 J. Biomedical Science and Engineering, 2013, 6, 1085-1089 JBiSE http://dx.doi.org/10.4236/jbise.2013.611136 Published Online November 2013 (http://www.scirp.org/journal/jbise/) OPEN ACCESS An AMPK paradox in pulmonary arterial hypertension Miranda Sun, Guofei Zhou* Department of Pediatrics, University of Illinois at Chicago, Chicago, USA Email: *guofei@uic.edu Received 27 September 2013; revised 29 October 2013; accepted 8 November 2013 Copyright © 2013 Miranda Sun, Guofei Zhou. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. ABSTRACT Adenosine monophosphate-activated protein kinase (AMPK) is a heterotrimeric serine-threonine kinase important as a metabolic sensor for intracellular ATP levels and plays a key role in regulating cell survival and proliferation, particularly when cells are exposed to hypoxia. AMPK is critical for lung function, and abnormal AMPK signaling participates in many lung diseases. Recent studies suggest that both inhibition and activation of AMPK are preventive for the de- velopment of pulmonary arterial hypertension (PAH). However, the molecular mechanisms by which inhibi- tion or activation of AMPK affects pulmonary hy- pertension (PH) appear to be distinct. Inhibition of AMPK by compound C blocks hypoxia-induced auto- phagy and induces apoptosis in pulmonary artery smooth muscle cells, leading to prevention of PAH; activation of AMPK by metformin attenuates the PH phenotype induced by hypoxia by regulating endothe- lial cell function. These seemingly opposing data on the function of AMPK in PH can be partly explained by off-target and compartment-specific effects of AMPK inhibitors and activators and the differenti- ated expression of AMPK in various cell types and subcellular locations. To elucidate the specific roles of AMPK in the pathogenesis of PAH, it is important to study the role of AMPK in a tissue specific manner combining genetic and biochemical approaches. Keywords: AMPK; Pulmonary Hypertension; Pulmonary Artery Smooth Muscle Cells; Endothelial Cells 1. INTRODUCTION Pulmonary arterial hypertension (PAH) is a disease cha- racterized by increased pulmonary arterial pressure that leads to right ventricular failure, and ultimately, death [1,2]. Active vasoconstriction as well as vascular remod- eling leads to manifestation of the disease. Pulmonary artery remodeling includes survival and proliferation of pulmonary artery smooth muscle cells (PASMC), which cause the development and progression of high pulmo- nary vascular tone observed in PAH patients [3]. Hy- poxia-induced pulmonary hypertension (PH) in several animal models is a well-established and commonly em- ployed method to investigate the pathogenesis of PAH. Hypoxia is known to induce right ventricular hypertro- phy (expressed as a ratio of right ventricular weight to left ventricular plus ventricular septum weight, RV/(LV + S), increased pulmonary arterial pressure, and pulmo- nary arterial wall remodeling [4]. Although major ad- vancements have been made in the last two decades in the understanding of the development and treatment of PAH, the exact mechanisms in the pathogenesis are still not clear and there is currently no cure for this disease. Adenosine monophosphate-activated protein