Food and Nutrition Sciences
Vol.05 No.20(2014), Article ID:50614,13 pages
10.4236/fns.2014.520208
Poverty Reduction and Pattern of Chronic Childhood Under-Nutrition in India: How Far Does the Link Exist?
Moumita Mukherjee
Independent Research Consultant, Atlanta, USA
Email: mukherjee.moumita3@gmail.com
Copyright © 2014 by author and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/



Received 13 August 2014; revised 10 September 2014; accepted 20 September 2014
ABSTRACT
In spite of an established link between poverty and under-nutrition in India, fall in under-nutri- tion is sluggish with fall in poverty. This research paper aims to seek answer on the effect of poverty decline on child under-nutrition in India over a period of one and a half decades. After examining the extent of association between poverty reduction and reciprocal changes in child under-nutrition, the paper found that although there was a definite influence of poverty levels on child under-nutrition at the state-level, the strength of the impact was not very high. This possibly explains why improvements in nutritional status among children have failed to keep up pace with steady reduction in mass poverty across the states in the last couple of decades. The results also strongly reiterate the magnificent role of child’s healthcare utilization and higher public spending which can help to capitalize on the increase in economic capabilities at the household level, resulting from robust economic growth and alleviation of endemic poverty.
Keywords:
Absolute Poverty, Chronic Under-Nutrition, India

1. Introduction
The link between poverty and under-nutrition among children has long been established [1] - [5] . Poverty leads to nutritional shortfalls and persistent hunger in many parts of the low income countries and consequently retards productive capacity and human capital [6] across the life-course and increases illness risks. It is thus natural that poverty alleviation strategies aim at reducing widespread under-nutrition as one of the central objectives [7] . However, research evidence is not clear on the causal link between changes in poverty rates in developing countries over time and under-nutrition prevalence [8] . This prevents to determine to what extent poverty reduction can be expected to influence under-nutrition and account for its magnitude and temporal changes through the pathways of other proximal and intervening variables like maternal education, household environment, care- giving and care-seeking etc. This paper aims to fill this gap and reconcile somewhat contradictory evidence in literature on the effect of poverty decline on child under-nutrition. Drawing on a state-level panel dataset for over a decade and a half from India, the primary motivation is generated from the fact that despite steady decline in poverty rates across the country, child under-nutrition has remained almost stagnant or has a sluggish reduction.
The extreme view in explaining this observed little disconnect between poverty decline and matching changes in child under-nutrition suggests an “weak association” assumption: under-nutrition levels and intertemporal changes are less proportionately related to poverty levels as well as poverty reduction over time [9] [10] . I contend instead that poverty reduction has a definite impact on child nutritional outcomes. However, the strength of the influence is contingent on a wider set of intervening factors, mostly socio-cultural and concerning public welfare. Likewise, I test whether the association is primarily due to the weak influence of poverty decline on nutritional status of children due to any apparent missing link in the causal chain, or through dampening of the effect declining poverty would have otherwise, but due to existing socioeconomic and supply-side “barriers”. As I find, the pure impact of poverty reduction on child under-nutrition is feeble and conditioned through indirect effects of mother’s education and access to health care. The slow and unequal improvements in these confounders explain the visible disconnect between declining poverty and stagnant nutritional status among Indian children.
2. Review of Literature
Two distinct and at times, conflicting strands of literature is identified on the linkages between poverty reduction and economic growth on the one hand and child nutritional outcomes on the other. While in South-Asia and in a range of Latin American and sub-Saharan African countries living standards and children’s nutritional status are found interrelated [5] [11] - [17] . It is found to be absent in countries like Mexico, Ecuador and Cambodia (Hong, et al., 2006). Poverty, access to health care and regional characteristics are among the few determinants of under-nutrition in Ghana [18] . In some developing countries, income growth improves nutrition outcomes but the trickle down effect is slow, long and indirect [7] . Navaneetham and Jose (2005) opines that absence or restricted access over resources—material, economic, socio-cultural—are the basic causes for endemic malnutrition in South Asia which in turn put children into vulnerable situation by leading to inadequate dietary intake and infections to disease, leading ultimately to chronic under-nutrition. In Vietnam, Glewwe et al. (2002) finds that although both household incomes grew and nutritional status improved among Vietnamese children during the 1990s, yet there is no significant impact of the former at the household level. In explaining, the authors highlight the potential role of positive societal changes (for e.g. higher public spending on health, improved access and quality of health services etc.) which essentially mediate any beneficial effects of income growth on child nutritional status [19] . For India, Radhakrishna et al. (2006) have found similar evidence; elimination or reduction of poverty does not necessitate a matching reduction in child under-nutrition. At the opposite end of the spectrum, Smith and Haddad (2002) analyzes cross-country panel data for 1970-1996 for 62 countries, and finds a strong impact of per capita national income on improvements in child nutritional status, which, in their opinion is brought about through positive accompanying changes—public and private investments in health, national food availability, women’s education and status and quality of household environment.
It thus seems apparent from the literature that, even modest influence of poverty reduction on child under-nu- trition, requires simultaneous improvements in other measures of household welfare and socioeconomic status, backed by a resilient health system ensuring improved access and quality of services. Based on a simple empirical model, emerging out of a framework of the possible pathways of influence of a basic determinant of under- nutrition-changes in poverty headcount rates-on the changing levels of child under-nutrition, I examine the poverty-under-nutrition linkage for state-level panel data for India and test how far poverty reduction has influenced child under-nutrition.
