Advances in Microbiology
Vol.08 No.10(2018), Article ID:87827,14 pages
10.4236/aim.2018.810052
Evaluation of the Antimicrobial Effect of Nepeta cataria and Basella alba against Clinically Resistant Acinetobacter baumannii in Nairobi, Kenya
Salome Marlene Morombaye1, Mourine Kangogo2, Gunturu Revathi3, Andrew Nyerere2, John Ochora4
1Institute of Basic Sciences, Technology and Innovation, Pan African University, Nairobi, Kenya
2Department of Medical Microbiology, Jomo Kenyatta University of Agriculture and Technology, Nairobi, Kenya
3Department of Pathology, Aga Khan University Hospital, Nairobi, Kenya
4Department of Botany, Jomo Kenyatta University of Agriculture and Technology, Nairobi, Kenya

Copyright © 2018 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY 4.0).
http://creativecommons.org/licenses/by/4.0/



Received: August 24, 2018; Accepted: October 15, 2018; Published: October 18, 2018
ABSTRACT
Acinetobacter baumannii is among the common nosocomial infections microorganisms in the Intensive Care Unit (ICU). Antimicrobial resistance (AMR) is one of the major significant concerns in developing nations due to either over-use or inadequate use of antimicrobial agents. The purpose of this study was to emphasize the potential antimicrobial activity of Nepeta cataria and Basella alba against nosocomial diseases caused by Acinetobacter baumannii. Nepeta cataria and Basella alba leaves were collected from Oldonyo Sabuk National Park and Botanical garden JKUAT respectively. The leaves were dried under shade at room temperature for thirty days. After methanolic and aqueous plant extraction, the percentage yield was determined, and the extracts were subjected to toxicity testing using brine shrimp eggs and preliminary phytochemical screening. The results recorded from this study demonstrated that 70% methanolic extract of Nepeta cataria and Basella alba had greater antimicrobial effect against Acinetobacter baumannii than aqueous extracts. Nepeta cataria extracts showed greater antimicrobial effect than Basella alba extracts. The methanolic plant extracts had MIC values 60 mg/ml when tested against Acinetobacter baumannii. The phytochemical screening showed the presence of various phytochemical constituents from the methanolic and aqueous extraction of Nepeta cataria and Basella alba. The methanolic plant extracts revealed more phytochemicals as compared to aqueous extracts. More phytochemicals were detected from Nepeta cataria than Basella alba plant extracts.
Keywords:
Medicinal Plants, Nepeta cataria, Basella alba, Antimicrobial Activity, Acinetobacter baumannii, Phytochemical Screening, Toxicity

1. Introduction
Acinetobacter species, ubiquitous Gram-negative coccobacilli, are widespread in nature, water and soil. More than 20 species of Acinetobacter have been characterized but only few species including Acinetobacter baumannii, A. calcoaceticus and A. lwoffii play a significant role in nosocomial infections [1] . Traditional medicinal plants are likely to provide new antibiotics in future [2] . Numerous works have been done to isolate and characterize bioactive compounds from plant resources that are active against Gram-positive and Gram-negative bacteria, fungi and viruses. A previous study reported that flavonoids, tannins and phenolic compounds are active against Acinetobacter [3] . In recent decades, the pharmacological properties of numerous medicinal plants and opportunities in phytotherapy have been explored through research projects, reviews, and monographs. These studies confirm that medicinal plants offer new approaches to tackling diseases [4] [5] [6] . Plant products derived from barks, leaves, flowers, roots, fruits or seeds have been part of phytomedicines from ancient days and they are also the source of most natural and synthetic drugs [7] .
Before 2008, A. baumannii was uncommon among pathogens recovered at Aga Khan University Hospital, Kenya, and it had remained susceptible to several antibiotics including extended-spectrum cephalosporins, carbapenems, and aminoglycosides [8] . Acinetobacter baumannii infections can be enhanced by the occurrence of multiple antimicrobial resistance, resulting in difficulties when determining the therapeutic options to treat the infection. Plant-based drugs have gained popularity due to their fewer side effects, better patient tolerance, and are relatively less expensive than synthetic drugs. They are more accepted due to a long history of use.
