The Emergence of Rapid Counter Immunostaining in the Controlled Narrow
Excision of Malignant Melanoma—How We Do It
1083
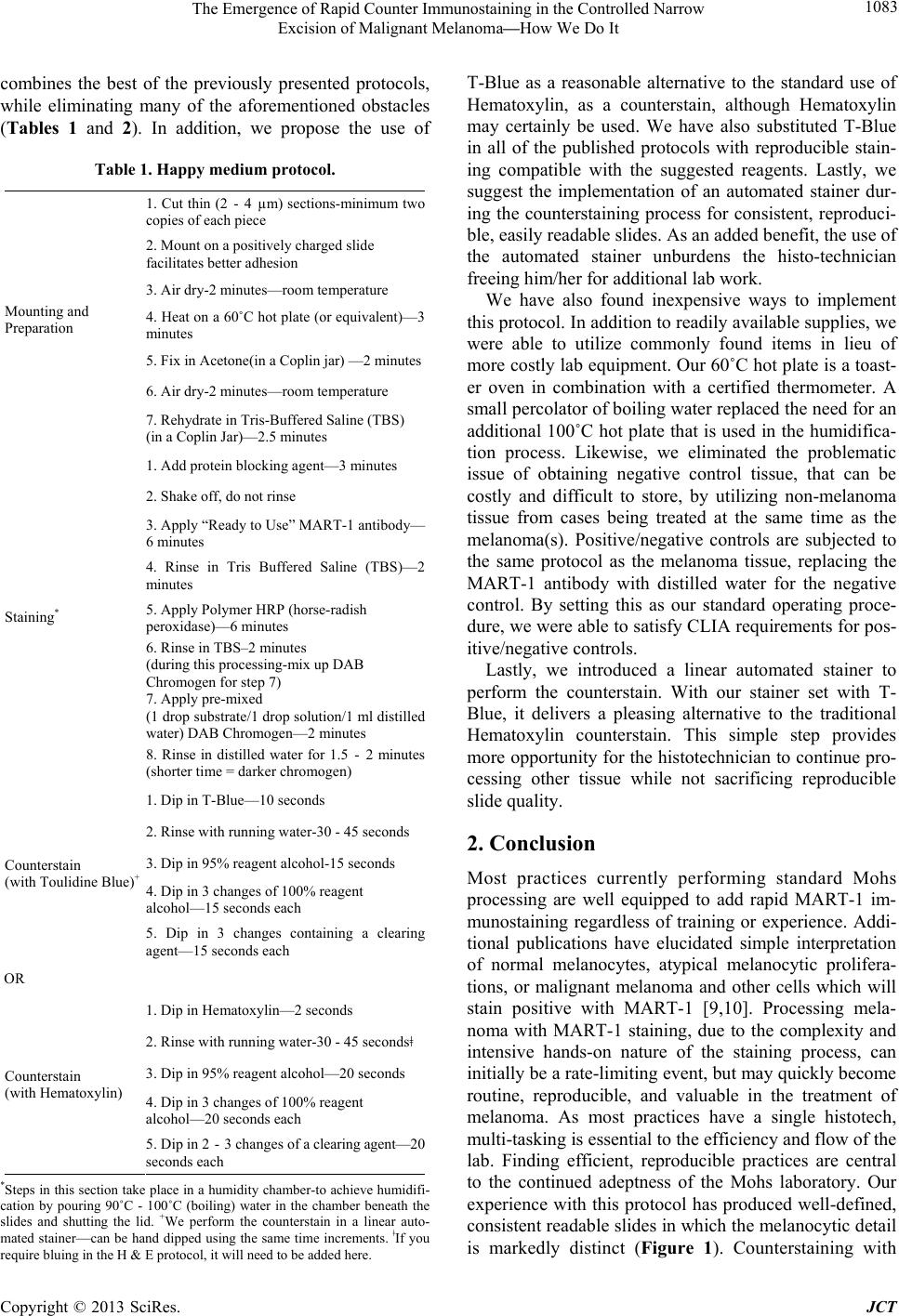
combines the best of the previously presented protocols,
while eliminating many of the aforementioned obstacles
(Tables 1 and 2). In addition, we propose the use of
Table 1. Happy medium protocol.
