Advances in Breast Cancer Research
Vol.2 No.2(2013), Article ID:30480,8 pages DOI:10.4236/abcr.2013.22006
Homocysteine as a Biomarker for Predicting Disease-Free Survival in Breast Cancer
1Departamento de Farmacologia, Universidade Federal de São Paulo, São Paulo, Brazil
2Instituto do Câncer do Estado de São Paulo, São Paulo, Brazil
3Disciplina de Imunologia, Universidade Federal de São Paulo, São Paulo, Brazil
4Centro de Referência da Saúde da Mulher, Hospital Pérola Byington, São Paulo, Brazil
5Disciplina de Mastologia, Universidade Federal de São Paulo, São Paulo, Brazil
6Departamento de Psicobiologia, Universidade Federal de São Paulo, São Paulo, Brazil
7Instituto de Educação e Ciência, Hospital Alemão Oswaldo Cruz, São Paulo, Brazil
Email: mjasiulionis@gmail.com
Copyright © 2013 Daniela Filippini Ierardi et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received February 5, 2013; revised March 6, 2013; accepted March 13, 2013
Keywords: Homocysteine; Cysteine; Breast Cancer; Estrogen Receptor; Prognostic and Predictive Biomarker; Tamoxifen; Anastrozol
ABSTRACT
Introduction: Breast cancer is the leading cause of cancer mortality among women. Some biomarkers and clinical features are used for the diagnosis and prognosis of this tumor, but no prognostic or predictive marker is routinely available specifically for hormone receptor positive tumors. Homocysteine is well known as a risk factor in atherosclerotic vascular diseases, but its participation in cancer biology is still unclear. The aim of this study was to evaluate serum Homocysteine and Cysteine as biomarkers of disease progression in breast tumor. As a secondary objective, the effect of a short course (one month) of hormonal treatment on Homocysteine, Cysteine and DNA methylation levels was also evaluated. Methods: Blood samples, tumor samples and normal adjacent tissue were collected during the initial biopsy (pre-treatment) and after one month of hormonal therapy (post-treatment). Serum Homocysteine and Cysteine were analyzed by HPLC and tissue global DNA methylation was determined by the Methylation-Sensitive Restriction Enzyme (MSRE) technique. Results: Variations in Homocysteine levels were significantly correlated with Disease-Free Survival. Cox proportional risk model demonstrated that nodal status and Homocysteine levels were independent prognostic factors for disease-free survival (DFS). A significant difference was observed between preand post-treatment levels of Homocysteine and Cysteine in advanced tumors, suggesting a prognostic role in patients with poor clinical characteristics. Conclusion: Although more studies are needed to confirm these results, our research suggests that Hcy might be used as a prognostic biomarker for breast cancer.
1. Introduction
Breast cancer is the leading cause of cancer death among women worldwide [1]. Clinical and pathological characteristics are still the sources of the most important information used to assess prognosis and define treatment (such as tumor staging, hormonal receptors expression and human epidermal growth factor receptor 2 status) [2].
Estrogen receptor positive (ER+) tumors have a better prognosis than most breast tumors, partly due to their response to hormonal therapies [3,4]. These drugs may modulate the estrogen receptor itself or inhibit estrogen production in post-menopausal women. Although it’s very effective, hormonal therapies cannot prevent relapse in about 30% of patients with estrogen receptor positive breast tumors, and no prognostic or predictive marker of response is routinely available for this group of patients [5].
Homocysteine (Hcy) is an extensively studied prognostic marker in atherosclerotic vascular diseases [6], but its contribution to cancer biology is still unclear. Alterations of homocysteine levels may cause an imbalance among the products of the anti-oxidative pathway resulting in increased oxidative metabolism [7]. Homocysteine synthesis is also related indirectly to DNA methylation, a mechanism for gene expression control in normal and tumor cells [8-10].
This work evaluates blood levels of homocysteine and its metabolite cysteine as biomarkers of survival and disease progression in post-menopausal women with non-metastatic breast cancer. We also studied the effect of a short-course of pre-operative (neoadjuvant) endocrine therapy on Homocysteine and Cysteine metabolism in a subgroup of these patients.
2. Patients and Methods
2.1. Patients
Ninety-seven post-menopausal breast cancer patients from two different institutions (Hospital São Paulo and Hospital Pérola Byington in São Paulo-Brazil) were evaluated. Sixty-seven of those patients participated in a randomized study of one month neoadjuvant endocrine therapy (tamoxifen or anastrozol) versus placebo.
The present study was approved by both Universidade Federal de São Paulo and Pérola Byington Hospital Institutional Review Boards, and all patients provided written informed consent. All patients were submitted to a diagnostic biopsy, and only patients with invasive breast carcinomas were included. Tumor samples were also obtained during definitive surgery for the removal of tumor tissue, for those patients participating in the randomized study. Serum and plasma were collected from all patients at the time of the initial biopsy (pre-treatment) and at the day of surgery (post-treatment) for patients in the randomized study.