Carbapenem-resistant Acinetobacter baumannii is based on the incidence of multidrug-resistant. A. baumannii has become an emerging pathogen in intensive care units (ICUs) because it has developed resistance to broad-spectrum antibiotics such as carbapenems which were a short time ago the only effective group of antibiotics against multidrug-resistant A. baumannii (MDRAB) infections [9] . The overall prevalence of nosocomial infections in hospital intensive care units due to Acinetobacter baumannii varies from 2% to 10% [10] . Plant-based drugs have gained popularity due to their fewer side effects, better patient tolerance, and relatively less expense than synthetic drugs and are therefore more accepted due to a long history of use. Plants are also the source of most natural and synthetic drugs. Biomolecules of plant origin can serve as alternatives for the control of resistant human pathogens. For instance, Nepata species (Labiateae) are used in traditional medicine in many countries and have large ethnobotanical effects with diuretic, diaphoretic, vulnerary, antitussive, antispasmodic, antiasthmatic, tonic, febrifuge, emmenagogue and carminative properties. It is used as a household herbal remedy, being employed especially in treating disorders of the digestive system, and stimulates sweating, thus reducing fever [11] . Basella alba is an important medicinal plant in ethnoveterinary for treatment of retained afterbirth and anaplasmosis. It is administered in gonorrhea and balanitis. The mucilaginous liquid obtained from the leaves and tender stalks of this plant is a popular remedy for habitual headaches. A decoction of the leaves is a good laxative for pregnant women and children [12] .
2. Materials and Methods
2.1. Collection and Preparation of Plants
The Nepeta cataria leaves were harvested from Ol Donyo Sabuk National Park near Thika town, Kenya in February 2018. The town is in Kyanzavi Division, Machakos County. Basella alba leaves were harvested at Botanical Garden within Jomo Kenyatta University of Agriculture and Technology (JKUAT). The two plant materials were authenticated by the Department of Botany in JKUAT. The leaves were dried under shade at room temperature for 30 days. Crude extraction was done at PAUSTI Molecular Biology and Biotechnology Laboratory located inside Jomo Kenyatta University of Agriculture and Technology.
2.2. Methanolic Extraction
Methanolic extraction of powdered leaves was done according to previous protocol [13] . One hundred and fifty grams (150 g) of the dried plant material was mixed with 750 ml of 70 % methanol at a ratio of 1:5 (w/v) in a flask and shaken vigorously. The plant material was soaked in 70% methanol for 72 hours to allow extraction to take place. The mixture was filtered using Whatman No.1 filter paper. The extracts were concentrated using vacuum rotary evaporator at 50˚C for 3 hours (Labtech EV311, DIAHANLABTECH CO., LTD) then frozen at −80˚C until lyophilization (FDL mr c). The final extracts obtained were weighed to obtain the percentage yield then stored at 4˚C in the refrigerator for further analysis.
2.3. Aqueous Extraction
The powdered plant material was prepared according to [14] protocol. 150 g of the powdered leaves were stirred for five minutes into 750 ml of boiled distilled water which has been cooled to 55˚C at a ratio of 1:5 (w/v) in a flask. The mixture was kept off the hot plate, for 30 minutes to allow it to infuse. The mixture was cooled and filtered using Whatman No.1 filter paper as described by [15] . The mixture was frozen and dried using a freeze dryer machine (FDL mr c). The obtained extracts were weighed; the percentage yield was determined and then stored at 4˚C.
2.4. Phytochemical Screening
Primary screening of the crude extract for the following phytochemicals was done according to the standard protocols described by [16] .
2.4.1. Test for Tannins
About 0.5 g of each plant methanolic extract was boiled in 20 ml of water in their respective test tubes and then filtered. A few drops of 0.1% ferric chloride was added to each test tube. A brownish green or blue-black coloration indicated the presence of tannins.
2.4.2. Test for Phlobatannins
An aqueous extract of each plant sample was boiled with 1% aqueous hydrochloric acid. A deposition of a red precipitate indicated the presence of Phlobatannins.
2.4.3. Test for Saponins
About 50 g of powdered plant extract was dissolved in 400 ml of distilled water in a conical flask and boiled for 5 min. The mixture was filtered when still hot and 5 ml of sterile distilled water added to a test tube containing equal amounts of cooled filtrate. The test tube was shaken vigorously for 30 seconds and then allowed to stand for 30 min. Formation of honey comb froth indicated the presence of saponins.
