, J., Ajabshir, S., Zarini, G., Exebio, J. and Dixon, Z. (2013) Perceived stress and self-rated health of Haitian and African Americans with and without type 2 diabetes. Journal of Research in Medical Science, 18, 198-204. http://www.ncbi.nlm.nih.gov/pubmed/23930115
|