For experimental purposes, clinical and pathological data were obtained from patients’ medical records. Observed clinical parameters were tumor size (T), lymph node positivity (N0, negative lymph node and N1; positive lymph node), clinical Stage (CS, initial stages = I and II; late stages = III), local relapse, distant relapse, date of last event (relapse, death or last visit) and cause of death. Initial tumor size was defined by clinical examination or ultrasound, whichever was greater. Final tumor size was defined by pathological gross examination.
Immunohistochemical characteristics such as estrogen receptor and progesterone receptor status were also recorded.
2.2. Serum Homocysteine and Cysteine Quantification
The total serum Hcy (tHcy) and Cys (tCys) levels were measured according to the method described by Pfeiffer and co-authors [11]. Positive and negative ΔHcy (or ΔCys) were defined as the difference in post-treatment tHcy (or tCys) minus pre-treatment tHcy (or tCys) levels.
2.3. Analysis of Tumor DNA Methylation Levels
One microgram of DNA extracted from tumor sample or adjacent tissue was digested with either MspI or HpaII restriction enzymes (Fermentas, St. Leon-Rot, Germany). Non-digested DNA, and MspI and HpaII digested DNA were visualized in 0.8% agarose gel. Observed bands were quantified with ImageJ and methylation ratio was calculated subtracting HpaII digested DNA quantification from the MspI quantification, divided by nondigested DNA quantification (HpaII-MspI/non-digested DNA).
2.4. Statistical Analysis
Kruskal-Wallis test was used to compare Hcy, Cys and pathological tumor size values, and these variables were correlated using Spearman correlation test when adequate [12].
Disease-free survival (DFS) was calculated from the date of diagnosis until date of first relapse or death, and presented using the Kaplan-Meyer method [13]. Followup was measured from date of diagnosis to the date of last visit or date of death. Survival curves were compared using Log-rank test or Breslow test when curve intersection was observed. Univariate and multivariate analysis were performed by Cox regression method.
Multivariate analyses tested all variables found in the univariate analysis with a p-value lower than 0.05, and excluded patients with one or more missing data. All statistical tests were two-sided, and the level of significance was set at 5%. Analyses were done using the Statistical Package for Social Science SPSS (release 15.0, Chicago, Illinois, USA). The analysis adhered to the reporting recommendations for tumor marker prognostic studies.
3. Results
3.1. Clinical Data and Biochemical Quantifications
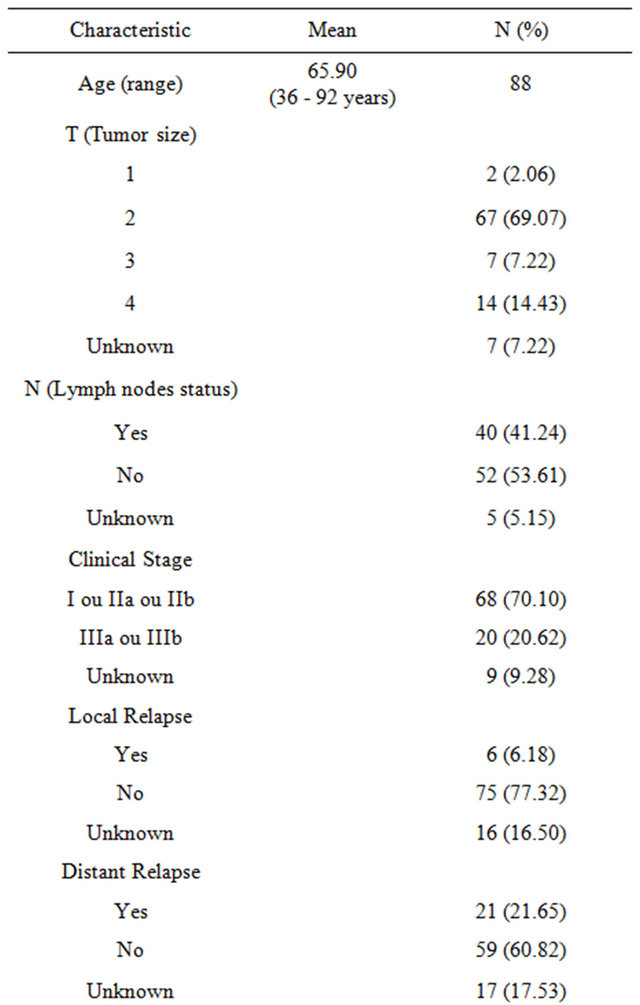
Patients’ characteristics are listed in Table 1. Of 67 patients participating in the randomized trial, one was excluded because she received neoadjuvant (pre-operative) chemotherapy.
Homocysteine (Hcy) and cysteine (Cys) levels were measured at the time of the initial biopsy in all patients (entire group). Patients that did not participate in the trial received therapy according to the discretion of their physicians, and had no Hcy or Cys measured after the biopsy.
Table 1. Patients’ clinical characteristics.
Patients participating in the randomized trial (trial group) had Hcy and Cys measured again at the time of the surgery.
There were no statistical differences in basic characteristics , as well as type of post-operative treatment, between those patients in the randomized trial and those not participating in the trial, and among groups in the randomized trial (data not shown). Because there were no statistical differences between groups, we treated the data as belonging to the same group.