2.4.4. Test for Flavonoids
5 ml of dilute ammonia solution was added to a portion of the aqueous filtrate of each plant extract followed by addition of concentrated H2SO4. Formation of yellow color indicated the presence of flavonoids.
2.4.5. Test for Steroids
2 ml of acetic anhydride was added to 0.5 g of the methanol extract with 2 ml H2SO4. The change in colour from violet to blue or green indicated the presence of steroids.
2.4.6. Test for Essential Oils
To 2 ml of the extract, 0.1 ml of 2 M sodium hydroxide was added, followed by a small quantity of 2 M hydrochloric acid and shaken. A white precipitate indicated the presence of essential oils.
2.4.7. Phenols
To 2 ml of the extract, 2 ml of Iron III chloride was added to the solution. A deep bluish-green solution indicated the presence of phenols.
2.5. In Vitro Antimicrobial Activity Testing
This study was a retrospective laboratory-based study of thirty stocked suspected Acinetobacter baumannii isolates at Aga Khan University Hospital in Nairobi which evaluated the qualitative phytochemicals composition of Nepeta cataria and Basella alba through the assessment of the activity and toxicity of the extracts in PAUSTI Laboratory inside Jomo Kenyatta University of Agriculture and Technology from February to July 2018. Fresh and pure colonies of Acinetobacter baumannii were used for the susceptibility testing on the Mueller-Hinton agar. Bacteria were sub-cultured on Blood agar and Brain Heart Infusion agar overnight at 37˚C. The fresh overnight cultures were diluted into the sterile normal saline equivalent to 0.5 MacFarland standard to prepare the test organism and inoculated on Mueller Hinton agar plates to determine the antibacterial activity of Basella alba and Nepeta cataria extract. 600 mg, 400 mg and 200 mg of methanolic and aqueous extracts of Basella alba and Nepeta cataria were weighed and stored in well labelled sterile centrifuge tubes for further dilution. To obtain the working solution, the methanolic and the aqueous extract were diluted with distilled water [17] . The antimicrobial activity of the plants extracts was determined by well diffusion method described by [18] . Using sterile swabs, the bacterial suspension of Acinetobacter baumannii was spread on the plates. Six millimeter well was cut in the plates with the sterile cork borer [19] . Using pipette, 100 µl of the solutions prepared was introduced into each well at different concentration. The plates were incubated overnight at 37˚C. The antimicrobial activity of the extract was recorded by measuring the zone of inhibition formed around the discs in millimeter [13] .
2.6. Determination of the Minimal Inhibitory Concentration
Acinetobacter species used in this study were confirmed by culturing on the Sheep Blood agar and Brain Heart Infusion agar media followed by biochemical test using API. Based on CLSI guidelines, MICs was determined by using the broth microdilution method [18] . Nine milliliters of the nutrient broth was dispensed into the test tubes and one milliliter of the stock working solution was added to the first tube and diluted serially to the next tubes. The negative control was prepared without adding the plant extracts while for the positive control, one milliliter of 70% methanol was added. One milliliter of the bacterial suspension according to 0.5 MacFarland was added to all the test tubes followed by overnight incubation at 37˚C. For the 96 well plates, the serial dilution was performed with 50 µl of reverse gradient dilution of the plant extract and 50 µl of the test organism suspension [20] . The plates were covered with plate sealing tape and incubated at 37˚C for 24 hours [21] .
2.7. Toxicity Testing on Brine Shrimp
The Toxicity testing was done to assess the active compounds for methanolic extracts of Nepeta cataria and Basella alba using the brine shrimps. Brine shrimp eggs were bought from Aqua-pet shop in Nairobi. They were dissolved in artificial seawater then transferred into a hatching chamber with a covered and light part for hatching (four days). Using a magnifying glass and pipette, ten nauplii were added to the previously labelled test tubes containing nine milliliters of salted water and one milliliter of the working plant extract solution at different concentrations (600, 400, and 200 mg/ml) by serial dilution from the stock solution [22] . Pure methanol was used as a positive control while artificial seawater was used as a negative control [17] . These tubes were incubated uncovered at room temperature for 24 hours. After 24 hours, the live nauplii were counted and recorded. The percentage mortality was calculated by dividing the number of dead nauplii by the total number and then multiplied by 100% [23] .