The rest of the paper is organized as follows: Section 3 introduces the empirical model. Section 4 describes the dataset constructed for the paper, the variables used and estimation strategies. Section 5 presents the results while Section 6 discusses the salient findings. Section 7 concludes.
3. The Empirical Model
There is an extensive volume of literature on the determinants of child under-nutrition [8] [14] focusing on de- veloping countries, and mostly governed by common theoretical and empirical frameworks. The well-acknowl- edged practice seems to consider a set of “basic” parameters such as poverty, which conditioned by the prevailing socio-cultural environment, influences more “proximal” determinants such as available resources for food- security, infant and child care and health services. These proximal determinants influence child nutritional status through the “intervening” effect of household food security, maternal and child health care and use of health services [20] - [22] . A typical pathway of influence of poverty on child nutritional status is illustrated in Figure 1.
In my empirical specification, along the broad lines of the framework outlined in Figure 1, I model the determinants of child nutritional status at the state-level, considering average poverty headcount rates as a basic determinant.
Figure 1. Conceptual framework for the determinants of child nutritional status. Source: adapted from UNICEF (1990, 1998).
4. Data, Variables and Estimation Methods
Both poverty and nutritional status of children are dynamic processes changing over time1. Estimating causal models based on cross-sectional microdata, at an individual level for any relationships between the two thus reveals only partial information [8] . However, in most developing countries representative longitudinal information on poverty and nutritional status are rare, forcing researchers to resort to alternative approaches. In this paper, I use a specially constructed state-level panel data for India for the period 1992-2006. The states are the individual observational units in my data, and I study the impact of changes in the levels of poverty headcount rates on changes in average under-nutrition in terms of stunting or low height-for-age distribution. Such a synthetic dataset relies naturally on a number of alternative data sources, ideally pertaining to same time-periods. My data is for 15 states in India. The analysis is regarding 15 major states only. The panel of states is observed for three time periods, 1992-1993, 1998-1999 and 2005-2006, the periods being chosen to match with the successive rounds of the Indian DHS (known commonly as National Family Health Survey—NFHS). Anthropometric information of children, my indicator of under-nutrition is for children under three years, to conform to different NFHS rounds.
4.1. Data
Data on percentage of population below poverty line is from National Human Development Report 2001 [23] published by the Planning Commission, India. I use data on coverage of the Public Distribution System (PDS) and per capita health expenditure of Government of India from other different sources [24] - [27] . I calculate all state-specific averages of other variables such as mother’s education, mean duration of breastfeeding, proportion of population having access to safe drinking water, average percentage of fully immunized children from three rounds of NFHS.
4.2. Methods
Description of variables: The outcome variable of concern is child nutritional status, which I measure in terms of height-for-age z-scores for an individual child’s standard deviations from that of a reference population (for details, IIPS 2007) [28] . Also referred as stunting, I take the state averages for proportion of children having the height-for-age z scores two standard deviations below that of the reference population. Average stunting reflects chronic and thus more pervasive form of under-nutrition, besides a popular summary indicator of the same [29] [30] .
I incorporate the principal causal factor poverty as an absolute index; I use poverty headcount rates (percentage of state population below state-specific poverty lines) as the poverty indicator. An important issue in this context is the choice of the time periods for the model covariates. Short term fluctuations and contemporaneous changes in poverty, state-specific food availability as well as Government’s spending on health affect stunting less, rather it may be more responsive to changes in these parameters occurring in past and near past [3] [10] . This typically lagged nature of the relationship between the causal factors and under-nutrition resembles a dynamic relationship. However, I do not model the relationship in a strict dynamic sense, I simply allow for the “lag” by using the economic indicators (including poverty rates) and most of the other controls for a few periods preceding the NFHS years i.e. NFHS I, II & III [28] [31] [32] for which I have the stunting data. A detail explanation of each variable, its sources and year of information is available in the Appendix.
As discussed in the conceptual framework and the empirical model, I consider a rich set of controls in the form of direct and intermediate determinants of child under-nutrition. The frameworks as well as standard models in the literature govern the choice of the variables [3] [33] . In the models economic variable except income poverty include data on per capita allocation of food grains under the PDS to each state (per annum) as an indicator of food security2. Average years of schooling for mothers and mean duration of breastfeeding are indicators of mother’s knowledge, attitude, belief and practice about childcare. Breastfeeding also indicates the child’s pattern of food intake. Household environment and health service coverage variables include percentage of population having access to safe drinking water3, percentage of fully immunized children less than two years of age and per capita public expenditure on health4.