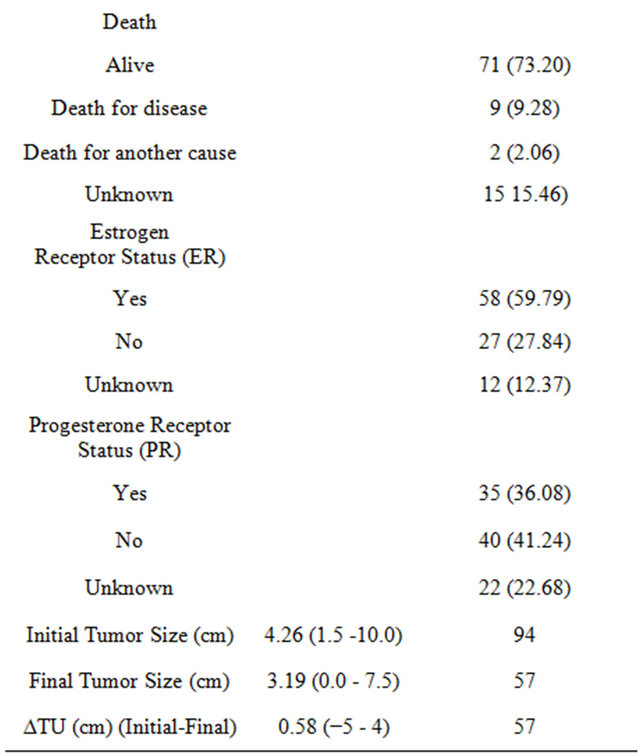
The entire group had biochemical characteristics measured at the time of the initial biopsy, but variations (∆) were calculate only for trial patients, which had samples collected both at the time of the initial biopsy and at the time of surgery. Results are shown in Table 2.
Homocysteine and Cyste ine l evels, both initial and at surgery, and their variations (∆) were weak or moderately correlated between themselves (r = 0.579, r = 0.756 and r = 0.621, respectively, with p < 0.001 for all tests). Initial Cysteine levels were weakly and inversely correlated with initial global DNA methylation levels (r = −0.366, p = 0.028). These results are expected in light of the metabolic relationships among Homocysteine, Cysteine and DNA methylation in the methionine cycle [10].
3.2. Variations in Serum Hcy and Cys Levels Correlate with Late Clinical Stages
Figure 1 shows that, for patients with advanced disease (Stage III) or with positive lymph nodes (Figures 1(c) and (d) respectively), Cysteine levels decreased after use of
Table 2. Biochemical characteristics.
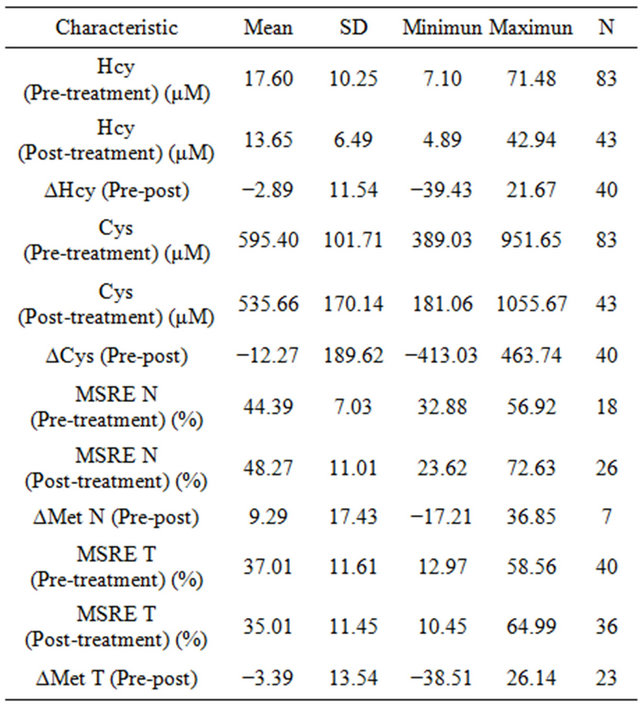
anastrozol, tamoxifen or placebo (trial group). Homocysteine levels decreased significantly in patients with advanced disease (Figure 1(a)), but not with statistical significance in patients with positive lymph nodes (Figure 1(b)).
There was no significant statistical correlation regarding Hcy or Cys levels variations and tumor size (data not shown). Interestingly, one patient in the anastrozole group presented a residual tumor with less than 1 mm of size, and other showed no residual tumor after surgery. In the tamoxifen group, one patient as well had no detectable tumor mass after surgery.
Hcy is a crucial component of the methionine cycle, which is linked to DNA methylation [10]. We quantified global DNA methylation levels in patients in the trial group, both at the initial biopsy and at the time of the definitive surgery, in normal and tumor samples. Although global DNA methylation levels were decreased in tumor compared to normal samples as expected [14], no significant correlation was found comparing global DNA methylation levels with initial clinical characteristics (data not shown). Variations in Homocysteine (∆Hcy) showed a statistically non-significant weak to moderate correlation with variations in tumor global DNA methylation levels (∆Met T) (r = 0.432, p = 0.057).
