Outcome of Strabismus in Children with Cataracts 125
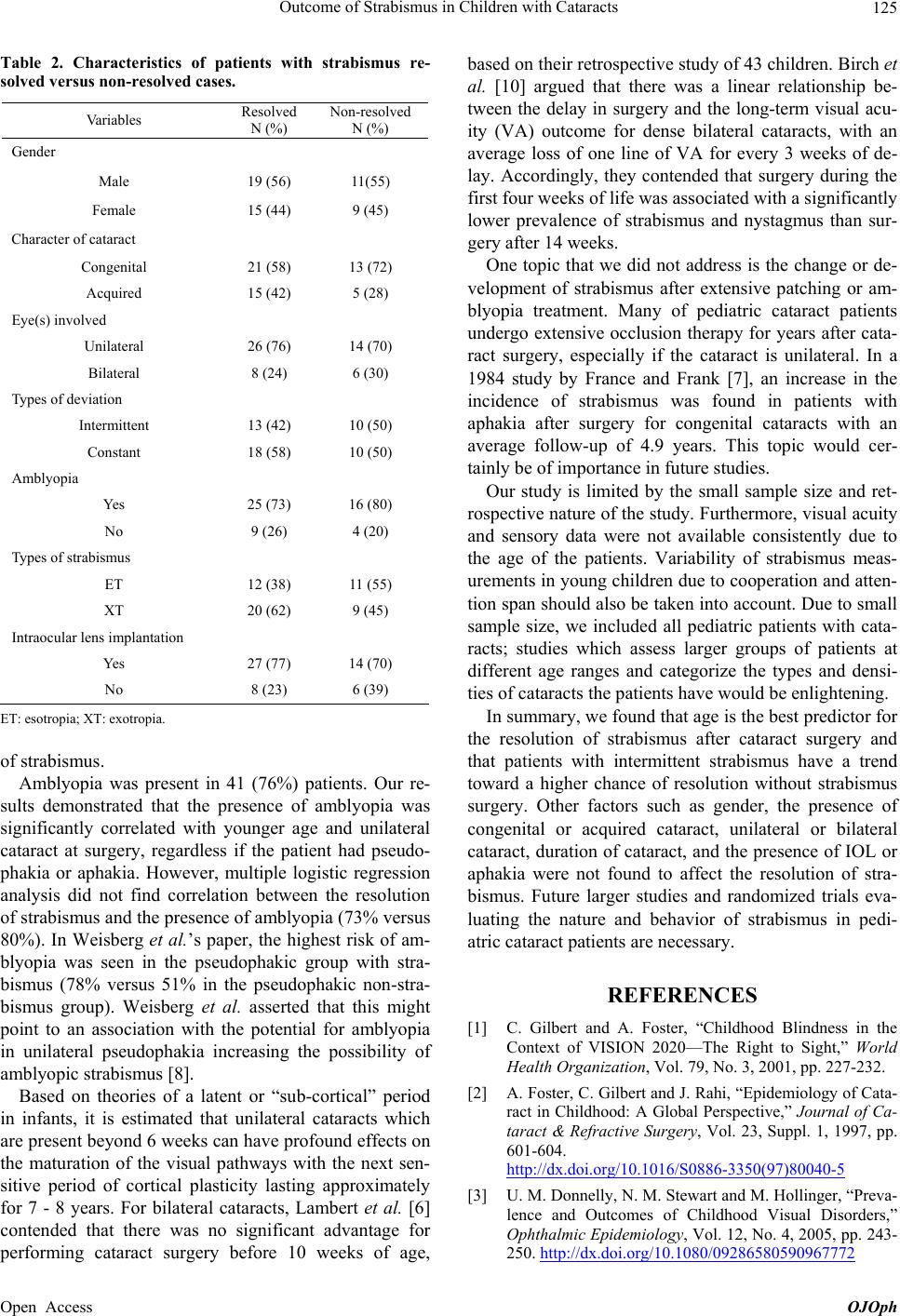
Table 2. Characteristics of patients with strabismus re-
solved versus non-resolved cases.
