A Clinical Study of Pterygium and Results of Treatment by Excision and Limbal
Autograft or Augmented with Post-Op Mitomycin C
Open Access OJOph
101
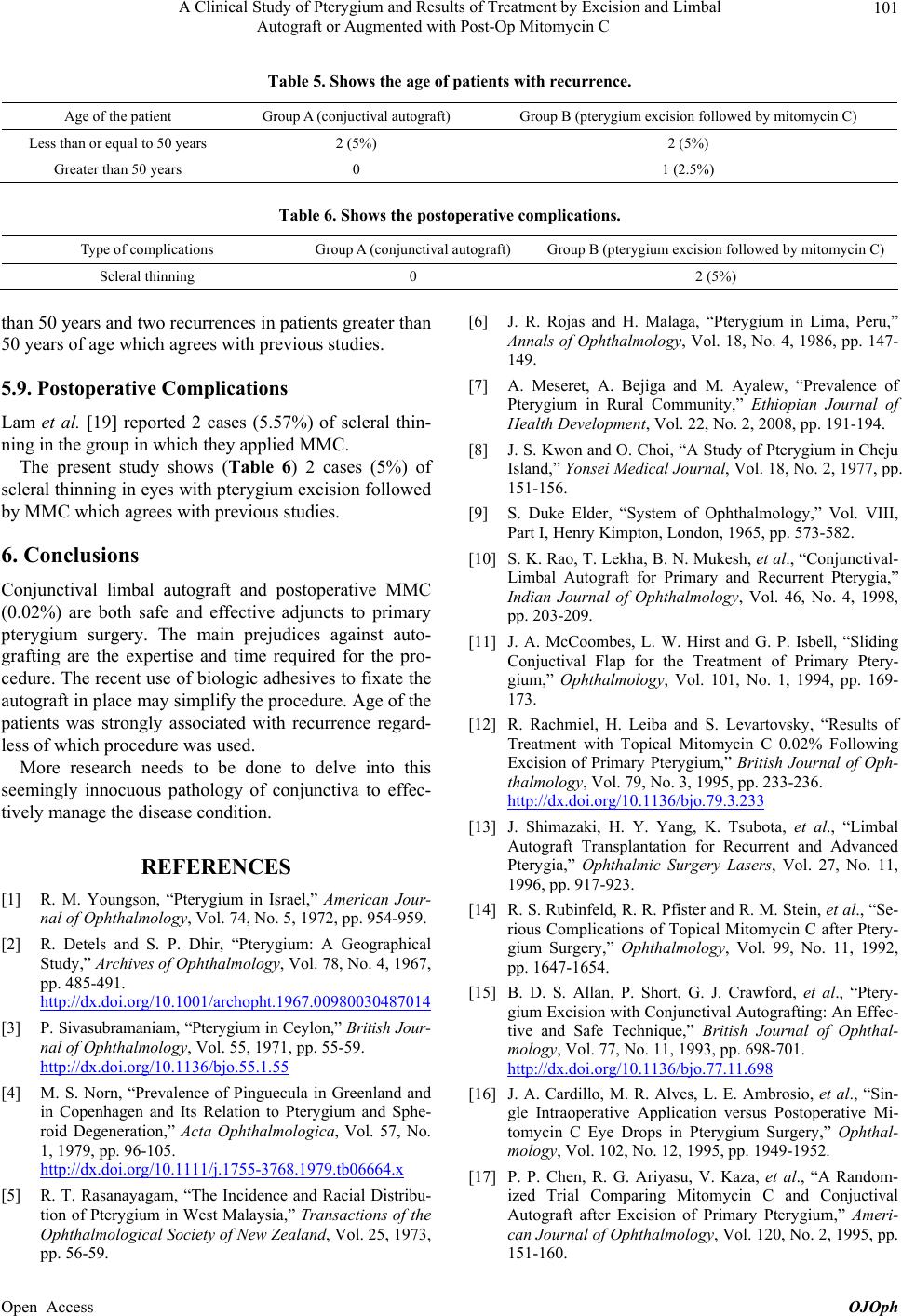
Table 5. Shows the age of patients with recurrence.
Age of the patient Group A (conjuctival autograft) Group B (pterygium excision f ollowed by mitomycin C)
Less than or equal to 50 years 2 (5%) 2 (5%)
Greater than 50 years 0 1 (2.5%)
Table 6. Shows the postoperative complications.
Type of complications Group A (conjunctival autograft) Group B (pterygium excision followed by mitomycin C )
Scleral thinning 0 2 (5%)
than 50 years and two recurrences in patients greater than
50 years of age which agrees with previous studies.
5.9. Postoperative Complications
Lam et al. [19] reported 2 cases (5.57%) of scleral thin-
ning in the group in which they applied MMC.
The present study shows (Table 6) 2 cases (5%) of
scleral thinning in eyes with pterygium excision followed
by MMC which agrees with previous studies.