3.3. Hcy and Cys Levels Did Not Vary Significantly after a Short Term of Neoadjuvant Antiestrogens
Regarding the initial biopsy, we found no significant statistical differences between serum levels of Hcy (r = −0.013; p = 0.938), or Cys (r = −0.069; p = 0.672), and
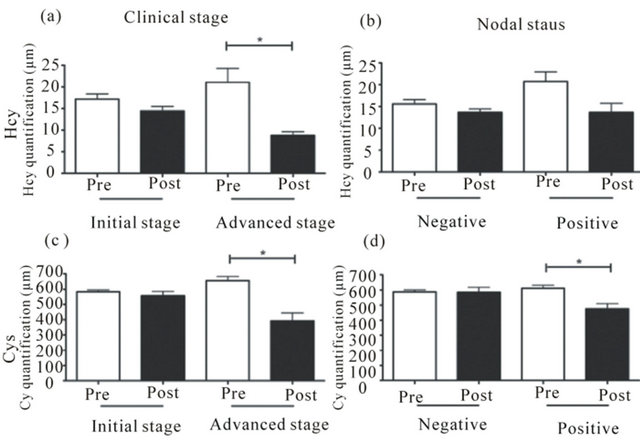
Figure 1. Homocysteine and cysteine levels after hormonal treatment present a larger decrease in patients with advanced clinical stage. Hcy and Cys levels before (pre) and after treatment (post) in initial or advanced clinical stage (a) and (c), respectively, and negative or positive nodal status (b) and (d), respectively. *p < 0.05.
DNA methylation for normal and tumor tissue (r = −0.214; p = 0.645 and r = 0.405; p = 0.62) for the entire group or the trial group.
We also did not find any significant statistical correlation between Hcy and Cys variations (∆Hcy and ∆Cys) and the use of antiestrogens or placebo on a multivariate analysis (data not shown).
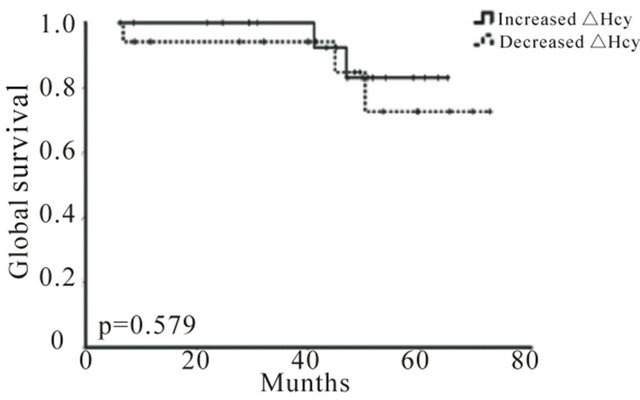
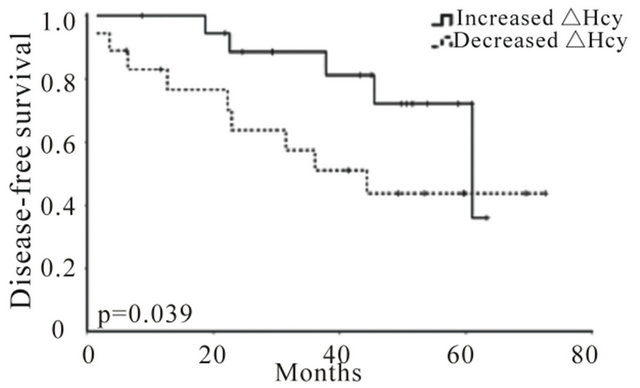
3.4. High Serum Hcy Variation Predicts Better Disease-Free Survival
Global survival was not significantly correlated with any clinical (data not shown) or isolated biochemical parameters, including Hcy or Cys (Figure 2), probably because of a low number of events. However, variations in Hcy levels (∆Hcy), but not in Cys (∆Cys), were significantly correlated with disease-free survival (DFS), and patients with an increase in Hcy levels after treatment (positive ΔHcy) present a higher probability of surviving with no evidence of relapse (Figure 3). Cox proportional risk model, including clinical stage, nodal status and Hcy variation (∆Hcy), demonstrated that nodal status (HR = 2.86; 95% CI = 1.16 − 12.79; p = 0.027) and Hcy variation (∆Hcy, HR = 0.96; 95% CI = 0.92 − 0.998; p = 0.042) are independent prognostic factors regarding DFS.