kinase (AMPK) is a heterotrimeric serine-threonine kinase im- portant as a metabolic sensor for intracellular ATP levels [5]. AMPK is composed of three subunits, the catalytic α subunit and the regulatory β and γ subunits. Each of the subunits can be found in multiple isoforms (α 1, α 2, β 1, β 2, γ 1, γ 2, γ 3), giving a total of 12 combinations hav- ing different tissue distribution and subcellular localiza- tion patterns [5,6]. AMPK is allosterically activated by the binding of two AMP molecules to the γ subunit, al- lowing the phosphorylation of α Thr 172 in the catalytic domain via an upstream kinase, thus increasing kinase activity, and inhibiting AMPK dephosphorylation [5]. AMPK is sensitive to stress and low energy states when the AMP/ATP ratio increases, such as in hypoxia. AMPK is also considered a “master switch” in regulating cell survival and proliferation. For example, AMPK activity is increased in rapidly proliferating cells like cardiac fibroblasts and cancer cells [7,8]. In addition, cell cycle regulation, decision to enter autophagy, apoptosis, and other cell fate decisions are regulated by AMPK (Figure 1) [9]. *Corresponding author. 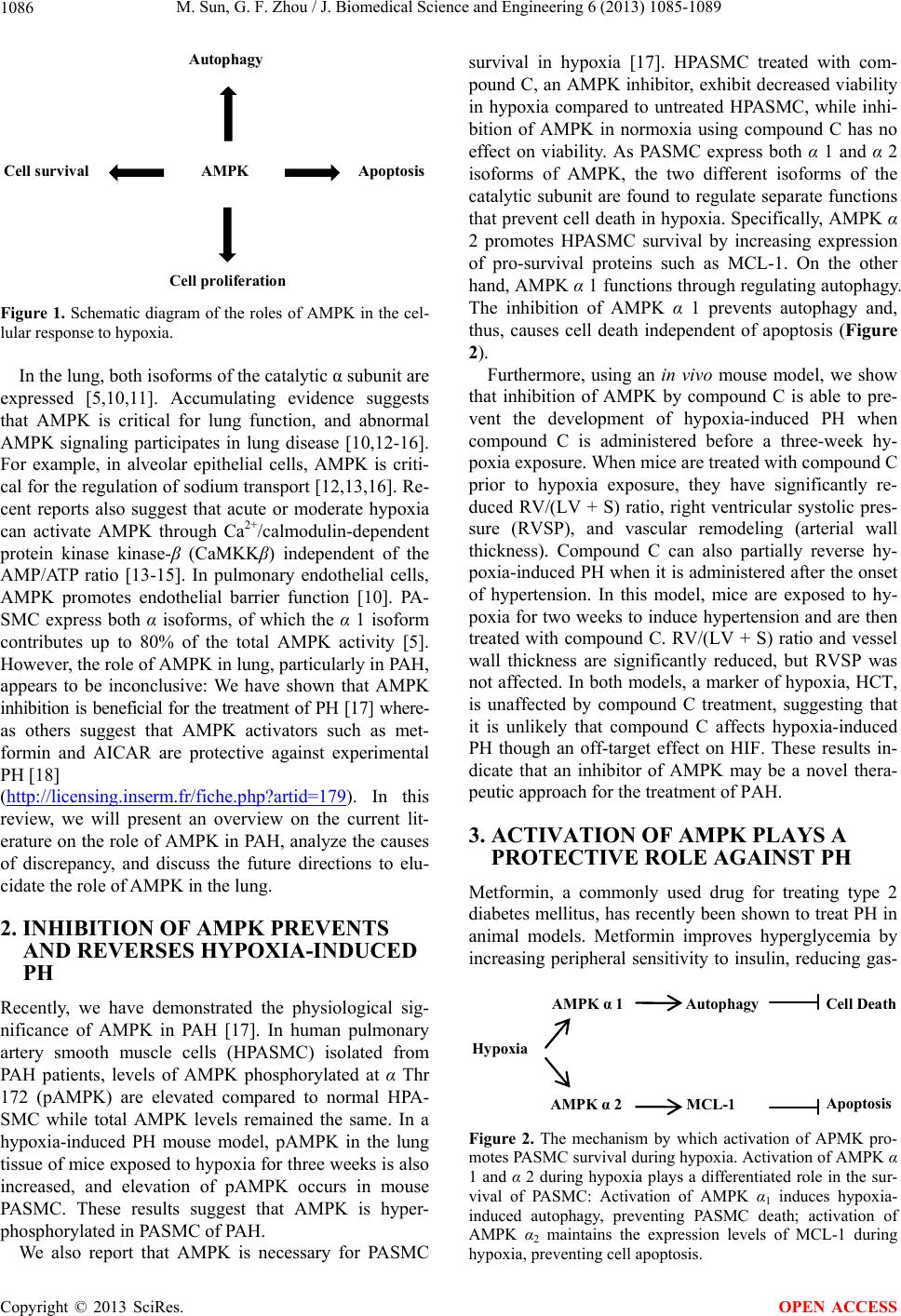 M. Sun, G. F. Zhou / J. Biomedical Science and Engineering 6 (2013) 1085-1089 Copyright © 2013 SciRes. OPEN ACCESS 1086 Autophagy AMPK Cell proliferation Apoptosis Cell survival Figure 1. Schematic diagram of the roles of AMPK in the cel- lular response to hypoxia. In the lung, both isoforms of the catalytic α subunit are expressed [5,10,11]. Accumulating evidence suggests that AMPK is critical for lung function, and abnormal AMPK signaling participates in lung disease [10,12-16]. For example, in alveolar epithelial cells, AMPK is criti- cal for the regulation of sodium transport [12,13,16]. Re- cent reports also suggest that acute or moderate hypoxia can activate AMPK through Ca2+/calmodulin-dependent protein kinase kinase-β (CaMKKβ) independent of the AMP/ATP ratio [13-15]. In pulmonary endothelial cells, AMPK promotes endothelial barrier function [10]. PA- SMC express both α isoforms, of which the α 1 isoform contributes up to 80% of the total AMPK activity [5]. However, the role of AMPK in lung, particularly in PAH, appears to be inconclusive: We have shown that AMPK inhibition is beneficial for the treatment of PH [17] where- as others suggest that AMPK activators such as met- formin and AICAR are protective against experimental PH [18] (http://licensing.inserm.fr/fiche.php?artid=179). In this review, we will present an overview on the current lit- erature on the role of AMPK in PAH, analyze the causes of discrepancy, and discuss the future directions to elu- cidate the role of AMPK in the lung. 2. INHIBITION OF AMPK PREVENTS AND REVERSES HYPOXIA-INDUCED PH Recently, we have demonstrated the physiological sig- nificance of AMPK in PAH [17]. In human pulmonary artery smooth muscle cells (HPASMC) isolated from PAH patients, levels of AMPK phosphorylated at α Thr 172 (pAMPK) are elevated compared to normal HPA- SMC while total AMPK levels remained the same. In a hypoxia-induced PH mouse model, pAMPK in the lung tissue of mice exposed to hypoxia for three weeks is also increased, and elevation of pAMPK