2.8. Statistical Analysis
Data obtained was analysed using Statistical Package for the Social Sciences (SPSS) to determine the significance (p-value) with values given in means ± SD for each measurement. Graphs were established using GraphPad Prism and Microsoft Excel.
3. Results and Discussion
3.1. Extraction and Phytochemical Screening
The percentage yield for Basella alba in both methanolic and aqueous extracts 4.63 and 1.93 while that of Nepeta cataria was 4.03 and 3.11 respectively (Table 1 and Table 2).
There was significant difference in the percentage yield of methanol and aqueous extracts of Basella alba since the p-value was <0.05 unlike in Nepeta cataria extracts (p-value > 0.05). A previous study reported methanol to be the most effective solvent enabling maximum separation of different phytochemicals. Preliminary analysis of the extracts revealed the presence of secondary metabolites in leaves of B. alba extract [13] . Using different parts of the plant, the study carried out by Adegoke and Ojo, (2017) [24] reported that the leaf fraction of Basella alba had the highest percentage yield (24.30%) than Basella alba fruit fraction with a yield of 11.13% with methanol used as extraction solvent. The results obtained by Iloki-Assanga et al. (2015) [25] proved that methanol was the most effective solvent for isolation of phenolic compounds, whereas much lower yields were obtained from samples extracted with acetone.
3.2. The Phytochemical Analysis
The phytochemical screening in the present study showed the presence of various phytochemical constituents from the methanolic and aqueous extracts of Nepeta cataria and Basella alba. From the methanolic extract of Nepeta cataria, the phytochemicals present included phenols, tannins, saponins, flavonoids and essential oils while in the aqueous extraction. All the phytochemicals detected using methanolic extracts were present except flavonoids. Basella alba methanolic extract revealed the presence of phenol, phlobatannin, saponin, flavonoid and steroid whereas saponin was the only phytochemical detected in the aqueous plant extract (Table 3).
Previous studies showed presence of flavonoid, phenol, steroids and essential oils in methanolic extract of Nepeta cataria [26] [27] [28] . Phenols and
Table 1. Determination of the percentage yield from Basella alba extracts using methanol and water.
Table 2. Determination of the percentage yield from the Nepeta cataria extracts using methanol and water.
Table 3. Preliminary phytochemicals analysis of Nepeta cataria and Basella alba extracts. The (+) signify presence of phytochemicals and (−) signify absence of phytochemicals.
flavonoids have previously been detected in aqueous extracts of Nepeta cataria [24] [29] . Other studies report presence of phenols, saponins, tannins and oils from Nepeta cataria leaf methanolic extracts whereas tannins, oils and phenols were detected in aqueous extracts [30] [31] [32] . A study by Ta et al. (2014) [33] reported the presence of tannins, saponin, glycoside, flavonoids, alkaloids and phenols from the ethanolic and aqueous Basella alba extracts. The result of the crude methanolic extracts of Basella alba indicated the presence of tannin, terpene, steroids, saponins, anthraquinone, in the leaf and stem extracts of the plant, and carbohydrate in the stem [34] .
3.3. In Vitro Antimicrobial Activity Testing
All the methanolic Nepeta cataria concentrations that were used (600 mg/ml, 400 mg/ml and 200 mg/ml) demonstrated antimicrobial activity. Antimicrobial activity of methanolic Nepeta cataria extracts was greater than those of Basella alba (Plate 1, Plate 2).
The only concentration of Nepeta cataria aqueous extracts that demonstrated antimicrobial activity was 600 mg/ml. Basella alba aqueous extract did not show any antimicrobial activity against Acinetobacter baumannii at the different concentrations.
From the two solvents used for plant material extraction, the methanolic extract showed a highest antimicrobial activity against Acinetobacter baumannii at the three different concentrations than the aqueous extract (Figure 1). Crude extract of methanolic Nepeta cataria exhibited an antimicrobial activity by presenting a zone of inhibition around the wells of 600, 400 and 200 mg/ml. From the aqueous extract, the zone of inhibition at 600 mg/ml was only recorded.
Results obtained in previous study revealed that the aqueous extracts of Nepeta cataria possess potential antibacterial activity as compared to its antifungal activity [4] . The methanolic crude extract of Nepeta cataria showed antimicrobial activity against all the test microorganisms except for Staphylococcus aureus and Salmonella typhii [4] [11] . The antimicrobial activity observed for Nepeta cataria in the study done by [26] may be attributed to the presence of main components in the essential oil.