Va ri ab le s Resolved
N (%)
Non-resolved
N (%)
Gender
Male 19 (56) 11(55)
Female 15 (44) 9 (45)
Character of cataract
Congenital 21 (58) 13 (72)
Acquired 15 (42) 5 (28)
Eye(s) involved
Unilateral 26 (76) 14 (70)
Bilateral 8 (24) 6 (30)
Types of deviation
Intermittent 13 (42) 10 (50)
Constant 18 (58) 10 (50)
Amblyopia
Yes 25 (73) 16 (80)
No 9 (26) 4 (20)
Types of strabismus
ET 12 (38) 11 (55)
XT 20 (62) 9 (45)
Intraocular lens implantation
Yes 27 (77) 14 (70)
No 8 (23) 6 (39)
ET: esotropia; XT: exotropia.
of strabismus.
Amblyopia was present in 41 (76%) patients. Our re-
sults demonstrated that the presence of amblyopia was
significantly correlated with younger age and unilateral
cataract at surgery, regardless if the patient had pseudo-
phakia or aphakia. However, multiple logistic regression
analysis did not find correlation between the resolution
of strabismus and the presence of amblyopia (73% versus
80%). In Weisberg et al.’s paper, the highest risk of am-
blyopia was seen in the pseudophakic group with stra-
bismus (78% versus 51% in the pseudophakic non-stra-
bismus group). Weisberg et al. asserted that this might
point to an association with the potential for amblyopia
in unilateral pseudophakia increasing the possibility of
amblyopic strabismus [8].
Based on theories of a latent or “sub-cortical” period
in infants, it is estimated that unilateral cataracts which
are present beyond 6 weeks can have profound effects on
the maturation of the visual pathways with the next sen-
sitive period of cortical plasticity lasting approximately
for 7 - 8 years. For bilateral cataracts, Lambert et al. [6]
contended that there was no significant advantage for
performing cataract surgery before 10 weeks of age,
based on their retrospective study of 43 children. Birch et
al. [10] argued that there was a linear relationship be-
tween the delay in surgery and the long-term visual acu-
ity (VA) outcome for dense bilateral cataracts, with an
average loss of one line of VA for every 3 weeks of de-
lay. Accordingly, they contended that surgery during the
first four weeks of life was associated with a significantly
lower prevalence of strabismus and nystagmus than sur-
gery after 14 weeks.
One topic that we did not address is the change or de-
velopment of strabismus after extensive patching or am-
blyopia treatment. Many of pediatric cataract patients
undergo extensive occlusion therapy for years after cata-
ract surgery, especially if the cataract is unilateral. In a
1984 study by France and Frank [7], an increase in the
incidence of strabismus was found in patients with
aphakia after surgery for congenital cataracts with an
average follow-up of 4.9 years. This topic would cer-
tainly be of importance in future studies.
Our study is limited by the small sample size and ret-
rospective nature of the study. Furthermore, visual acuity
and sensory data were not available consistently due to
the age of the patients. Variability of strabismus meas-
urements in young children due to cooperation and atten-
tion span should also be taken into account. Due to small
sample size, we included all pediatric patients with cata-
racts; studies which assess larger groups of patients at
different age ranges and categorize the types and densi-
ties of cataracts the patients have would be enlightening.
In summary, we found that age is the best predictor for
the resolution of strabismus after cataract surgery and
that patients with intermittent strabismus have a trend
toward a higher chance of resolution without strabismus
surgery. Other factors such as gender, the presence of
congenital or acquired cataract, unilateral or bilateral
cataract, duration of cataract, and the presence of IOL or
aphakia were not found to affect the resolution of stra-
bismus. Future larger studies and randomized trials eva-
luating the nature and behavior of strabismus in pedi-
atric cataract patients are necessary.
REFERENCES
[1] C. Gilbert and A. Foster, “Childhood Blindness in the
Context of VISION 2020—The Right to Sight,” World
Health Organization, Vol. 79, No. 3, 2001, pp. 227-232.
[2] A. Foster, C. Gilbert and J. Rahi, “Epidemiology of Cata-
ract in Childhood: A Global Perspective,” Journal of Ca-
taract & Refractive Surgery, Vol. 23, Suppl. 1, 1997, pp.
601-604.
http://dx.doi.org/10.1016/S0886-3350(97)80040-5
[3] U. M. Donnelly, N. M. Stewart and M. Hollinger, “Preva-
lence and Outcomes of Childhood Visual Disorders,”
Ophthalmic Epidemiology, Vol. 12, No. 4, 2005, pp. 243-
250. http://dx.doi.org/10.1080/09286580590967772
Open Access OJOph