occurs in mouse PASMC. These results suggest that AMPK is hyper- phosphorylated in PASMC of PAH. We also report that AMPK is necessary for PASMC survival in hypoxia [17]. HPASMC treated with com- pound C, an AMPK inhibitor, exhibit decreased viability in hypoxia compared to untreated HPASMC, while inhi- bition of AMPK in normoxia using compound C has no effect on viability. As PASMC express both α 1 and α 2 isoforms of AMPK, the two different isoforms of the catalytic subunit are found to regulate separate functions that prevent cell death in hypoxia. Specifically, AMPK α 2 promotes HPASMC survival by increasing expression of pro-survival proteins such as MCL-1. On the other hand, AMPK α 1 functions through regulating autophagy. The inhibition of AMPK α 1 prevents autophagy and, thus, causes cell death independent of apoptosis (Figure 2). Furthermore, using an in vivo mouse model, we show that inhibition of AMPK by compound C is able to pre- vent the development of hypoxia-induced PH when compound C is administered before a three-week hy- poxia exposure. When mice are treated with compound C prior to hypoxia exposure, they have significantly re- duced RV/(LV + S) ratio, right ventricular systolic pres- sure (RVSP), and vascular remodeling (arterial wall thickness). Compound C can also partially reverse hy- poxia-induced PH when it is administered after the onset of hypertension. In this model, mice are exposed to hy- poxia for two weeks to induce hypertension and are then treated with compound C. RV/(LV + S) ratio and vessel wall thickness are significantly reduced, but RVSP was not affected. In both models, a marker of hypoxia, HCT, is unaffected by compound C treatment, suggesting that it is unlikely that compound C affects hypoxia-induced PH though an off-target effect on HIF. These results in- dicate that an inhibitor of AMPK may be a novel thera- peutic approach for the treatment of PAH. 3. ACTIVATION OF AMPK PLAYS A PROTECTIVE ROLE AGAINST PH Metformin, a commonly used drug for treating type 2 diabetes mellitus, has recently been shown to treat PH in animal models. Metformin improves hyperglycemia by increasing peripheral sensitivity to insulin, reducing gas- AMPK α 1 Autophagy Cell Death Apoptosis MCL-1 Hypoxia AMPK α 2 Figure 2. The mechanism by which activation of APMK pro- motes PASMC survival during hypoxia. Activation of AMPK α 1 and α 2 during hypoxia plays a differentiated role in the sur- vival of PASMC: Activation of AMPK α1 induces hypoxia- induced autophagy, preventing PASMC death; activation of AMPK α2 maintains the expression levels of MCL-1 during hypoxia, preventing cell apoptosis. 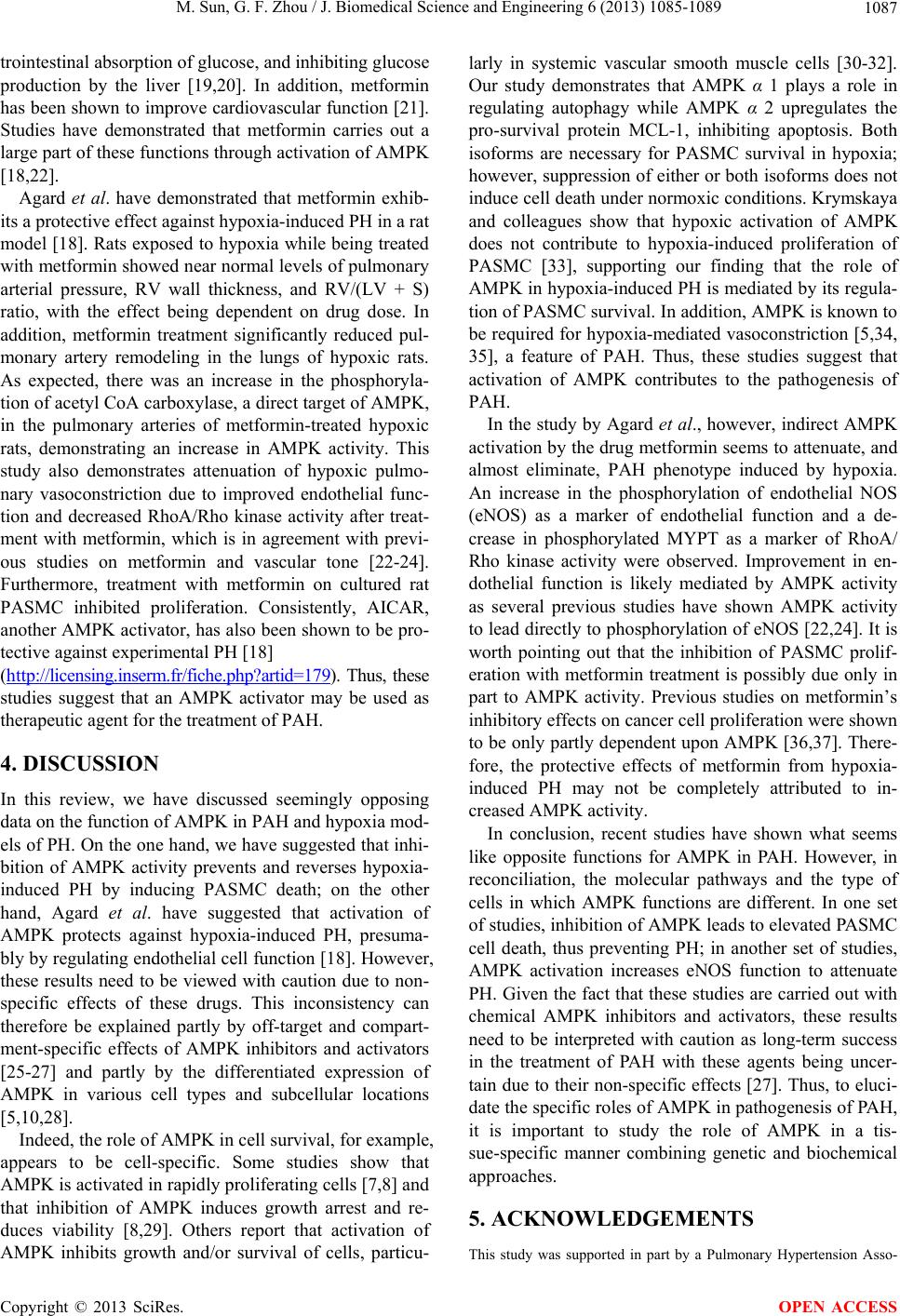 M. Sun, G. F. Zhou / J. Biomedical Science and Engineering 6 (2013) 1085-1089 Copyright © 2013 SciRes. OPEN ACCESS 1087 trointestinal absorption of glucose, and inhibiting glucose production by the liver [19,20]. In addition, metformin has been shown to improve cardiovascular function [21]. Studies have demonstrated that metformin carries out a large part of these functions through activation of AMPK [18,22]. Agard et al. have demonstrated that metformin exhib- its a protective effect against hypoxia-induced PH in a rat model [18]. Rats exposed to