B. Iranloye et al. / Journal of Diabetes Mellitus 3 (2013) 221-226 225
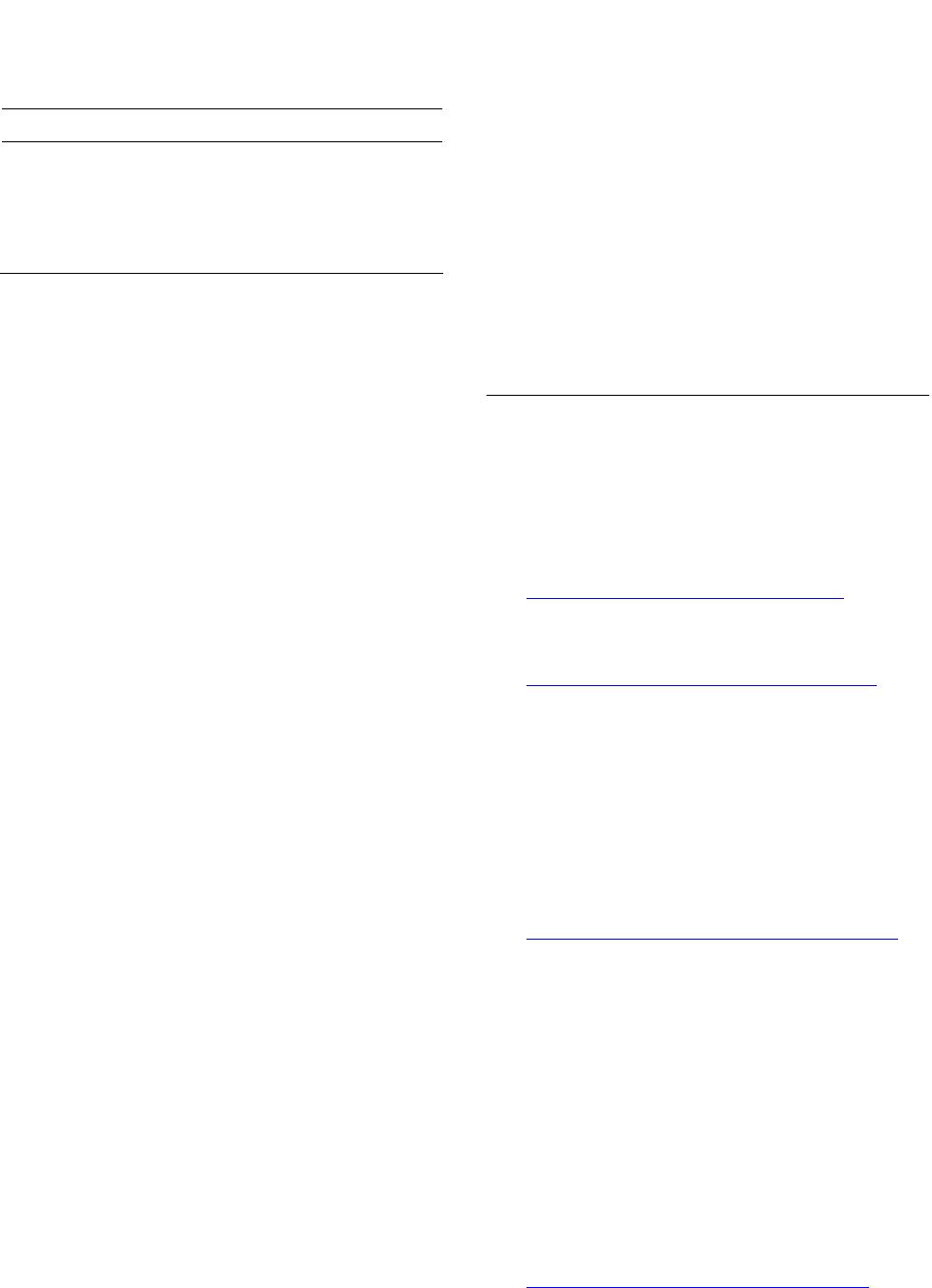
Table 2. Effect of virgin coconut oil (VCO) on serum insulin
level.
Insulin level (μiu/ml)
Control (C) 3.05 ± 0.25
Diabetes untreated (DUT) 1.19 ± 0.04*
Diabetes + 7.5 ml/kg VCO (DT7.5) 1.90 ± 0.40*
Diabetes + 10 ml/kg VCO (DT10) 2.50 ± 0.03#
Values are expressed as mean ± S.E.M. *p < 0.05 is significant compared
with Control. #p < 0.05 is significant compared with Diabetes untreated
group.
even after 3 hours indicating impairment in glucose tol-
erance which is an indication of diabetes. In DT7.5 and
DT10 rats there was a significant improvement in glucose
tolerance compared with the DUT rats, supporting the
view that ingestion of VCO improves glucose tolerance
in diabetic rats [21]. In addition, the 10 ml/kg dosage of
VCO proved to have a greater effect as the blood glucose
level in DT10 rats after 3 hours of glucose challenge was
closer to the control value than in DT7.5 rats.
