F. ALOUNI ET AL.
Open Access IJOHNS
231
Figure 3. Histopathologic examination of the specimen taken
from left sphenoid sinus.
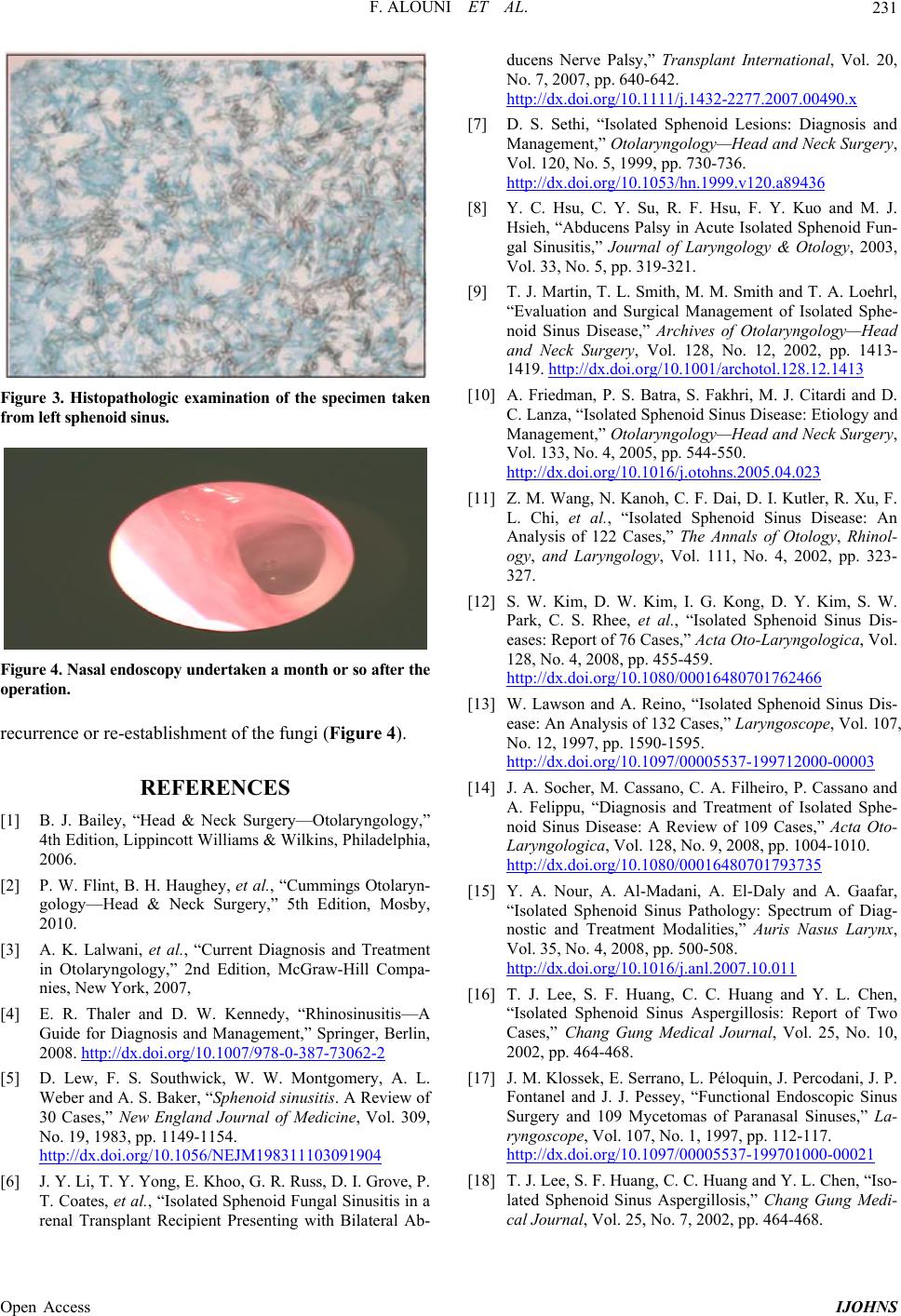
Figure 4. Nasal endoscopy underta ken a mo nth or so after the
operatio n.
recurrence or re-establishment of the fungi (Figure 4).
REFERENCES
[1] B. J. Bailey, “Head & Neck Surgery—Otolaryngology,”
4th Edition, Lippincott Williams & Wilkins, Philadelphia,
2006.
[2] P. W. Flint, B. H. Haughey, et al., “Cummings Otolaryn-
gology—Head & Neck Surgery,” 5th Edition, Mosby,
2010.
[3] A. K. Lalwani, et al., “Current Diagnosis and Treatment
in Otolaryngology,” 2nd Edition, McGraw-Hill Compa-
nies, New York, 2007,
[4] E. R. Thaler and D. W. Kennedy, “Rhinosinusitis—A
Guide for Diagnosis and Management,” Springer, Berlin,
2008. http://dx.doi.org/10.1007/978-0-387-73062-2
[5] D. Lew, F. S. Southwick, W. W. Montgomery, A. L.