4.3. Model Estimation
The econometric estimation of the above is relatively straightforward; I employ reduced form estimating equations as follows:
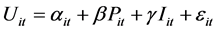
where  denotes percentage of children whose HAZ score is below −2 SD from the median HAZ score of the reference population in state i in time-period t,
denotes percentage of children whose HAZ score is below −2 SD from the median HAZ score of the reference population in state i in time-period t,  incorporates time-varying state-level fixed-effects,
incorporates time-varying state-level fixed-effects,  represents poverty headcount ratios and
represents poverty headcount ratios and  is a vector of time-varying control factors and
is a vector of time-varying control factors and  is a state-level idiosyncratic error. This specification observes the strength and significance of
is a state-level idiosyncratic error. This specification observes the strength and significance of , to test for the hypothesis that absolute levels of poverty have effect on observed average levels of stunting. Under the assumption of strict exogeneity of all regressors, I first estimate the above specification as a pooled cross-sectional Ordinary Least Square (OLS) regression model; I later allow state-specific fixed and random effect intercept terms in subsequent models considering the panel-data arrangement of the variables. I am not doing a variant of above, including state-time dummies, to control for aggregate time trends in changes in the levels of average stunting due to huge loss of degrees of freedom [34] . I subsequently relax the strict exogeneity assumption, allowing for possible correlation between
, to test for the hypothesis that absolute levels of poverty have effect on observed average levels of stunting. Under the assumption of strict exogeneity of all regressors, I first estimate the above specification as a pooled cross-sectional Ordinary Least Square (OLS) regression model; I later allow state-specific fixed and random effect intercept terms in subsequent models considering the panel-data arrangement of the variables. I am not doing a variant of above, including state-time dummies, to control for aggregate time trends in changes in the levels of average stunting due to huge loss of degrees of freedom [34] . I subsequently relax the strict exogeneity assumption, allowing for possible correlation between  and
and , leading to endogenous regression models. I employ two-stage least square regressions, instrumenting breastfeeding and health service uptake by income poverty and mother’s education. I apply standard econometric tests to choose between competing models and decide on the preferred specification. I apply Hausman specification tests for suitability of fixed and random effect models5; I test suitability of random-effects models over the conventional pooled ordinary least square regression applying the Breusch- Pagan Lagrangian Multiplier (LM) tests for random effects6 [31] . Endogeneity may be a concern, but at the aggregate level there is no good way to address the problem using instrumental variables.
, leading to endogenous regression models. I employ two-stage least square regressions, instrumenting breastfeeding and health service uptake by income poverty and mother’s education. I apply standard econometric tests to choose between competing models and decide on the preferred specification. I apply Hausman specification tests for suitability of fixed and random effect models5; I test suitability of random-effects models over the conventional pooled ordinary least square regression applying the Breusch- Pagan Lagrangian Multiplier (LM) tests for random effects6 [31] . Endogeneity may be a concern, but at the aggregate level there is no good way to address the problem using instrumental variables.
Tests for endogeneity7 of the regressors and the suitability of instrumental variable (IV) estimators include, among others, the Durbin-Wu-Hausman test and a related Wu-Hausman F test as well as Davidson-Mackinnon test available as standard routines in common econometric software packages. I apply these tests against any significant extent of the problem of endogeneity.
National Women’s Sample Weights as available in NFHS rounds are used to estimate the stunting prevalence, and to run regression analyses to try and maximize the representativeness of the sample in terms of the size, distribution, and characteristics of the study population.
I present the results for fitted models and parameter estimates in the results section calculated in STATA8. All models report heteroscedasticity-adjusted robust standard errors.
5. Results
5.1. Data Exploration
At the next step I scrutinize the sample distribution of all variables in terms of their descriptive statistics (Table 1). Since for linear regression to yield good estimates I need all variables to conform to normal distribution, hence, depending on the descriptive measures I check whether the data are reasonably symmetric and, if so, whether the tails are sufficiently thin or not. If the mean is larger than median then the distributions are positively skewed and the opposite would be the case for median exceeding the mean value. The analysis of the Inter Quartile Range (IQR) helps to decide whether the tails of the distribution are thinner or fatter than a regular normal distribution. On the basis of IQR I estimate a pseudo standard deviation9. If this is smaller than the standard deviation then the tails are heavier than normal. Thus, an idea about the required transformation of the data can be formed by comparing mean-based vis-à-vis order-based statistics of the data when one is trying to model an average behavior [38] .
Among variables, PDS coverage has positively skewed distribution with fatter tail. Ladder transformation created log transformation of PDS coverage.
5.2. Association between Poverty Headcount and Chronic Under-Nutrition in India
Let us first consider the average effects models for the specification in (1) in Table 2. Ignoring the time-ordering of the state level observations, the random effect model is significant in (A-D) compared to OLS regression according to Breusch-Pagan LM test for random effects but fixed effect models are preferred according to Hausman test after controlling state group dummies. Therefore in the aggregate model, I find that, time-varying fixed effects of factors are significantly influencing the stunting pattern.
I also ran the two stage least square model where I take childcare and feeding, child’s health seeking in any state depend upon state level income poverty and average years of mother’s education. Durbin-Wu-Hausman χ2 test and Wu-Hausman F test show that endogeneity is significant. Hausman test shows that fixed effect model is consistent and efficient. Then Davidson-MacKinnon test of exogeneity shows that endogeneity is not significant. Here I dropped the IV model as at aggregate level, there is no good way to test endogeneity using instrumental variables.
Model A has the only covariate income poverty indicating highly significant association with the chronic childhood under-nutrition. In model B, I control only immediate influencing factors where magnitude of influ-
Table 1. Descriptive statistics.
Table 2. Parameter estimates of association between pattern of average levels of poverty headcount ratio and pattern of under-nutrition.