1. Cut thin (2 - 4 µm) sections-minimum two
copies of each piece
2. Mount on a positively charged slide
facilitates better adhesion
3. Air dry-2 minutes—room temperature
4. Heat on a 60˚C hot plate (or equivalent)—3
minutes
5. Fix in Acetone(in a Coplin jar) —2 minutes
6. Air dry-2 minutes—room temperature
Mounting and
Preparation
7. Rehydrate in Tris-Buffered Saline (TBS)
(in a Coplin Jar)—2.5 minutes
1. Add protein blocking agent—3 minutes
2. Shake off, do not rinse
3. Apply “Ready to Use” MART-1 antibody
6 minutes
4. Rinse in Tris Buffered Saline (TBS)—2
minutes
5. Apply Polymer HRP (horse-radish
peroxidase)—6 minutes
6. Rinse in TBS–2 minutes
(during this processing-mix up DAB
Chromogen for step 7)
7. Apply pre-mixed
(1 drop substrate/1 drop solution/1 ml distilled
water) DAB Chromogen—2 minutes
Staining*
8. Rinse in distilled water for 1.5 - 2 minutes
(shorter time = darker chromogen)
1. Dip in T-Blue—10 seconds
2. Rinse with running water-30 - 45 seconds
3. Dip in 95% reagent alcohol-15 seconds
4. Dip in 3 changes of 100% reagent
alcohol—15 seconds each
Counterstain
(with Toulidine Blue)+
5. Dip in 3 changes containing a clearing
agent—15 seconds each
OR
1. Dip in Hematoxylin—2 seconds
2. Rinse with running water-30 - 45 secondsǂ
3. Dip in 95% reagent alcohol—20 seconds
4. Dip in 3 changes of 100% reagent
alcohol—20 seconds each
Counterstain
(with Hematoxylin)
5. Dip in 2 - 3 changes of a clearing agent—20
seconds each
*Steps in this section take place in a humidity chamber-to achieve humidifi-
cation by pouring 90˚C - 100˚C (boiling) water in the chamber beneath the
slides and shutting the lid. +We perform the counterstain in a linear auto-
mated stainer—can be hand dipped using the same time increments. ǂIf you
require bluing in the H & E protocol, it will need to be added here.
T-Blue as a reasonable alternative to the standard use of
Hematoxylin, as a counterstain, although Hematoxylin
may certainly be used. We have also substituted T-Blue
in all of the published protocols with reproducible stain-
ing compatible with the suggested reagents. Lastly, we
suggest the implementation of an automated stainer dur-
ing the counterstaining process for consistent, reproduci-
ble, easily readable slides. As an added benefit, the use of
the automated stainer unburdens the histo-technician
freeing him/her for additional lab work.
We have also found inexpensive ways to implement
this protocol. In addition to readily available supplies, we
were able to utilize commonly found items in lieu of
more costly lab equipment. Our 60˚C hot plate is a toast-
er oven in combination with a certified thermometer. A
small percolator of boiling water replaced the need for an
additional 100˚C hot plate that is used in the humidifica-
tion process. Likewise, we eliminated the problematic
issue of obtaining negative control tissue, that can be
costly and difficult to store, by utilizing non-melanoma
tissue from cases being treated at the same time as the
melanoma(s). Positive/negative controls are subjected to
the same protocol as the melanoma tissue, replacing the
MART-1 antibody with distilled water for the negative
control. By setting this as our standard operating proce-
dure, we were able to satisfy CLIA requirements for pos-
itive/negative controls.
Lastly, we introduced a linear automated stainer to
perform the counterstain. With our stainer set with T-
Blue, it delivers a pleasing alternative to the traditional
Hematoxylin counterstain. This simple step provides
more opportunity for the histotechnician to continue pro-
cessing other tissue while not sacrificing reproducible
slide quality.
2. Conclusion
Most practices currently performing standard Mohs
processing are well equipped to add rapid MART-1 im-
munostaining regardless of training or experience. Addi-
tional publications have elucidated simple interpretation
of normal melanocytes, atypical melanocytic prolifera-
tions, or malignant melanoma and other cells which will
stain positive with MART-1 [9,10]. Processing mela-
noma with MART-1 staining, due to the complexity and
intensive hands-on nature of the staining process, can
initially be a rate-limiting event, but may quickly become
routine, reproducible, and valuable in the treatment of
melanoma. As most practices have a single histotech,
multi-tasking is essential to the efficiency and flow of the
lab. Finding efficient, reproducible practices are central
to the continued adeptness of the Mohs laboratory. Our
experience with this protocol has produced well-defined,
consistent readable slides in which the melanocytic detail
is markedly distinct (Figure 1). Counterstaining with
Copyright © 2013 SciRes. JCT