Of all the Basella alba aqueous extracts tested at 600, 400, 200 mg/ml concentration, no zone of inhibition was recorded against Acinetobacter baumannii contrary to the methanolic extract which showed the greater activity at 200 and 400 mg/ml. Kumar et al. (2013) [30] reported a significant growth inhibition on human cancer cell lines and momentous zone of inhibition for microorganisms studied. The methanolic extracts exhibited marked antimicrobial activity against gram positive and gram-negative bacteria and fungi. Basella alba showed good inhibitory activity against Aspergillus niger. This mild activity of the aqueous was also reported in another study [35] . The results reported by Toyang et al. (2012) [36] showed that the solvents dichloromethane and methanol extracted compounds with better activity than aqueous extracts.
3.4. Determination of the Minimal Inhibitory Concentration
For Nepeta cataria and Basella alba crude extracts, the results of minimum inhibitory concentration (MIC) against the test Acinetobacter baumannii isolates were as shown in (Plate 3).
The values of MIC varied with plant samples from 10−1 to 10−9 mg/ml. From the macro dilution using test tubes, there was bacterial growth in all the tubes

Plate 1. Antimicrobial activity of methanolic extract of Basella alba (a) and Nepeta cataria (b) against Acinetobacter baumannii.

Plate 2: Antimicrobial activity of aqueous extract of Basella alba (a) and Nepeta cataria (b) against Acinetobacter baumannii.
Figure 1. The percentage of efficacy response of methanolic and aqueous extracts of Nepeta cataria and Basella alba.
inoculated. Using the 96 well plates for the methanolic extract of both plants, the screening revealed that Nepeta cataria and Basella alba methanolic extracts were the most sensitive to Acinetobacter baumannii at the lower MIC value of 60 mg/ml where there was not bacterial growth. The antibacterial screening of the Nepeta cataria showed that methanolic extracts exhibited antibacterial activity against Staphylococcus aureus, Klebsiella pneumoniae and Salmonella typhii with MIC of 0.1 mg/ml and inactivity against Proteus mirabilis, Shigella
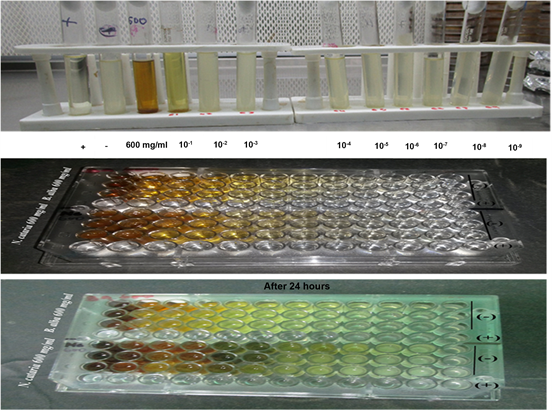
Plate 3. Determination of MIC using macro and micro (96-wells) two-fold dilution.
dysenteriae, Escherichia coli and Pseudomonas aeruginosa [27] . Moreover, the results obtained by different authors vary widely because of that there are no standard criteria for the evaluation of the plant activity. The MIC and MBC were 50 mg/ml for P. aeruginosa and E. coli of Basella alba of both the leaf and stem [34] . The essential oils of Nepeta cataria inhibited the growth of the examined bacteria at concentrations of 0.125 - 2 µL/ml [37] . However, only few literatures are available on the evaluation of the aqueous and methanolic activity of the Nepeta cataria and Basella alba extract, it is difficult to give a good comparison of this data with some variables such as environmental and climatic conditions of the plant and the method of extraction and antimicrobial screening.
3.5. Toxicity Testing on Brine Shrimp
All the hatched eggs were killed by methanolic Nepeta cataria and Basella alba extracts as compared to the 70% methanol used as positive control. 65% of dead eggs was recorded for Nepeta cataria aqueous extract at 200 mg/ml and 100 % for 400 and 600 mg/ml. For aqueous Basella alba, it was 55% for 200 mg/ml; 85% for 400 mg/ml and 100% for the 600 mg/ml (Figure 2).