hypoxia while being treated with metformin showed near normal levels of pulmonary arterial pressure, RV wall thickness, and RV/(LV + S) ratio, with the effect being dependent on drug dose. In addition, metformin treatment significantly reduced pul- monary artery remodeling in the lungs of hypoxic rats. As expected, there was an increase in the phosphoryla- tion of acetyl CoA carboxylase, a direct target of AMPK, in the pulmonary arteries of metformin-treated hypoxic rats, demonstrating an increase in AMPK activity. This study also demonstrates attenuation of hypoxic pulmo- nary vasoconstriction due to improved endothelial func- tion and decreased RhoA/Rho kinase activity after treat- ment with metformin, which is in agreement with previ- ous studies on metformin and vascular tone [22-24]. Furthermore, treatment with metformin on cultured rat PASMC inhibited proliferation. Consistently, AICAR, another AMPK activator, has also been shown to be pro- tective against experimental PH [18] (htt p://licensing.inserm.fr/fiche.php?artid=179). Thus, these studies suggest that an AMPK activator may be used as therapeutic agent for the treatment of PAH. 4. DISCUSSION In this review, we have discussed seemingly opposing data on the function of AMPK in PAH and hypoxia mod- els of PH. On the one hand, we have suggested that inhi- bition of AMPK activity prevents and reverses hypoxia- induced PH by inducing PASMC death; on the other hand, Agard et al. have suggested that activation of AMPK protects against hypoxia-induced PH, presuma- bly by regulating endothelial cell function [18]. However, these results need to be viewed with caution due to non- specific effects of these drugs. This inconsistency can therefore be explained partly by off-target and compart- ment-specific effects of AMPK inhibitors and activators [25-27] and partly by the differentiated expression of AMPK in various cell types and subcellular locations [5,10,28]. Indeed, the role of AMPK in cell survival, for example, appears to be cell-specific. Some studies show that AMPK is activated in rapidly proliferating cells [7,8] and that inhibition of AMPK induces growth arrest and re- duces viability [8,29]. Others report that activation of AMPK inhibits growth and/or survival of cells, particu- larly in systemic vascular smooth muscle cells [30-32]. Our study demonstrates that AMPK α 1 plays a role in regulating autophagy while AMPK α 2 upregulates the pro-survival protein MCL-1, inhibiting apoptosis. Both isoforms are necessary for PASMC survival in hypoxia; however, suppression of either or both isoforms does not induce cell death under normoxic conditions. Krymskaya and colleagues show that hypoxic activation of AMPK does not contribute to hypoxia-induced proliferation of PASMC [33], supporting our finding that the role of AMPK in hypoxia-induced PH is mediated by its regula- tion of PASMC survival. In addition, AMPK is known to be required for hypoxia-mediated vasoconstriction [5,34, 35], a feature of PAH. Thus, these studies suggest that activation of AMPK contributes to the pathogenesis of PAH. In the study by Agard et al., however, indirect AMPK activation by the drug metformin seems to attenuate, and almost eliminate, PAH phenotype