Significance level: *p < 0.1; **p < 0.05; ***p < 0.01.
ence of income poverty is reduced but it is highly significant as before. However child’s health seeking also has significant influence. In model C, I control intermediate determinants along with proximate ones. In line with the common previous findings in numerous household-level cross sectional studies [39] , I still find significant impact of poverty on average stunting with less magnitude compared to previous models. In model D, I control one distant factor, per capita public expenditure on health along with proximate and intermediate factors which itself is not significant but with incorporation of this factor, significance of poverty vanishes. Incorporation of state-group10 dummies controls state level heterogeneity and therefore a significant test statistic for the Hausman specification test rules in favour of the fixed effects model (or more appropriately, against the suitability of random effects specification, according to Cameron and Trivedi 2009) [40] . Thus there seems to be a significant fixed group effect in the state-level panel. Again I should mention, endogeneity may be a concern, but at the aggregate level there is no good way to address the problem using instrumental variables. Also I should mention that since I am working only with three time points, First Difference and Fixed Effect models are therefore same. Thus I am not using First Difference model.
Table 3 depicts the proportion of contribution of model covariates to stunting of children under the age of three in fifteen major Indian states considering three time points.
Now I interpret the percentage contribution of different influencing factors following the conceptual framework [14] along with support of existing literatures. In model 1 with only covariate income poverty, its contribution is 33 percent. Inclusion of proximate factors in model 2 causes massive reduction in income poverty’s direct contribution (17 percent). Child’s health service uptake shows 39 percent influence. Moreover, literature has evidence to the fact that poverty influences child’s health seeking in low and middle income countries
Table 3. Regression based decomposition of observed variance accounted by each of the model covariates.
[41] - [45] . Poorer children seek health care less compared to richer children (ibid.). In India also different works suggest the same starting from neonatal care to treatment seeking of any ailment of children [46] . Thus, I can argue that poverty influences through these factors. When I incorporate underlying factors, income poverty’s direct influence reduces to 8 percent and major contributors are health service uptake (17 percent) and mother’s education (35 percent). After incorporating per capita public expenditure on health, influence of poverty becomes only 4 percent and major contributors are mother’s education (27 percent) and health expenditure (22 percent).
It indicates that at state level, social services are associated with less stunting and increase in Government’s health outlay can help to break the vicious circle of poverty and under-nutrition at macro level. But, it is unable to capture the inherent inequalities at micro levels i.e. whether the same factors have random effects at micro levels. More in-depth research is necessary to explore the research problem.
6. Discussion
Over a major part of the last couple of decades, India and most of her states are experiencing a steady decline in income poverty (as measured by poverty headcount ratios). At the same time, changes in chronic child under-nutrition which is an important development indicator and summary measure of population welfare fails to keep up pace with the positive income effects that accompanies poverty reduction. For example, during 1992-2005, poverty rates show a decrease by about 17 percent on an average across the states, but stunting prevalence shows the same by only about 8 percent. Does this suggest that poverty reduction, at best, can be only hypothesized to have a small influence in improving child nutritional outcomes? At an aggregate level, however, average levels of poverty correlates well with that of chronic child under-nutrition across Indian states. But this does not prove that why the ratio of their change is much less than one. It is clear from fixed effect models that decline in under-nutrition is significantly associated with decline in poverty but when I control other influencing factors, the significance becomes weaker and finally no longer exists. Furthermore, strength of such broad measures of association intensifies during the recent years; for the major states correlation coefficient between average poverty headcount and child stunting rates increases from 0.483 in 1992-1993 to 0.552 in 2005-2006. In 2005-2006, almost all the states (with possible exception of Tamil Nadu) having lower levels of child stunting also have lower levels of poverty. States nevertheless vary widely in relative achievement in reduction of both these parameters. Ten states show achievement of higher reduction in child under-nutrition compared to the national average but only Tamil Nadu, Bihar, West Bengal show faster decline in poverty as well.
A causal analysis attempting to link the two phenomena is not however straightforward. In the present work, it is of primary interest to test the significance of association between absolute levels and the change in poverty and the same related to chronic under-nutrition controlling for other potential confounders.
The results from my empirical specification suggest that average levels of poverty over time wield significant influence on observed levels of under-nutrition rates across the Indian states. In fact, child’s health seeking has strong impact; no other variable has additional significant impact. Poverty has a significant magnitude of effect on child under-nutrition, although the influence is not statistically significant after controlling for the effect of Government’s health outlay. It would, therefore, be incorrect to assume that child under-nutrition levels are independent of poverty reduction, though it is equally naïve to consider that poverty reduction, through a direct income-effect and a subsequent clearly visible “trickling-down” of indirect positive externalities, will automatically improve child nutritional outcomes. My model does not claim a strong predictive ability; nevertheless, the results highlight that I can obtain greater leverage from poverty reduction, if accompanying and more far-fetch- ing changes are made in knowledge and practice of childcare, health seeking and also effective supply-side interventions.
Moreover, huge body of literature—theoretical as well as empirical—is evidence for the fact that poverty influences child’s health outcomes in low and middle income countries though different researchers use different poverty measures where some of them based their work on relative poverty measure [2] [5] [18] . Some works are based on differential impact of income growth [47] . My work is different from previous works as it takes poverty headcount ratio as the main influencing factor like Svedberg (2008). I interpret models and decomposition results in the light of these literatures and others. First, the impact of poverty through the pathway of proximate factors like dietary habits and health seeking is visible in early literature also. Poorer children seek health care less compared to richer children [41] - [44] . In India also different works suggest the same starting from neonatal care to treatment seeking of any ailment of children [48] . In another study on Bangladesh, household’s wealth status still remain significant determinant after adjusting for child’s mean duration of breastfeeding [18] . Thus I can argue that poverty influences along with these factors [2] [18] . Literatures I mention above and many other studies prove empirically that mother’s education is a crucial determinant of child’s healthcare seeking as well as child’s nutritional status [2] [18] [49] [50] . I can argue that since educational level of mother—proxy indicator of mother’s knowledge about childcare, social beliefs and practice of child care—is lower in poor families compared to richer families [25] , utility of government health spending reaches poor families less. As the rich and the poor are equally eligible to consume government provision of healthcare services, more aware richer people consume more health care even from Government facility compared to poorer children; thus Government’s health outlay also reaches poor less.