It has been reported that the lauric oil in VCO pos-
sesses insulino-tropic properties [18]. Serum insulin was
increased in DT10 rats with a non significant increase in
DT7.5 rats compared with DUT rats. Since the dosage of
7.5 ml/kg body weight of VCO could not elevate serum
insulin, it implies that the 10 ml/kg body weight dose is
more effective in the control of glucose homeostasis than
the 7.5 ml/kg body weight. This is evidenced by the re-
duction in blood glucose level and the improvement in
glucose tolerance compared to DUT rats as discussed
earlier.
Antioxidant enzymes are critical part of cellular pro-
tection against reactive oxygen species and ultimately
oxidative stress. Oxidative stress is determined by the
balance between the generation of ROS such as super-
oxide anion (2
O) and the antioxidant defense systems
such as superoxide dismutase (SOD). Antioxidants en-
zymes involved in the elimination of ROS include SOD,
CAT and GSH, respectively. The present study showed a
decrease in the activity of all measured antioxidants en-
zymes in DUT rats. This indicates a decrease in the anti-
oxidant defense system. However treatment with VCO in
DT7.5 and DT10 rats increased the activities of the anti-
oxidant enzymes. Since oxidative stress contributes sig-
nificantly to the pathophysiology of diabetes [22], sub-
stances that suppress oxidative stress might be therapeu-
tically beneficial. Studies have shown that exogenously
administered antioxidants have protective effects on dia-
betes, thus providing insight into the relationship be-
tween free radicals and diabetes [20,22-24]. The reduc-
tion in fasting blood glucose of rats treated with VCO
after 4 weeks and a decrease in the OGTT of the rats
compared with the diabetic untreated rats can be associ-
ated to the antioxidant effect of VCO.
5. CONCLUSION
VCO alleviates hyperglycemia and improves glucose
tolerance probably by its antioxidant effect which con-
sequently leads to improvement of insulin secretion as
examined in this study. The study also shows that a dos-
age of 10 ml/kg body weight of VCO is quite beneficial
and more effective than that of 7.5 ml/kg body weight.
This was evident because the 7.5 ml/kg body weight did
not increase insulin secretion and possibly because of the
higher OGTT values.
REFERENCES
[1] American Diabetes Association (2010) Diagnosis and
classification of diabetes mellitus. Diabetic Care, 33.
[2] World Health Organization (2011) Diabetes fact sheet.
Sheet number 312 August.
[3] Lenzen, S. (2008) The mechanisms of alloxan- and strep-
tozotocin-induced Diabetes. Diabetologia, 51, 216-226.
http://dx.doi.org/10.1007/s00125-007-0886-7
[4] Nevin, K.G. and Rajamohan, T. (2006) Virgin coconut oil
supplemented diet increases the antioxidant status in rats.
Food Chemistry, 99, 260-266.
http://dx.doi.org/10.1016/j.foodchem.2005.06.056
[5] Dosumu, O.O., Duru, F.I.O., Osinubi, A.A., Oremosu,
A.A. and Noronha, C.C. (2010) Influence of virgin coco-
nut oil (VCNO) on oxidative stress, serum testosterone
and gonadotropic hormones (FSH, LH) in chronic ethanol
ingestion. Agriculture and Biology Journal of North Ame-
rica, 1, 1126-1132.
[6] Van Immerseel, F., De Buck, J. and Boyen, F. (2004)
Medium-chain fatty acids decrease colonization and in-
vasion through hilA suppression shortly after infection of
chickens with Salmonella enterica serovar enteritidis. Ap-
plied and Environmental Microbiology, 70, 3582-3587.
http://dx.doi.org/10.1128/AEM.70.6.3582-3587.2004
[7] Takeuchi, H., Sekine, S., Kojima, K. and Aoyama, T.
(2008) The application of medium-chain fatty acids: Edi-
ble oil with a suppressing effect on body fat accumulation.
Asia Pacific Journal of Clinical Nutrition, 17, 320-324.
[8] Anosike, C.A. and Obidoa, O. (2010) Anti-inflammatory
and anti-ulcerogenic effect of ethanol extract of coconut
(Cocos nucifera) on experimental rats. African Journal of
Food, Agriculture, Nutrition and Development, 10, 10-16.
[9] Cretney, J. and Tafunai, A. (2004) Tradition, trade, and
technology: Virgin coconut oil in samoa. In Chains of
Fortune: Linking Women Producers and Workers with
Global Markets, 45-74.
[10] Uchiyama, M. and Mihara, M. (1978) Determination of
malonaldehyde precursor in tissues by thiobarbituris acid
test. Analytical Biochemistry, 86, 271-278.
http://dx.doi.org/10.1016/0003-2697(78)90342-1
[11] Sun, M. and Zigmam S. (1978) An improved spectro-
Copyright © 2013 SciRes. OPEN ACCES S