induced by hypoxia. An increase in the phosphorylation of endothelial NOS (eNOS) as a marker of endothelial function and a de- crease in phosphorylated MYPT as a marker of RhoA/ Rho kinase activity were observed. Improvement in en- dothelial function is likely mediated by AMPK activity as several previous studies have shown AMPK activity to lead directly to phosphorylation of eNOS [22,24]. It is worth pointing out that the inhibition of PASMC prolif- eration with metformin treatment is possibly due only in part to AMPK activity. Previous studies on metformin’s inhibitory effects on cancer cell proliferation were shown to be only partly dependent upon AMPK [36,37]. There- fore, the protective effects of metformin from hypoxia- induced PH may not be completely attributed to in- creased AMPK activity. In conclusion, recent studies have shown what seems like opposite functions for AMPK in PAH. However, in reconciliation, the molecular pathways and the type of cells in which AMPK functions are different. In one set of studies, inhibition of AMPK leads to elevated PASMC cell death, thus preventing PH; in another set of studies, AMPK activation increases eNOS function to attenuate PH. Given the fact that these studies are carried out with chemical AMPK inhibitors and activators, these results need to be interpreted with caution as long-term success in the treatment of PAH with these agents being uncer- tain due to their non-specific effects [27]. Thus, to eluci- date the specific roles of AMPK in pathogenesis of PAH, it is important to study the role of AMPK in a tis- sue-specific manner combining genetic and biochemical approaches. 5. ACKNOWLEDGEMENTS This study was supported in part by a Pulmonary Hypertension Asso-  M. Sun, G. F. Zhou / J. Biomedical Science and Engineering 6 (2013) 1085-1089 Copyright © 2013 SciRes. OPEN ACCESS 1088 ciation/Pfizer Proof-of-Concept award (G. Zhou) in which American Thoracic Society provides administrative support. REFERENCES [1] Humbert, M., Sitbon, O. and Simonneau, G. (2004) Treat- ment of pulmonary arterial hypertension. New England Journal of Medicine, 351, 1425-1436. http://dx.doi.org/10.1056/NEJMra040291 [2] McLaughlin, V.V., Archer, S.L., Badesch, D.B., Barst, R.J., Farber, H.W., Lindner, J.R., et al. (2009) ACCF/ AHA 2009 expert consensus document on pulmonary hypertension: A report of the American College of Cardi- ology Foundation Task Force on Expert Consensus Documents and the American Heart Association: De- veloped in collaboration with the American College of Chest Physicians, American Thoracic Society, Inc., and the Pulmonary Hypertension Association. Circulation, 119, 2250-2294. http://dx.doi.org/10.1161/CIRCULATIONAHA.109.1922 30 [3] Durmowicz, A.G. and Stenmark, K.R. (1999) Mecha- nisms of structural remodeling in chronic pulmonary hy- pertension. Pediatrics in Review/American Academy of Pediatrics, b, e91-e102. [4] Stenmark, K.R., Fagan, K.A. and Frid, M.G. (2006) Hy- poxia-induced pulmonary vascular remodeling: Cellular and molecular mechanisms. Circulation Research, 99, 675- 691. http://dx.doi.org/10.1161/01.RES.0000243584.45145.3f [5] Evans, A.M., Hardie, D.G., Peers, C., Wyatt, C.N., Viollet, B., Kumar, P., et al. (2009) Ion channel regula- tion