6. Conclusions
Conjunctival limbal autograft and postoperative MMC
(0.02%) are both safe and effective adjuncts to primary
pterygium surgery. The main prejudices against auto-
grafting are the expertise and time required for the pro-
cedure. The recent use of biologic adhesives to fixate the
autograft in place may simplify the procedure. Age of the
patients was strongly associated with recurrence regard-
less of which procedure was used.
More research needs to be done to delve into this
seemingly innocuous pathology of conjunctiva to effec-
tively manage the disease condition.
REFERENCES
[1] R. M. Youngson, “Pterygium in Israel,” American Jour-
nal of Ophthalmology, Vol. 74, No. 5, 1972, pp. 954-959.
[2] R. Detels and S. P. Dhir, “Pterygium: A Geographical
Study,” Archives of Ophthalmology, Vol. 78, No. 4, 1967,
pp. 485-491.
http://dx.doi.org/10.1001/archopht.1967.00980030487014
[3] P. Sivasubramaniam, “Ptery gium in Ceylon,” British Jour-
nal of Ophthalmology, Vol. 55, 1971, pp. 55-59.
http://dx.doi.org/10.1136/bjo.55.1.55
[4] M. S. Norn, “Prevalence of Pinguecula in Greenland and
in Copenhagen and Its Relation to Pterygium and Sphe-
roid Degeneration,” Acta Ophthalmologica, Vol. 57, No.
1, 1979, pp. 96-105.
http://dx.doi.org/10.1111/j.1755-3768.1979.tb06664.x
[5] R. T. Rasanayagam, “The Incidence and Racial Distribu-
tion of Pterygium in West Malaysia,” Transactions of the
Ophthalmological Society of New Zealand, Vol. 25, 1973,
pp. 56-59.
[6] J. R. Rojas and H. Malaga, “Pterygium in Lima, Peru,”
Annals of Ophthalmology, Vol. 18, No. 4, 1986, pp. 147-
149.
[7] A. Meseret, A. Bejiga and M. Ayalew, “Prevalence of
Pterygium in Rural Community,” Ethiopian Journal of
Health Development, Vol. 22, No. 2, 2008, pp. 191-194.
[8] J. S. Kwon and O. Choi, “A Study of Pterygium in Cheju
Island,” Yonsei Medical Journal, Vol. 18, No. 2, 1977, pp.
151-156.
[9] S. Duke Elder, “System of Ophthalmology,” Vol. VIII,
Part I, Henry Kimpton, London, 1965, pp. 573-582.
[10] S. K. Rao, T. Lekha, B. N. Mukesh, et al., “Conjunctival-
Limbal Autograft for Primary and Recurrent Pterygia,”
Indian Journal of Ophthalmology, Vol. 46, No. 4, 1998,
pp. 203-209.
[11] J. A. McCoombes, L. W. Hirst and G. P. Isbell, “Sliding
Conjuctival Flap for the Treatment of Primary Ptery-
gium,” Ophthalmology, Vol. 101, No. 1, 1994, pp. 169-
173.
[12] R. Rachmiel, H. Leiba and S. Levartovsky, “Results of
Treatment with Topical Mitomycin C 0.02% Following
Excision of Primary Pterygium,” British Journal of Oph-
thalmology, Vol. 79, No. 3, 1995, pp. 233-236.
http://dx.doi.org/10.1136/bjo.79.3.233
[13] J. Shimazaki, H. Y. Yang, K. Tsubota, et al., “Limbal
Autograft Transplantation for Recurrent and Advanced
Pterygia,” Ophthalmic Surgery Lasers, Vol. 27, No. 11,
1996, pp. 917-923.
[14] R. S. Rubinfeld, R. R. Pfister and R. M. Stein, et al., “Se-
rious Complications of Topical Mitomycin C after Ptery-
gium Surgery,” Ophthalmology, Vol. 99, No. 11, 1992,
pp. 1647-1654.
[15] B. D. S. Allan, P. Short, G. J. Crawford, et al., “Ptery-
gium Excision with Conjunctival Autografting: An Effec-
tive and Safe Technique,” British Journal of Ophthal-
mology, Vol. 77, No. 11, 1993, pp. 698-701.
http://dx.doi.org/10.1136/bjo.77.11.698
[16] J. A. Cardillo, M. R. Alves, L. E. Ambrosio, et al., “Sin-
gle Intraoperative Application versus Postoperative Mi-
tomycin C Eye Drops in Pterygium Surgery,” Ophthal-
mology, Vol. 102, No. 12, 1995, pp. 1949-1952.
[17] P. P. Chen, R. G. Ariyasu, V. Kaza, et al., “A Random-
ized Trial Comparing Mitomycin C and Conjuctival
Autograft after Excision of Primary Pterygium,” Ameri-
can Journal of Ophthalmology, Vol. 120, No. 2, 1995, pp.
151-160.