This could be attributed to the phytochemicals recorded from the extraction using methanol, which is an organic solvent with a distinctive odor like that of ethanol however far more toxic than ethanol. From the plant materials, Basella alba showed the lowest rate of toxicity than Nepeta cataria whether 70 % methanol or water were used. 65% of death was recorded for Nepeta cataria aqueous extract at 200 mg/ml and 100% for 400 and 600 mg/ml. The methanolic Nepeta cataria shows highest mortality ratio at different concentration of methanolic leaf extract with LC50 of 0.98 mg/L against larvae of Anopheles
Figure 2. Toxicity testing of the plant extracts using brine shrimp eggs.
gambiae [38] . Although, there was non-significant difference between the aqueous extracts and the sea water, the aqueous extract had the least mortality of 25% while the organic extraction had the highest mortality of 100%. This could explain why most traditional herbal medicines are prepared using water as a solvent because it is not or less toxic as reported in previous study [39] . Some other studies reported that methanolic extract of Basella alba leaf did not cause liver and muscle damage in live pups indicating that it is safe for consumption [40] [41] . The phonological age of the plant, percentage humidity of the harvested material, geographical location, climatic conditions, soil condition, time of harvest, and the method of extraction are possible sources of variation for the chemical composition, toxicity and bioactivity of the extracts [11] .
4. Conclusion
From the present study, the methanolic extracts of Nepeta cataria and Basella alba showed the high presence of phytochemicals compared to their aqueous extracts. The bioactivity of the methanolic and aqueous extracts of Nepeta cataria and Basella alba against clinically resistant Acinetobacter baumannii isolates was revealed, with a greater antimicrobial activity of methanolic extracts of Nepeta cataria than the Basella alba methanolic extracts. From methanolic plant material extracts, the cytotoxic activity on the brine shrimp recorded an LC50 value that was less than 200 mg/ml for the aqueous extracts and an antimicrobial effect of against Acinetobacter baumannii an MIC of 60 mg/ml.
Acknowledgements
The authors acknowledge African Union Commission (AUC) for the scholarship and research funding through Pan African University Institute of basic Science, Technology and Innovation (PAUSTI), Jomo Kenyatta University of Agriculture and Technology and Japan International Conference Agency (JICA) for the financial support.
Conflicts of Interest
The authors declare no conflicts of interest regarding the publication of this paper.
Cite this paper
Morombaye, S.M., Kangogo, M., Revathi, G., Nyerere, A. and Ochora, J. (2018) Evaluation of the Antimicrobial Effect of Nepeta cataria and Basella alba against Clinically Resistant Acinetobacter baumannii in Nairobi, Kenya. Advances in Microbiology, 8, 790-803. https://doi.org/10.4236/aim.2018.810052
References
- 1. Shamsizadeh, Z., Nikaeen, M., Nasr, E.B., Mirhoseini, S.H., Hatamzadeh, M. and Hassanzadeh, A. (2017) Detection of Antibiotic Resistant Acinetobacter baumannii in Various Hospital Environments: Potential Sources for Transmission of Acinetobacter Infections. Environmental Health and Preventive Medicine, 22, 44. https://doi.org/10.1186/s12199-017-0653-4
- 2. Cheesman, M., Ilanko, A., Blonk, B. and Cock, I. (2017) Developing New Antimicrobial Therapies: Are Synergistic Combinations of Plant Extracts/Compounds with Conventional Antibiotics the Solution? Pharmacognosy Reviews, 11, 57-72. https://doi.org/10.4103/phrev.phrev_21_17
- 3. Miyasaki, Y., Rabenstein, J.D., Rhea, J., Crouch, M.-L., Mocek, U.M., Kittell, P.E. and Liu, G.Y. (2013) Isolation and Characterization of Antimicrobial Compounds in Plant Extracts against Multidrug-Resistant Acinetobacter baumannii. PLoS ONE, 8, e61594. https://doi.org/10.1371/journal.pone.0061594
- 4. Bandh, S., Kamili, A., Ganai, B.A. and Lone, B.A. (2011) Evaluation of Antimicrobial Activity of Aqueous Extracts of Nepeta cataria. Journal of Pharmacy Research, 4, 3141-3142.
- 5. Colalto, C. (2017) What Phytotherapy Needs: Evidence-Based Guidelines for Better Clinical Practice. Phytotherapy Research, 32, 1-13.