 (a)
(a)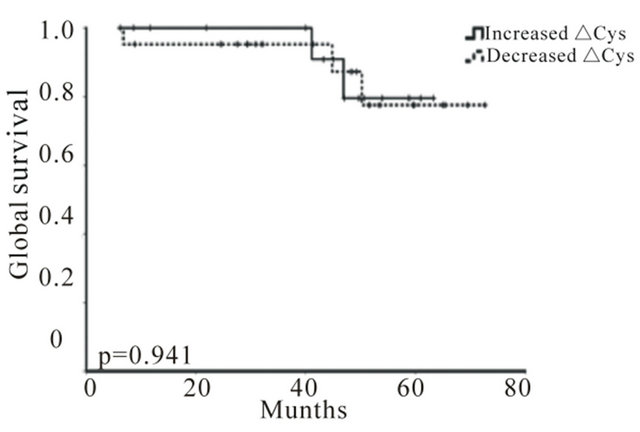 (b)
(b)
Figure 2. Hcy and Cys variations do not correlate with overall survival (OS) in breast cancer. Kaplan-Meier OS curves for increased and decreased ∆Hcy (a) and ∆Cys (b) (p = 0.579 and p = 0.941, respectively) + indicates event.
4. Discussion
We found a significant inverse correlation between increased Homocysteine levels, and disease-free survival (Figure 3(a)). We also encountered significant positive correlations between variations in Hcy and Cys in trial patients with advanced disease or positive lymph nodes (Figure 1), suggesting that Homocysteine levels in these patients may be correlated with response to hormonal treatment. These findings seem contradictory unless we consider that patients with bulky disease, who may have a more noticeable response to antihormonal therapy and therefore a higher variation in Hcy and Cys levels, are also the ones with a much higher chance of relapse. We also postulate that Hcy levels are inversely related to tumor response to antiestrogens, but the low number of patients in this sample did not allow our analyses to support this hypothesis. There are many limitations in this study, including the number of subjects and their heterogeneity, and we approach all findings as hipothesis generating only.
Increased Homocysteine levels have long been studied as a risk factor for cardiovascular disease, and more recently for some neurological problems and pregnancy complications [15]. Plasma Hcy quantification is a relatively simple and fast procedure, and there is some evidence showing Hcy contribution in carcinogenesis [16]
 (a)
(a)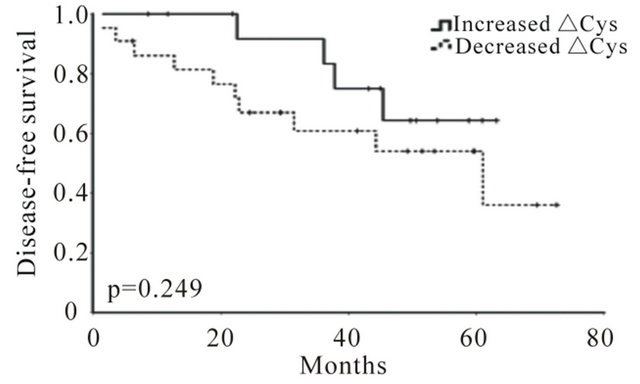 (b)
(b)
Figure 3. Hcy level variations correlate with disease-free survival (DFS) in breast cancer. Kaplan-Meier DFS curves for increased and decreased ∆Hcy (a) and ∆Cys (b). (*p = 0.039 and p = 0.249, respectively) + indicates event.
and as a risk factor for breast cancer [17]. Few cheap and practical biochemical biomarkers are routinely available to predict prognosis or response to cancer treatment and, in this context, Hcy might be a useful prognostic and/or predictive biomarker.
Breast cancer is a very common type of cancer, and has been studied extensively. Although several biomarkers are described in the literature [18-20], there are many efforts to increase the biomarker list and to personalize cancer diagnosis and treatment. However, most of these efforts look at molecular profiles and depend on molecular genetics facilities or tissue sampling processing, which are expensive and not largely available.
Hcy metabolism can be disrupted by defects in transulfuration or remethylation pathways, which may cause increases in Hcy levels. The accumulation of Hcy levels can result in Cys levels augmentation [17,21]. As expected, our results show a correlation between Hcy and Cys levels, both before and after antiestrogens therapy. A correlation between Hcy and Cys variations (∆Hcy/ΔCys) was also observed.
DNA methylation is a well-studied epigenetic mechanism involved in gene expression control [9]. The imbalance in Hcy levels may result in changes in Sadenosylmethionine (SAM) levels and consequently promote alterations in DNA methylation patterns [8].
Soares and co-authors [22] already demonstrated the importance of hypomethylation as an epigenetic event involved in the breast tumorigenesis. Although we did not observe any correlation among tumor size and global methylation levels in tumor tissues, we observed an inverse correlation between Hcy variation (∆Hcy) and tumor sample methylation variation (∆Met T), although not statistically significant (data not shown). These parameters may be influenced by several modifying factors such as diet, DNA polymorphisms of the enzymes involved in the methionine metabolism and, even more critical in our study, the interference of two different drugs, tamoxifen and anastrozol [23,24].
We also correlated Hcy and Cys levels variations with clinical-pathological features of breast tumors, as nodal status (N) and clinical stage (CS). Our results show a significant reduction of the Hcy and Cys levels after antiestrogens or placebo in patients with poor clinical characteristics (Figures 1(a), (c) and (d)). Although we could not find a statistically significant difference for nodal status and Hcy levels (Figure 1(c)), we did observe the same biological pattern (reduction of Hcy levels in node positive patients). A study with untreated patients suffering from primary head and neck squamous cell carcinoma (HNSCC) was not able to find any correlation between folate, B12 vitamin and Hcy serum levels and disease progression [25], suggesting that the difference between Hcy and Cys levels and progression may be specific for different tumor types.