A few similar observations I find in cross-national study of Smith and Haddad (2002) and intra-national study in Svedberg (2008). The findings also underscore the importance of supplementary socio-cultural changes in explaining the apparent disconnect between steady economic growth and stalling child under-nutrition levels in other developing countries [51] [52] . But the results of the present study partially lend support to the premise that both poverty reduction and matching social sector reforms that aid improving human development indicators and public sector health interventions form the ideal recipe for improving child nutritional outcomes.
The present study has a few limitations, common to aggregate studies of similar scope. Firstly, measurement biases arising out of data for several of the variables pertaining to different time-periods and through different agencies (for e.g. survey estimates, official publications of government agencies) can influence the results. The key variables of interest—under-nutrition rates for individual states—use different definitions (in terms of coverage age-groups) in different NFHS waves, which I adjust to ensure conformity across NFHS rounds and individual states. Any such errors can influence results, if they are not purely random. Secondly, the synthetic panel I use is a short one. The models on average levels use 45 observations. It is well acknowledged that regression coefficient estimates, and power of certain econometric tests of hypothesis are susceptible to sample sizes. Hence, I make any conclusion with caution, and at best, as indicative. Lastly, although I try to wipe out unobserved heterogeneity allowing specific intercept terms, one can miss out systematically on parameter(s) that may cause the results to be biased in either direction.
7. Conclusion
This paper examines the extent of association between poverty reduction and reciprocal changes in child under- nutrition, to find that although there is a definite influence of poverty levels and its intertemporal changes on child under-nutrition at the state-level, the strength of the impact is not very high. This possibly explains why improvements in nutritional status among children have failed to keep up pace with steady reduction in mass poverty across the states in the last couple of decades. The results also strongly reiterate the sublime role of maternal education and higher public spending that can help to capitalize on the increase in economic capabilities at the household level, resulting from robust economic growth and alleviation of endemic poverty.
Acknowledgements
I dedicate my work to my mother project Future Health Systems Research Project Consortium and especially to my Doctoral Supervisor Prof. Barun Kanjilal and my senior ex-colleague Dr. Sumit Mazumdar. Because both of them built up the idea of the paper and helped me to find the right data sources, developing every step and methodology as well as the conclusion of the paper.
References
- Deolalikar, A. (2004) Poverty and Child Malnutrition in Bangladesh. The World Bank.
- Svedberg, P. (2000) Poverty and Under-Nutrition: Theory, Measurement and Policy. Oxford University Press, New York. http://dx.doi.org/10.1093/0198292686.001.0001
- Svedberg, P. (2008) Why Malnutrition in Shining India Persists. 4th Annual Conference on Economic Growth and Development, New Delhi.
- Navaneetham, K. and Jose, S. (2005) Poverty, Malnutrition and Mortality in South Asia: A Review of Issues and Options. CICRED Seminar on Mortality as Both a Determinant and a Consequence of Poverty and Hunger, Thiruvananthapuram, 1-21.
- Hong, R. and Mishra, V. (2006) Effect of Wealth Inequality on Chronic Under-Nutrition in Cambodian Children. Journal of Health and Population Nutrition, 24, 89-99.
- Dasgupta, P. and Ray, D. (1986) Inequality as a Determinant of Malnutrition and Unemployment: Theory. The Economic Journal, 96, 1011-1034. http://dx.doi.org/10.2307/2233171
- Shekar, M. and Lee, Y. (2006) Mainstreaming Nutrition in Poverty Reduction Strategy Papers: What Does It Take? A Review of the Early Experience. Health Nutrition and Population Discussion Paper, The World Bank.
- Smith, L.C. and Haddad, L.J. (2002) How Potent Is Economic Growth in Reducing Under-Nutrition? What Are the Pathways of Impact? New Cross-Country Evidence. Economic Development and Cultural Change, 51, 55-76. http://dx.doi.org/10.1086/345313
- Glewwe, P. (2002) Schools and Skills in Developing Countries: Education Policies and Socioeconomic Outcomes. Journal of Economic Literature, 40, 436-482. http://dx.doi.org/10.1257/jel.40.2.436
- Radhakrishna, R., Rao, K.H., Ravi, C. and Reddy, B.S. (2006) Estimation and Determination of Chronic Poverty in India: An Alternative Approach. Paper Presented at the CPRC Workshop on Concepts and Methods for Analysing Poverty Dynamics and Chronic Poverty, Chancellors Conference Center, University of Manchester.
- Poel, E., Hosseinpoor, A., Speybroeck, N., Ourti, T. and Vega, J. (2008) Socioeconomic Inequality in Malnutrition in Developing Countries. Bulletin of the World Health Organization, 86, 282-291. http://dx.doi.org/10.2471/BLT.07.044800
- Zere, E. and McIntyre, D. (2003) Inequities in Under-Five Child Malnutrition in South Africa. International Journal for Equity in Health, 2, 7.
- Fotso, J.C. (2006) Child Health Inequities in Developing Countries: Differences across Urban and Rural Areas. International Journal for Equity in Health, 5, 9.