- 6. Shasank, S.S. and Rabindra, N.P. (2017) Isolation of ESBL-Producing Gram-Negative Bacteria and in Silico Inhibition of ESBLs by Flavonoids. Journal of Taibah University Medical Sciences, 11, 217-229.
- 7. Ochwang, I.D.O., Kimwele, C.N. and Oduma, J.A. (2016) Phytochemical Screening of Medicinal Plants of the Kakamega Country, Kenya Commonly Used against Cancer. Medicinal & Aromatic Plants, 5, 277. https://doi.org/10.4172/2167-0412.1000277
- 8. Revathi, G., Siu, L.K., Lu, P.L. and Huang, L.Y. (2013) First Report of NDM-1-Producing Acinetobacter baumannii in East Africa. International Journal of Infectious Diseases, 17, e1255-e1258. https://doi.org/10.1016/j.ijid.2013.07.016
- 9. Chen, L.K., Kuo, S.C., Chang, K.C., Cheng, C.C., Yu, P.Y., Chang, C.H. and Tseng, C.C. (2017) Clinical Antibiotic-Resistant Acinetobacter baumannii Strains with Higher Susceptibility to Environmental Phages than Antibiotic-Sensitive Strains. Scientific Reports, 7, 1-10. https://doi.org/10.1038/s41598-017-06688-w
- 10. Chaudhary, M. (2012) Molecular Characterization and Antimicrobial Susceptibility Study of Acinetobacter baumannii Clinical Isolates from Middle East, African and Indian Patients. Journal of Proteomics & Bioinformatics, 5, 265-269. https://doi.org/10.4172/jpb.1000248
- 11. Khan, M.E., Mela, B., Teixeira, J.A., Amupitan, J.O., Kubmarawa, D. and Atiko, R. (2011) Phytochemical and Antimicrobial Evaluation of the Potency of Nepata cateria Leaves against Some Pathogens. Medicinal and Aromatic Plant Science and Biotechnology, 5, 169-172.
- 12. Sushila, R., Deepti, A., Dharmender, R., Madhavi, T. and Permender, R. (2010) Cytotoxic and Antibacterial Activity of Basella alba Whole Plant: A Relatively Unexplored Plant. Pharmacologyonline, 3, 651-658.
- 13. Suguna, J., Thenmozhi, S., Parimalam, K., Kalaiselvi, K. and Panneer, S.K. (2015) Antimicrobial and Antioxidant Activity of the Leaf Extract of Basella alba. Human Journals Research Article, 3, 6677.
- 14. Agaie, B.M. and Onyeyili, P.A. (2011) In Vitro Anthelmintic Activity of the Aqueous Leaf Extract of Anogeissus leiocarpus and Its Phytochemical, Proximate and Elemental Contents. Journal of Medicinal Plants Research, 5, 6656-6661. https://doi.org/10.5897/JMPR11.583
- 15. Bamidele, O., Akinnuga, A.M., Olorunfemi, J.O., Odetola, O.A., Oparaji, C.K. and Ezeigbo, N. (2010) Effects of Aqueous Extract of Basella alba Leaves on Haematological and Biochemical Parameters in Albino Rats. African Journal of Biotechnology, 9, 6952-6955.
- 16. Mohammed, S.A., Sanni, S., Ismail, A.M., Kyari, A.S. and Abdullahi, S. (2014) Preliminary Phytochemical and Elemental Analysis of Aqueous and Fractionated Pod Extracts of Acacia nilotica (Thorn mimosa). Veterinary Research Forum.
- 17. Janackovic, P., Gavrilovic, M., Rakic, B., Tesevic, V. and Marin, P. (2016) Brine Shrimp Lethality Bioassay of Selected Gymnosperm and Angiosperm Species. Zbornik Matice Srpske Za Prirodne Nauke, 131, 109-119.
- 18. CLSI (2017) Performance Standards for Antimicrobial Susceptibility Testing. 27th Edition.
- 19. Idris, A., Ietidal, A. and Eihab, I. (2013) Antibacterial Activity of Endophytic Fungi Extracts from the Medicinal Plant Kigelia africana. Egyptian Academic Journal of Biological Sciences, 5, 1-9.