by AMPK: The route of hypoxia-response coupling in the carotid body and pulmonary artery. Annals of the New York Academy of Sciences, 1177, 89-100. http://dx.doi.org/10.1111/j.1749-6632.2009.05041.x [6] Horman, S., Morel, N., Vertommen, D., Hussain, N., Neumann, D., Beauloye, C., et al. (2008) AMP-activated protein kinase phosphorylates and desensitizes smooth muscle myosin light chain kinase. The Journal of Bio- Logical Chemistry, 283, 18505-18512. http://dx.doi.org/10.1074/jbc.M802053200 [7] Hattori, Y., Akimoto, K., Nishikimi, T., Matsuoka, H. and Kasai, K. (2006) Activation of AMP-activated pro- tein kinase enhances angiotensin ii-induced proliferation in cardiac fibroblasts. Hypertension, 47, 265-270. http://dx.doi.org/10.1161/01.HYP.0000198425.21604.aa [8] Park, H.U., Suy, S., Danner, M., Dailey, V., Zhang, Y., Li, H., et al. (2009) AMP-activated protein kinase pro- motes human prostate cancer cell growth and survival. Molecular cancer therapeutics, 8, 733-741. http://dx.doi.org/10.1158/1535-7163.MCT-08-0631 [9] Mishra, R., Cool, B.L., Laderoute, K.R., Foretz, N., Viol- let, B. and Simonson, M.S. (2008) AMP-activated protein kinase inhibits transforming growth factor-beta-induced Smad3-dependent transcription and myofibroblast trans- differentiation. The Journal of Biological Chemistry, 283, 10461-10469. http://dx.doi.org/10.1074/jbc.M800902200 [10] Creighton, J., Jian, M., Sayner, S., Alexeyev, M. and Insel, P.A. (2011) Adenosine monophosphate-activated kinase alpha1 promotes endothelial barrier repair. FASEB Journal: Official Publication of the Federation of Ameri- can Societies for Experimental Biology, 25, 3356-3365. [11] Evans, A.M., Mustard, K.J.W., Wyatt, C.N., Dipp, M., Kinnear, N.P. and Hardie, D.G. (2006) Does AMP-acti- vated protein kinase couple inhibition of mitochondrial oxidative phosphorylation by hypoxia to pulmonary ar- tery constriction? Advances in experimental medicine and biology, 580, 147-154. http://dx.doi.org/10.1007/0-387-31311-7_22 [12] Dada, L., Gonzalez, A.R., Urich, D., Soberanes, S., Manghi, T.S., Chiarella, S.E., et al. (2012) Alcohol wor- sens acute lung injury by inhibiting alveolar sodium transport through the adenosine A1 receptor. PLoS ONE [Electronic Resource], 7, Article ID: e30448. http://dx.doi.org/10.1371/journal.pone.0030448 [13] Gusarova, G.A., Dada, L.A., Kelly, A.M., Brodie, C., Witters, L.A., Chandel N.S. and Sznajder, J.I. (2009) Al- pha1-AMP-activated protein kinase regulates hypoxia- induced Na,K-ATPase endocytosis via direct phospho- rylation of protein kinase C zeta. Molecular and cellular biology, 29, 3455-3464. http://dx.doi.org/10.1128/MCB.00054-09 [14] Gusarova, G.A., Trejo, H.E., Dada, L.A., Briva, A., Welch, L.C., Hamanaka, R.B., et al. (2011) Hypoxia leads to Na,K-ATPase downregulation via Ca(2+) release-acti- vated Ca(2+) channels and AMPK activation. Molecular and cellular biology, 31, 3546-3556. http://dx.doi.org/10.1128/MCB.05114-11 [15] Mungai, P.T., Waypa, G.B., Jairaman, A., Prakriya, M., Dokic, D., Ball, M.K., et al. (2011) Hypoxia triggers AMPK activation through reactive oxygen species-me- diated activation of calcium release-activated calcium channels. Molecular and cellular biology, 31, 