At this moment, few data are available regarding Hcy role in tumor biology. Some efforts have been done to evaluate the relationship between Hcy and Cys levels with the risk of developing breast tumors. Some studies observed that an increased breast cancer risk was associated with high levels of Hcy or Cys in women with low levels of folate [17,21,26]. In addition, high plasma or serum levels of Hcy were also observed in patients with other cancer types [16,27-31].
Although most authors analyzed Hcy levels and other methionine cycle components as factors for developing cancer, only a few studies discussed the possible role of Hcy as a prognostic factor. Bobe and co-workes [28] found that high Hcy concentrations were associated with colorectal adenoma recurrence. No studies could be found correlating Hcy and breast cancer prognosis. We also studied the relationship of Hcy and/or Cys concentration with global methylation levels, in order to search for possible biological mechanisms underlying this association, but we were not able to find any correlation at this time.
To check the possibility that the Hcy and/or Cys present prognostic or predictive value, we evaluated patients with resectable breast tumors, followed for a period of four to seven years. Due to a small number of fatal events, the study lacked power to determine the contribution of the Hcy and Cys as prognostic factors in overall survival (OS). Nevertheless, our results show that an increase in Hcy levels after a short course of neoadjuvant therapy is significantly correlated with a longer disease-free survival (DFS) (Figure 3), suggesting that the variation of Hcy is a possible prognostic marker for breast tumor. Interestingly, advanced tumors presented a decrease in Hcy after antiestrogens treatment (Figures 1(a) and (d)), confirming an association between Hcy and prognosis in breast tumors. A multivariate analysis showed that Hcy levels and nodal status (N), but not tumor size, are independent prognostic factors regarding DFS, implying that the variation in Hcy levels can be useful as an additional marker in the prediction of treatment response in breast tumor patients.
The short-term course of tamoxifen or anastrozol had little influence on overall survival (OS) or disease free survival (DFS) (data not shown). A study from Washington University [32] showed that the use of 4 months of either tamoxifen or letrozol (another aromatase inhibitor, comparable to anastrozol) had no impact on relapse-free survival or specific breast cancer survival. A meta-analysis of 4 studies [33] comparing anastrozol to tamoxifen as neoadjuvant therapy detected a superiority of anastrozol regarding the rate of breast-conserving surgery, which could not be found in our study probably because of the small number of subjects, and the short period of treatment.
High Hcy level is a well-known cardiovascular risk factor and Hcy levels have also been suggested as a potential tumor marker [16]. At least in our knowledge, no report has been published about the value of the Hcy levels variation as a predictive or prognostic marker for breast cancer. We are well aware of the limitations of this study (retrospective analysis of a heterogeneous group of patients), but we have shown for the first time the potential of Hcy levels variation as a disease-free survival (DFS) marker in breast tumor patients. This finding is hypothesis generating, and will be further characterized in the near future by our group.
5. Acknowledgements
The authors thank Dr. Andre Mattar for providing patient samples, Pérola Byington Clinical Research Department and São Paulo Hospital Serviço de Arquivo Médico e Estatística for patients’ clinical data. The authors would like to thank Universidade Federal de São Paulo, Fundação de Amparo à Pesquisa do Estado de São Paulo (2011/12306-1, to M.G.J.; 2008/56564-1, to C.S.P.; 2010/ 04585-5, to G. Aguiar; 2010/00245-5 to B.F.A.C), Conselho Nacional de Desenvolvimento Científico e Tecnológico (151578/2009-5, to D.F.I.; Research felowship 306485/2008-7 to M.G.J. and to 301742/2010-3 V.D’A.) and Coordenação de Aperfeiçoamento Pessoal de Nível Superior-CAPES (2745/2010, to D.F.I.).
REFERENCES
- T. S. Foster, J. D. Miller, M. E. Boye, M. B. Blieden, R. Gidwani and M. W. Russell, “The Economic Burden of Metastatic Breast Cancer: A Systematic Review of Literature from Developed Countries,” Cancer Treatment Reviews, Vol. 37, No. 6, 2011, pp. 405-415.