- Smith, L.C. and Haddad, L.J. (1999) Explaining Child Malnutrition in Developing Countries: A Cross-Country Analysis. Research Reports 111, International Food Policy Research Institute, Washington DC.
- Pongou, R., Ezzati, M. and Salomon, J.A. (2006) Household and Community Socioeconomic and Environmental Determinants of Child Nutritional Status in Cameroon. BMC Public Health, 6, 98.
- Larrea, C. and Freire, W. (2002) Social Inequality and Child Malnutrition in Four Andean Countries. Revista Panamericana de Salud Pública, 11, 356-364. http://dx.doi.org/10.1590/S1020-49892002000500010
- Taguri, A., Betilmal, I., Mahmud, S.M., Ahmed, A.M., Goulet, O., Galan, P. and Hercberg, S. (2008) Risk Factors for Stunting among Under-Fives in Libya. Public Health Nutrition, 12, 1141-1149. http://dx.doi.org/10.1017/S1368980008003716
- Hong, R., Banta, J. and Betancourt, J. (2006) Relationship between Household Wealth Inequality and Chronic Childhood Under-Nutrition in Bangladesh. International Journal for Equity in Health, 5, 15. http://dx.doi.org/10.1186/1475-9276-5-15
- Poel, E., Hosseinpoor, A., Appiah, C., Vega, J. and Speybroeck, N. (2007) Malnutrition and the Disproportional Burden on the Poor: The Case of Ghana. International Journal for Equity in Health, 6, 21.
- The United Nations Children’s Fund (1990) Strategy for Improved Nutrition of Children and Women in Developing Countries. UNICFF, New York.
- The United Nations Children’s Fund (1998) The State of the World’s Children. UNICFF, New York.
- Engle, P.L., Bentley, M. and Pelto, G. (2000) The Role of Care in Nutrition Programmes: Current Research and a Research agenda. Proceedings of the Nutrition Society, 59, 25-35. http://dx.doi.org/10.1017/S0029665100000045
- (2001) National Human Development Report 2011. Planning Commission, Government of India.
- www.CEHAT.org
- The World Health Organization (2010) Water Related Diseases. http://www.who.int/water_sanitation_health/diseases/malnutrition/en/
- The World Health Organization (1978) Expanded Program on Immunization. Report and Working Papers. 31st Session of the WHO Regulatory Committee Mongolia, SEARO, 21-28 August 1978.
- www.indiastat.com
- International Institute for Population Sciences (IIPS) and ORC Macro (2007) National Family Health Survey (NFHS-2), 2005-2006. IIPS, Mumbai.
- Pradhan, M. and Prescott, N. (2002) Social Risk Management Options for Medical Care in Indonesia. Health Economics, 11, 431-446.
- Milman, A., Frongillo, E.A., Onis, M. and Hwang, J. (2005) Differential Improvement among Countries in Child Stunting Is Associated with Long-Term Development and Specific Interventions. Journal of Nutrition, 135, 1415- 1422.
- International Institute for Population Sciences (IIPS) and ORC Macro (1994) National Family Health Survey (NFHS-2), 1992-1993. IIPS, Mumbai.
- International Institute for Population Sciences (IIPS) and ORC Macro (2000) National Family Health Survey (NFHS-2), 1998-1999. IIPS, Mumbai.
- Smith, L.C., Ramakrishnan, U., Ndiaye, A., Haddad, L.J. and Martorell, R. (2003) The Importance of Women’s Status for Child Nutrition in Developing Countries. Research Reports 131, International Food Policy Research Institute, Washington DC.
- Baltagi, B.H. and Boozer, M.A. (1997) Econometric Analysis of Panel Data, Econometric Theory. Cambridge University Press, Cambridge, 747-754.
- Davidson, R. and MacKinnon, J.G. (1993) Estimation and Inference in Econometrics. Oxford University Press, New York, 237-240.
- Wooldridge, J. (2000) Introductory Econometrics: A Modern Approach. South-Western College Publishing, New York, 483-484.
- Fiorio, C.V. and Jenkins, S.P. (2008) INEQRBD: Stata Module to Calculate Regression-Based Inequality Decomposition. Statistical Software Components S456960, Boston College Department of Economics.
- Mukherjee, C., White, H. and Wuyts, M. (1998) Econometrics and Data Analysis for Developing Countries. Business and Economics, Psychology Press.
- Mazumdar, S. (2010) Determinants of Inequality in Child Malnutrition in India: The Poverty-under-Nutrition Linkage. Asian Population Studies, 6, 307-333. http://dx.doi.org/10.1080/17441730.2010.512763
- Cameron, A.C. and Trivedi, P.K. (2009) Microeconometrics Using Stata. Stata Press, College Station.
- Mahal, A., Singh, J., Afridi, F., Lamba, V., Gumber, A. and Selvaraju, V. (2000) Who Benefits from Public Spending in India? Working Paper, National Council of Applied Economic Research, New Delhi.
- Black, R.E., Allen, L.H., Bhutta, Z.A., Caulfield, L.E., Onis, M., Ezzati, M., Mathers, C. and Rivera, J. (2008) Maternal and Child Under-Nutrition: Global and Regional Exposures and Health Consequences. The Lancet, 371, 243-260.