3531-3545. http://dx.doi.org/10.1128/MCB.05124-11 [16] Vadász, I., Dada, L.A., Briva, A., Trejo, H.E., Welch, L.C., Chen, J., et al. (2008) AMP-activated protein kinase regulates CO2-induced alveolar epithelial dysfunction in rats and human cells by promoting Na,K-ATPase endo- cytosis. Journal of Clinical Investigation, 118, 752-762. [17] Ibe, J.C., Zhou, Q., Chen, T., Tang, H., Yuan, J.X., Raj, J.U., et al. (2013) AMPK is required for pulmonary artery smooth muscle cell survival and the development of hy- poxic pulmonary hypertension. American Journal of Res- piratory Cell and Molecular Biology, in Press. http://dx.doi.org/10.1165/rcmb.2012-0446OC [18] Agard, C., Rolli-Derkinderen, M., Dumas-de-La-Roque, E., Rio, M., Sagan, C., Savineau, J.P., et al. (2009) Pro- tective role of the antidiabetic drug metformin against chronic experimental pulmonary hypertension. British journal of Pharmacology, 158, 1285-1294. http://dx.doi.org/10.1111/j.1476-5381.2009.00445.x [19] Borst, S.E. and Snellen, H.G. (2001) Metformin, but not exercise training, increases insulin responsiveness in skeletal muscle of Sprague-Dawley rats. Life Sciences, 69, 1497-1507. http://dx.doi.org/10.1016/S0024-3205(01)01225-5  M. Sun, G. F. Zhou / J. Biomedical Science and Engineering 6 (2013) 1085-1089 Copyright © 2013 SciRes. OPEN ACCESS 1089 [20] Hundal, R.S., Krssak, M., Dufour, S., Laurent, D., Lebon, V., Chandramouli, V., et al. (2000) Mechanism by which metformin reduces glucose production in type 2 diabetes. Diabetes, 49, 2063-2069. http://dx.doi.org/10.2337/diabetes.49.12.2063 [21] McAlister, F.A., Eurich, D.T., Majumdar, S.R. and John- son, J.A. (2008) The risk of heart failure in patients with type 2 diabetes treated with oral agent monotherapy. European Journal of Heart Failure, 10, 703-708. http://dx.doi.org/10.1016/j.ejheart.2008.05.013 [22] Davis, B.J., Xie, Z., Viollet, B. and Zou, M.H. (2006) Activation of the AMP-activated kinase by antidiabetes drug metformin stimulates nitric oxide synthesis in vivo by promoting the association of heat shock protein 90 and endothelial nitric oxide synthase. Diabetes, 55, 496-505. http://dx.doi.org/10.2337/diabetes.55.02.06.db05-1064 [23] Fagan, K.A., Oka, M., Bauer, N.R., Gebb, S.A., Ivy, D.D., Morris, K.G., et al. (2004) Attenuation of acute hypoxic pulmonary vasoconstriction and hypoxic pulmonary hy- pertension in mice by inhibition of Rho-kinase. American journal of physiology Lung cellular and molecular physi- ology, 287, L656-L664. http://dx.doi.org/10.1152/ajplung.00090.2003 [24] Morrow, V.A., Foufelle, F., Connell, J.M.C., Petrie, J.R., Gould, G.W. and Salt, I.P. (2003) Direct activation of AMP-activated protein kinase stimulates nitric-oxide synthesis in human aortic endothelial cells. The Journal of Biological Chemistry, 278, 31629-31639. http://dx.doi.org/10.1074/jbc.M212831200 [25] Creighton, J. (2011) Targeting therapeutic effects: Sub- cellular location matters. Focus on “Pharmacological AMP- kinase activators have compartment-specific effects on cell physiology”. American Journal of Physiology Cell Physiology, 301, C1293-C1295. http://dx.doi.org/10.1152/ajpcell.00358.2011 [26] Kodiha, M., Ho-Wo-Cheong, D. and Stochaj, U. (2011) Pharmacological AMP-kinase activators have