- B. Metzger, L. Chambeau, D. Y. Begon, C. Faber, J. Kayser, G. Berchem, M. Pauly, J. Boniver, P. Delvenne, M. Dicato and T. Wenner, “The Human Epidermal Growth Factor Receptor (EGFR) Gene in European Patients with Advanced Colorectal Cancer Harbors Infrequent Mutations in Its Tyrosine Kinase Domain,” BMC Medical Genetics, Vol. 12, No. 1, 2011, p. 144. doi:10.1186/1471-2350-12-144
- S. R. Johnston, “New Strategies in Estrogen ReceptorPositive Breast Cancer,” Clinical Cancer Research, Vol. 16, No. 7, 2010, pp. 1979-1987. doi:10.1158/1078-0432.CCR-09-1823
- Early Breast Cancer Trialists Collaborative Group, “Tamoxifen for Early Breast Cancer: An Overview of the Randomised Trials. Early Breast Cancer Trialists’ Collaborative Group,” Lancet, Vol. 351, No. 9114, 1998, pp. 1451-1467. doi:10.1016/S0140-6736(97)11423-4
- I. H. Abdulkareem and I. B. Zurmi, “Review of Hormonal Treatment of Breast Cancer,” Nigerian Journal of Clinical Practice, Vol. 15, No. 1, 2012, pp. 9-14. doi:10.4103/1119-3077.94088
- K. Miyaki, “Genetic Polymorphisms in Homocysteine Metabolism and Response to Folate Intake: A Comprehensive Strategy to Elucidate Useful Genetic Information,” Journal of Epidemiology, Vol. 20, No. 4, 2010, pp. 266-270. doi:10.2188/jea.JE20100042
- B. T. Zhu, “On the Mechanism of Homocysteine Pathophysiology and Pathogenesis: A Unifying Hypothesis,” Histology and Histopathology, Vol. 17, No. 4, 2002, pp. 1283-1291.
- P. Yi, S. Melnyk, M. Pogribna, I. P. Pogribny, R. J. Hine and S. J. James, “Increase in Plasma Homocysteine Associated with Parallel Increases in Plasma S-Adenosylhomocysteine and Lymphocyte DNA Hypomethylation,” The Journal of Biological Chemistry, Vol. 275, No. 38, 2000, pp. 29318-29223. doi:10.1074/jbc.M002725200
- M. Esteller and G. Almouzni, “How Epigenetics Integrates Nuclear Functions. Workshop on Epigenetics and Chromatin: Transcriptional Regulation and Beyond,” EMBO Reports, Vol. 6, No. 7, 2005, pp. 624-628. doi:10.1038/sj.embor.7400456
- P. Sharma, R. D. Senthilkumar, V. Brahmachari, E. Sundaramoorthy, A. Mahajan, A. Sharma and S. Sengupta, “Mining Literature for a Comprehensive Pathway Analysis: A Case Study for Retrieval of Homocysteine Related Genes for Genetic and Epigenetic Studies,” Lipids in Health and Disease, Vol. 5, No. 1, 2006, p. 1. doi:10.1186/1476-511X-5-1
- C. M. Pfeiffer, D. L. Huff and E. W. Gunter, “Rapid and Accurate HPLC Assay for Plasma Total Homocysteine and Cysteine in a Clinical Laboratory Setting,” Clinical Chemistry, Vol. 45, No. 2, 1999, pp. 290-292.
- B. R. Kirkwood and J. A. C. Sterne, “Essential Medical Statistic,” Blackwell Publishing Limited, Oxford, 2006.
- D. G. Kleinbaum and M. Klein, “Statistics for Biology and Health. Survival Analysis, Series: Statistics for Biology and Health,” Springer, New York, 2005.
- M. Hatziapostolou and D. Iliopoulos, “Epigenetic Aberrations during Oncogenesis,” Cellular and Molecular Life Sciences, Vol. 68, No. 10, 2011, pp. 1681-1702. doi:10.1007/s00018-010-0624-z
- E. Lonn, S. Yusuf, M. J. Arnold, P. Sheridan, J. Pogue, M. Micks, M. J. McQueen, J. Probstfield, G. Fodor, C. Held and J. Genest Jr., “Homocysteine Lowering with Folic Acid and B Vitamins in Vascular Disease,” The New England Journal of Medicine, Vol. 354, No. 15, 2006, pp. 1567-1577. doi:10.1056/NEJMoa060900
- L. L. Wu and J. T. Wu, “Hyperhomocysteinemia Is a Risk Factor for Cancer and a New Potential Tumor Marker,” Clinica Chimica Acta, Vol. 322, No. 1-2, 2002, pp. 21-28. doi:10.1016/S0009-8981(02)00174-2
- J. Lin, I. M. Lee, Y. Song, N. R. Cook, J. Selhub, J. E. Manson, J. E. Buring and S. M. Zhang, “Plasma Homocysteine and Cysteine and Risk of Breast Cancer in Women,” Cancer Research, Vol. 70, No. 6, 2010, 2010, pp. 2397-2405.
- M. Brooks, “Breast Cancer Screening and Biomarkers,” Methods in Molecular Biology, Vol. 472, 2009, pp. 307- 321. doi:10.1007/978-1-60327-492-0_13
- T. Wright and A. McGechan, “Breast Cancer: New Technologies for Risk Assessment and Diagnosis,” Journal of Molecular Diagnostics, Vol. 7, No. 1, 2003, pp. 49-55.
- C. L. Corless, “Medicine. Personalized cancer diagnostics,” Science, Vol. 334, No. 6060, 2011, pp. 1217-1218. doi:10.1126/science.1216427
- M. H. Stipanuk, J. E. Dominy Jr., J. I. Lee and R. M. Coloso, “Mammalian Cysteine Metabolism: New Insights into Regulation of Cysteine Metabolism,” Journal of Nutrition, Vol. 136, Suppl. 6, 2006, pp. 1652S-1659S.