Weber and A. S. Baker, “Sphenoid sinusitis. A Review of
30 Cases,” New England Journal of Medicine, Vol. 309,
No. 19, 1983, pp. 1149-1154.
http://dx.doi.org/10.1056/NEJM198311103091904
[6] J. Y. Li, T. Y. Yong, E. Khoo, G. R. Russ, D. I. Grove, P.
T. Coates, et al., “Isolated Sphenoid Fungal Sinusitis in a
renal Transplant Recipient Presenting with Bilateral Ab-
ducens Nerve Palsy,” Transplant International, Vol. 20,
No. 7, 2007, pp. 640-642.
http://dx.doi.org/10.1111/j.1432-2277.2007.00490.x
[7] D. S. Sethi, “Isolated Sphenoid Lesions: Diagnosis and
Management,” Otolaryngology—Head and Neck Surgery,
Vol. 120, No. 5, 1999, pp. 730-736.
http://dx.doi.org/10.1053/hn.1999.v120.a89436
[8] Y. C. Hsu, C. Y. Su, R. F. Hsu, F. Y. Kuo and M. J.
Hsieh, “Abducens Palsy in Acute Isolated Sphenoid Fun-
gal Sinusitis,” Journal of Laryngology & Otology, 2003,
Vol. 33, No. 5, pp. 319-321.
[9] T. J. Martin, T. L. Smith, M. M. Smith and T. A. Loehrl,
“Evaluation and Surgical Management of Isolated Sphe-
noid Sinus Disease,” Archives of Otolaryngology—Head
and Neck Surgery, Vol. 128, No. 12, 2002, pp. 1413-
1419. http://dx.doi.org/10.1001/archotol.128.12.1413
[10] A. Friedman, P. S. Batra, S. Fakhri, M. J. Citardi and D.
C. Lanza, “Isolated Sphenoid Sinus Disease: Etiology and
Management,” Otolaryngology—Head and Neck Surgery,
Vol. 133, No. 4, 2005, pp. 544-550.
http://dx.doi.org/10.1016/j.otohns.2005.04.023
[11] Z. M. Wang, N. Kanoh, C. F. Dai, D. I. Kutler, R. Xu, F.
L. Chi, et al., “Isolated Sphenoid Sinus Disease: An
Analysis of 122 Cases,” The Annals of Otology, Rhinol-
ogy, and Laryngology, Vol. 111, No. 4, 2002, pp. 323-
327.
[12] S. W. Kim, D. W. Kim, I. G. Kong, D. Y. Kim, S. W.
Park, C. S. Rhee, et al., “Isolated Sphenoid Sinus Dis-
eases: Report of 76 Cases,” Acta Oto-Laryngologica, Vol.
128, No. 4, 2008, pp. 455-459.
http://dx.doi.org/10.1080/00016480701762466
[13] W. Lawson and A. Reino, “Isolated Sphenoid Sinus Dis-
ease: An Analysis of 132 Cases,” Laryngoscope, Vol. 107,
No. 12, 1997, pp. 1590-1595.
http://dx.doi.org/10.1097/00005537-199712000-00003
[14] J. A. Socher, M. Cassano, C. A. Filheiro, P. Cassano and
A. Felippu, “Diagnosis and Treatment of Isolated Sphe-
noid Sinus Disease: A Review of 109 Cases,” Acta Oto-
Laryngologica, Vol. 128, No. 9, 2008, pp. 1004-1010.
http://dx.doi.org/10.1080/00016480701793735
[15] Y. A. Nour, A. Al-Madani, A. El-Daly and A. Gaafar,
“Isolated Sphenoid Sinus Pathology: Spectrum of Diag-
nostic and Treatment Modalities,” Auris Nasus Larynx,
Vol. 35, No. 4, 2008, pp. 500-508.
http://dx.doi.org/10.1016/j.anl.2007.10.011
[16] T. J. Lee, S. F. Huang, C. C. Huang and Y. L. Chen,
“Isolated Sphenoid Sinus Aspergillosis: Report of Two
Cases,” Chang Gung Medical Journal, Vol. 25, No. 10,
2002, pp. 464-468.
[17] J. M. Klossek, E. Serrano, L. Péloquin, J. Percodani, J. P.
Fontanel and J. J. Pessey, “Functional Endoscopic Sinus
Surgery and 109 Mycetomas of Paranasal Sinuses,” La-
ryngoscope, Vol. 107, No. 1, 1997, pp. 112-117.
http://dx.doi.org/10.1097/00005537-199701000-00021
[18] T. J. Lee, S. F. Huang, C. C. Huang and Y. L. Chen, “Iso-
lated Sphenoid Sinus Aspergillosis,” Chang Gung Medi-
cal Journal, Vol. 25, No. 7, 2002, pp. 464-468.