- Peters, D.H., Garg, A., Bloom, G., Walker, D.G., Brieger, W.R. and Rahman, M.H. (2008) Poverty and Access to Health Care in Developing Countries. Annals of the New York Academy of Sciences, 1136, 161-171. http://dx.doi.org/10.1196/annals.1425.011
- Mahal, A., Yazbeck, A.S., Peters, D.H. and Ramana, G.N.V. (2001) The Poor and Health Service Use in India. Health, Nutrition and Population Discussion Paper, The World Bank, Washington DC.
- Yazbeck, A.S. (2009) Attacking Inequality in the Health Sector. A Synthesis of Evidence and Tools. The World Bank, Washington DC. http://dx.doi.org/10.1596/978-0-8213-7444-3
- Menon, P., Ruel, M.T. and Morris, S.S. (2000) Socio-Economic Differentials in Child Stunting Are Consistently Larger in Urban than in Rural Areas. Food and Nutrition Bulletin, 21, 282-289.
- Heltberg, R. (2009) Malnutrition, Poverty and Economic Growth. Health Economics, 18, 77-88. http://dx.doi.org/10.1002/hec.1462
- Kanjilal, B., Mazumdar, P.G., Mukherjee, M. and Rahaman, M.H. (2010) Nutritional Status of Children in India: Household Socio-Economic Condition as the Contextual Determinant. International Journal for Equity in Health, 9, 19. http://dx.doi.org/10.1186/1475-9276-9-19
- Wagstaff, A. (2002) Poverty and Health Sector Inequalities. Bulletin of the World Health Organization, 80, 97-105.
- Linnermayr, S., Alderman, H. and Ka, A. (2008) Determinants of Malnutrition in Senegal: Individual, Household, Community Variables and Their Interaction. Economics & Human Biology, 6, 252-263. http://dx.doi.org/10.1016/j.ehb.2008.04.003
- Garcia, M. (1994) Malnutrition and Food Insecurity Projections, 2020. 2020 Brief No. 6, International Food Policy Research Institute, Washington DC.
- Garrett, J.L. (2000) Achieving Urban Food and Nutrition Security in the Developing World. Overview: A 2020 Vision for Food, Agriculture and the Environment. International Food Policy Research Institute, Washington DC.
Variable description
1. Percentage below poverty line—for first round NFHS data, percentage of population below poverty line was data of 1983. For second round, poverty estimates are taken from 1993-1994 and for third round it was taken from 1999-2000 estimates. Percentage of population below poverty line for north eastern states has been calculated by
Step 1: to get total number of persons in north-eastern states, multiplying number of population below poverty line of the particular states with the ratio 100/percentage of population below poverty line of that state.
Step 2: {(number of persons below poverty line)*100}/(total number of persons).
2. Inequality adjusted per capita consumption expenditure—GINI adjusted per capita consumption expenditure is taken for period 1983 for studying its impact on stunting of period 1991-1992, similarly 1993-1994 for 1998-1999 and 1999-2000 for studying 2005-2006. NSSO 38th, 50th and 55th round household consumption expenditure has been used to get per capita expenditure. For northeastern states,
First calculated the adjustment factor by dividing all India inequality adjusted per capita consumption expenditure by all India per capita consumption expenditure.
Next, north eastern state specific per capita consumption expenditure was multiplied by population of the respective state of the respective time period (for 1983, census 1981; for 1993-1994 census 1991; and for 2000 census 2001 has been used). Summed the total consumption expenditure of seven states. Then summed population of respective periods of seven states. Then divided total consumption expenditure of seven states by total population of seven states.
Next, per capita consumption expenditure of northeastern states was multiplied by the adjustment factor.
3. PDS coverage—state wise total targeted allocation of food grains per annum in “000” metric tons averaged for the year 1986-1987 to 1995-1996 was used for 1991-1992 and 1998-1999 period. And 2003-2004 data on allocation of food grains per annum in “000” metric ton was used for 2005-2006 period. Amounts allotted for northeastern states for respective periods were calculated by summing up state specific figures.
4. Annual food production—annual food production in a state influence the per capita availability of food inside the household (Rosegrant, 2007). Annual food production data of periods 1990-1991, 1996-1997 and 2003-2004 are used. Amounts for northeastern states have been created by summing up state specific figures.
5. NSDP-Net state Domestic Product data of periods 1990-1991, 1996-1997 and 2003-2004 are used. Amounts for northeastern states have been created by summing up state specific figures.
6. Percentage of population in workforce—it is gathered for years 1983, 1993-1994 and 1999-2000. Percentage for northeastern states is calculated as below:
Northeastern state specific percentage of persons in labor force are multiplied by population of the respective state of the respective time period (for 1983, census 1981; for 1993-1994 census 1991; and for 2000 census 2001 has been used). Summed the total number of persons in the labor force of seven states. Then summed population of respective periods of seven states. Then divided number of persons in the labor force of seven states by total population of seven states.
7. Mother’s nutritional status—as probability of a child to be stunted depends to some extent on mother’s nutritional status; it is taken as one explanatory variable. It is measured by body mass index of mother measured as height/kg2 of the person. State variable is recoded by clubbing together seven northeastern states. Mother’s body mass index is calculated from NFHS 2 and NFHS 3 as data on mother’s BMI is available in these two rounds. For NFHS round 1, data has been extrapolated using other two rounds of data by Stata software version 9.0. Then state specific averages are used for analysis.
8. Maternal education—it influences the knowledge and awareness about child care. So it influences the feeding of the child, its preventive and curative care uptake State specific averages of mother’s years of education are calculated for three rounds.