- J. Soares, A. E. Pinto, C. V. Cunha, S. Andre, I. Barao, J. M. Sousa and M. Cravo, “Global DNA Hypomethylation in Breast Carcinoma: Correlation with Prognostic Factors and Tumor Progression,” Cancer, Vol. 85, No. 1, 1999, pp. 112-118. doi:10.1002/(SICI)1097-0142(19990101)85:1<112::AID-CNCR16>3.0.CO;2-T
- G. Anker, P. E. Lonning, P. M. Ueland, H. Refsum and E. A. Lien, “Plasma Levels of the Atherogenic Amino Acid Homocysteine in Post-Menopausal Women with Breast Cancer Treated with Tamoxifen,” International Journal of Cancer, Vol. 60, No. 3, 1995, pp. 365-368. doi:10.1002/ijc.2910600316
- M. Cattaneo, L. Baglietto, M. L. Zighetti, D. Bettega, C. Robertson, A. Costa, P. M. Mannucci and A. Decensi, “Tamoxifen Reduces Plasma Homocysteine Levels in Healthy Women,” British Journal of Cancer, Vol. 77, 1998, pp. 2264-2266. doi:10.1038/bjc.1998.376
- G. Almadori, F. Bussu, J. Galli, G. Cadoni, B. Zappacosta, S. Persichilli, A. Minucci, B. Giardina and M. Maurizi, “Serum Levels of Folate, Homocysteine, and Vitamin B12 in Head and Neck Squamous Cell Carcinoma and in Laryngeal Leukoplakia,” Cancer, Vol. 103, No. 2, 2005, pp. 284-292. doi:10.1002/cncr.20772
- Y. C. Chou, M. S. Lee, M. H. Wu, H. L. Shih, T. Yang, C. P. Yu, J. C. Yu and C. A. Sun, “Plasma Homocysteine as a Metabolic Risk Factor for Breast Cancer: Findings from a Case-Control Study in Taiwan,” Breast Cancer Research and Treatment, Vol. 101, No. 2, 2007, pp. 199- 205. doi:10.1007/s10549-006-9278-9
- F. L. Sciacca, E. Ciusani, A. Silvani, E. Corsini, S. Frigerio, S. Pogliani, E. Parati, D. Croci, A. Boiardi and A. Salmaggi, “Genetic and Plasma Markers of Venous Thromboembolism in Patients with High Grade Glioma,” Clinical Cancer Research, Vol. 10, No. 4, 2004, pp. 1312- 1317. doi:10.1158/1078-0432.CCR-03-0198
- G. Bobe, G. Murphy, C. J. Rogers, K. W. Hance, P. S. Albert, A. O. Laiyemo, L. B. Sansbury, E. Lanza, A. Schatzkin and A. J. Cross, “Serum Adiponectin, Leptin, C-Peptide, Homocysteine, and Colorectal Adenoma Recurrence in the Polyp Prevention Trial,” Cancer Epidemiology, Biomarkers & Prevention, Vol. 19, No. 6, 2010, pp. 1441- 1452. doi:10.1158/1055-9965.EPI-09-1082
- G. Almadori, F. Bussu, J. Galli, G. Cadoni, B. Zappacosta, S. Persichilli, A. Minucci and B. Giardina, “Serum Folate and Homocysteine Levels in Head and Neck Squamous Cell Carcinoma,” Cancer, Vol. 94, No. 4, 2002, pp. 1006- 1011. doi:10.1002/cncr.10343
- Y. Ozkan, S. Yardim-Akaydin, H. Firat, E. Caliskan-Can, S. Ardic and B. Simsek, “Usefulness of Homocysteine as a Cancer Marker: Total Thiol Compounds and Folate Levels in Untreated Lung Cancer Patients,” Anticancer Research, Vol. 27, No. 2, 2007, pp. 1185-1189.
- K. Schroecksnadel, B. Frick, C. Winkler, L. C. Fuith and D. Fuchs, “Relationship between Homocysteine and Neopterin Concentrations in Patients with Gynecological Cancer,” Cancer Letters, Vol. 240, No. 2, 2006, pp. 198-202. doi:10.1016/j.canlet.2005.09.009
- M. J. Ellis, Y. Tao, J. Luo, R. A’Hern, D. B. Evans, A. S. Bhatnagar, H. A. Chaudri Ross, A. von Kameke, W. R. Miller, I. Smith, W. Eiermann and M. Dowsett, “Outcome Prediction for Estrogen Receptor-Positive Breast Cancer Based on Postneoadjuvant Endocrine Therapy Tumor Characteristics,” Journal of the National Cancer Institute, Vol. 100, No. 19, 2008, pp. 1380-1388. doi:10.1093/jnci/djn309
- J. H. Seo, Y. H. Kim and J. S. Kim, “Meta-Analysis of Pre-Operative Aromatase Inhibitor versus Tamoxifen in Postmenopausal Woman with Hormone Receptor-Breast Cancer,” Cancer Chemotherapy and Pharmacology, Vol. 63, No. 2, 2009, pp. 261-266. doi:10.1007/s00280-008-0735-5