compart- ment-specific effects on cell physiology. American Jour- Nal of Physiology Cell Physiology, 301, C1307-C1315. http://dx.doi.org/10.1152/ajpcell.00309.2011 [27] Viollet, B., Horman, S., Leclerc, J., Lantier, L., Foretz, M., Billaud, M., et al. (2010) AMPK inhibition in health and disease. Critical Reviews in Biochemistry and Mo- Lecular Biology, 45, 276-295. http://dx.doi.org/10.3109/10409238.2010.488215 [28] Viollet, B., Athea, Y., Mounier, R., Guigas, B., Zarrin- pashneh, E., Horman, S., et al. (2009) AMPK: Lessons from transgenic and knockout animals. Frontiers in Bio- Science: A Journal and Virtual Library, 14, 19-44. [29] Chhipa, R.R., Wu, Y., Mohler, J.L. and Ip, C. (2010) Sur- vival advantage of AMPK activation to androgen-inde- pendent prostate cancer cells during energy stress. Cellu- lar Signalling, 22, 1554-1561. http://dx.doi.org/10.1016/j.cellsig.2010.05.024 [30] Igata, M., Motoshima, H., Tsuruzoe, K., Kojima, K., Matsumura, T., Kondo, T., et al. (2005) Adenosine mo- nophosphate-activated protein kinase suppresses vascular smooth muscle cell proliferation through the inhibition of cell cycle progression. Circulation Research, 97, 837-844. http://dx.doi.org/10.1161/01.RES.0000185823.73556.06 [31] Nagata, D., Takeda, R., Sata, M., Satonaka, H., Suzuki, E., Nagano, T. and Hirata, Y. (2004) AMP-activated pro- tein kinase inhibits angiotensin II-stimulated vascular smooth muscle cell proliferation. Circulation, 110, 444- 451. http://dx.doi.org/10.1161/01.CIR.0000136025.96811.76 [32] Vucicevic, L., Misirkic, M., Janjetovic, K., Harhaji-Traj- kovic, L., Prica, M., Stevanovic, D., et al. (2009) AMP- activated protein kinase-dependent and independent me- chanisms underlying in vitro antiglioma action of com- pound C. Biochemical Pharmacology, 77, 1684-1693. http://dx.doi.org/10.1016/j.bcp.2009.03.005 [33] Krymskaya, V.P., Snow, J., Cesarone, G., Khavin, I., Goncharov, D.A., Lim, P.N., et al. (2011) mTOR is re- quired for pulmonary arterial vascular smooth muscle cell proliferation under chronic hypoxia. FASEB Journal: Of- ficial Publication of the Federation of American Societies for Experimental Biology, 25, 1922-1933. [34] Evans, A.M. (2006) AMP-activated protein kinase un- derpins hypoxic pulmonary vasoconstriction and carotid body excitation by hypoxia in mammals. Experimental physiology, 91, 821-827. http://dx.doi.org/10.1113/expphysiol.2006.033514 [35] Robertson, T.P., Mustard, K.J.W., Lewis, T.H., Clark, J.H., Wyatt, C.N., Blanco, E.A., et al. (2008) AMP-acti- vated protein kinase and hypoxic pulmonary vasocon- striction. European Journal of Pharmacology, 595, 39-43. http://dx.doi.org/10.1016/j.ejphar.2008.07.035 [36] Ben Sahra, I., Laurent, K., Loubat, A., Giorgetti-Peraldi, S., Colosetti, P., Auberger, P., et al. (2008) The antidia- betic drug metformin exerts an antitumoral effect in vitro and in vivo through a decrease of cyclin D1 level. Onco- gene, 27, 3576-3586. http://dx.doi.org/10.1038/sj.onc.1211024 [37] Zhuang, Y. and Miskimins, W.K. (2008) Cell cycle arrest in metformin treated breast cancer cells involves activa- tion of AMPK, downregulation of cyclin D1, and requires p27Kip1 or p21Cip1. Journal of Molecular Signaling, 3, 18. http://dx.doi.org/10.1186/1750-2187-3-18
|