9. Duration of breastfeeding—as one immediate determinant breastfeeding is taken. Mean duration of breastfeeding is calculated for each state for each period as an indicator of breastfeeding duration in each state.
10. Household’s environment indicators are also Government’s provision of some public goods like drinking water and modern toilet facility, which are treated as community characteristics also (Linnermayr and Alderman, 2008). Under-nutrition reduction through better environment provision improves child’s health status and weakens the vicious circle of malnutrition and morbidity (WHO, 2010).
Safe drinking water—the Department of Drinking water and Sanitation has defined that “Drinking water is water intended for human consumption for drinking and cooking purposes from any source. It includes water supplied by pipes or any other means for human consumption by any supplier”. Drinking water is also defined as water free from different insects. In short, the potable water should not have bacteria or insects and it should not create any harmful effect on human body. In general, those households have access to drinking water from tap, tub well or hand pump situated within or outside the premises, it is considered as having access to safe drinking water.
Drinking water taken from pipes which are coming inside the residence/yard/plot, hand pump in yard or plot, public hand pump are taken as safe, whereas drinking water from well, spring, river, pond, lake, stream, dam, rainwater or any other unsafe source are taken as insecure.
Modern toilet facility—own flush or traditional pit toilet are taken as good whereas deficing in bush or using shared or public toilet are taken as bad toilet.
11. Fully immunized children—full immunization is defined as child has taken one BCG, 3 DPT, 3 Polio and 1 measles within 9 months of age according to Expanded Immunization Programme launched by World Health Organization (WHO, 1974) to protect all children against six vaccine preventable diseases—Diphtheria, Whooping cough, Tetanus, Polio, Tuberculosis and Measles. Expanded Programme on Immunization was launched in India in 1978. It is now known as Universal Child Immunization, Indian version of it was launched in 1985 (WHO, 1978). Expanded Programme on Immunization, Report and working papers, 31st Session of the WHO Reg. Committee, Mongolia, 21-28 Aug, 1978, SEARO). Percentage of children under two year of age who are fully immunized are calculated for every state and state specific averages are taken for analysis.
12. Total number of available hospital beds per “00,000” population is taken from www.Cehat.org for the years 1991, 1996 and 2001.
Northeastern state specific numbers are multiplied by population of the respective state of the respective time period (for 1991, census 1981; for 1996 census 1991; and for 2001 census 2001 has been used). Summed the total number of beds in seven states. Then summed population of respective periods of seven states. Then divided total number of beds in the seven states by total population of seven states.
13. Per capita health expenditure by government of India is taken from www.indiastat.com for the years 1989-1990 and 1999-2000. Values for the interim period are interpolated using Stata version 9.0.
Northeastern state specific values are multiplied by population of the respective state of the respective time period (census 1981; census 1991; and census 2001 has been used). Summed the total health expenditure in seven states. Then summed population of respective periods of seven states. Then divided total health expenditure in the seven states by total population of seven states.
NOTES
1Although chronic under-nutrition is of an irreversible occurrence at the household/individual level, average chronic under-nutrition for regional units like states change over time.
2At macro level, it is the variable which at least gives an idea about how much food grains have been allocated considering the leakage. Due to data limitation on micro level distribution, allocation is an indicative indicator only.
3I also tried with percentage of population having access to modern toilet facility but there is high correlation with mother’s average years of education (0.7072).
4For economy in length, I have only reported the efficient models in the results sections.
5The Hausman specification test offers a statistical comparison between the competing models, RE and FE; it simply tests the difference between FE and RE estimates are significantly different from zero. The Hausman specification test examines if the individual effects are uncorrelated with the other regressors in the model, i.e. it considers the individual effects to be random. Hence, in other words the Hausman test offers to test whether the preferred model is a RE model.
6The Breusch-Pagan Lagrange multiplier (LM) test is designed to test random effects. The null hypothesis of the one-way random group effect model is that individual-specific or time-series error variances are zero; H0 = σ2u = 0. If the null hypothesis is not rejected, the pooled OLS model is appropriate.
7Tests for endogeneity in a regression estimated via instrumental variables (IV), entails the null hypothesis which states that an ordinary least squares (OLS) estimator of the same equation would yield consistent estimates: that is, any endogeneity among the regressors would not have deleterious effects on OLS estimates. A rejection of the null indicates that endogenous regressors’ effects on the estimates are meaningful, and instrumental variables techniques are required. The test was first proposed by Durbin (1954) and separately by Wu (1973) (his T4 statistic) and Hausman (1978). This “Durbin-Wu-Hausman” (DWH) test is numerically equivalent to the standard “Hausman test”. Under the null, it is distributed Chi-squared with m degrees of freedom, where m is the number of regressors specified as endogenous in the original instrumental variables regression. A related test is the Wu-Hausman test. The test statistic, under the null, is distributed F(m, N-k), where m is the number of regressors specified as endogenous in the original instrumental variables regression. A rejection indicates that the instrumental variables estimator should be employed. See Davidson and MacKinnon (1993, pp. 237-240) [35] and Wooldridge (2000, pp. 483-484) [36] .
8Fiorio, C.V. & Jenkins, S.P. (2008) [37] .
9A pseudo standard deviation is (IQR/1.35) which should be equal to the actual standard deviation for a Normal density.
10States are grouped according to the regions as defined in NFHS rounds (IIPS 1994, IIPS 2000, IIPS 2007).