- 20. Elshikh, M., Ahmed, S., Mcgaw, M., Marchant, R., Funston, S., Dunlop, P. and Banat, I.M. (2016) Resazurin-Based 96-Well Plate Microdilution Method for the Determination of Minimum Inhibitory Concentration of Biosurfactants. Biotechnology Letters, 38, 1015-1019. https://doi.org/10.1007/s10529-016-2079-2
- 21. Andrews, J.M. (2001) Determination of Minimum Inhibitory Concentrations. The Journal of Antimicrobial Chemotherapy, 48, 5-16. https://doi.org/10.1093/jac/48.suppl_1.5
- 22. Sarah, Q.S., Anny, F.C. and Misbahuddin, M. (2017) Brine Shrimp Lethality Assay. Bangladesh Journal of Pharmacology, 12, 186-189. https://doi.org/10.3329/bjp.v12i2.32796
- 23. Olowa, L.F. and Nuñeza, O.M. (2013) Brine Shrimp Lethality Assay of the Ethanolic Extracts of Three Selected Species of Medicinal Plants from Iligan City. International Research Journal of Biological Sciences, 2, 74-77.
- 24. Adegoke, G.O. and Ojo, O.A. (2017) Phytochemical, Antioxidant and Antimicrobial Activities in the Leaf, Stem and Fruit Fractions of Basella Alba and Basella Rubra. Science, 5, 73-79.
- 25. Iloki-Assanga, S.B., Lewis-Luján, L.M., Lara-Espinoza, C.L., Gil-Salido, A.A., Fernandez-Angulo, D., Rubio-Pino, J.L. and Haines, D.D. (2015) Solvent Effects on Phytochemical Constituent Profiles and Antioxidant Activities, Using Four Different Extraction Formulations for Analysis of Bucida buceras Leaves and Phoradendron californicum Complementary and Alternative Medicine. BMC Research Notes, 8, 1-14. https://doi.org/10.1186/s13104-015-1388-1
- 26. Adiguzel, A., Ozer, H., Sokmen, M., Gulluce, M., Sokmen, A., Kilic, H. and Baris, O. (2009) Antimicrobial and Antioxidant Activity of the Essential Oil and Methanol Extract of Nepeta cataria. Polish Journal of Microbiology, 58, 69-76.
- 27. Edewor, T.I. and Usman, L.A. (2011) Phytochemical and Antibacterial Activities of Leaf Extracts of Nepeta cataria. African Journal of Pure and Applied Chemistry, 5, 503-506. https://doi.org/10.5897/AJPAC11.074
- 28. Süntar, I., Nabavi, S.M., Barreca, D., Fischer, N. and Efferth, T. (2017) Pharmacological and Chemical Features of Nepeta L. Genus: Its Importance as a Therapeutic Agent. Phytotherapy Research, 32, 185-198.
- 29. Deshmukh, S.A. and Gaikwad, D.K. (2014) A Review of the Taxonomy, Ethnobotany, Phytochemistry and Pharmacology of Basella alba (Basellaceae). Journal of Applied Pharmaceutical Science, 4, 153-165.
- 30. Kumar, S., Prasad, A.K., Iyer, S.V. and Vaidya, S.K. (2013) Systematic Pharmacognostical, Phytochemical and Pharmacological Review on an Ethno Medicinal Plant, Basella alba Leaves. Academic Journals, 5, 53-58.
- 31. Nostro, A., Germano, M.P., Angelo, V.D., Marino, A. and Cannatelli, M.A. (2000) Extraction Methods and Bioautography for Evaluation of Medicinal Plant Antimicrobial Activity. Letters in Applied Microbiology, 30, 379-384. https://doi.org/10.1046/j.1472-765x.2000.00731.x
- 32. Seladji, M., Bekhechi, C., Beddou, F., Dib, H. and Bendimerad, N. (2014) Antioxidant Activity and Phytochemical Screening of Nepeta nepetella Aqueous and Methanolic Extracts from Algeria. Journal of Applied Pharmaceutical Science, 4, 12-16.
- 33. Ta, I., Ajongbolo, Kf. and Aladekoyi, G. (2014) Phytochemical Screening and Antimicrobial Activity of Crude Extracts of Basella alba and Helianthus annuus on Selected Food Pathogens. Research and Reviews: Journal of Microbiology and Biotechnology, 3, 27-31.
- 34. Oyewole, O.A. and Owolabi, O.A. (2012) The Antimicrobial Activities of Crude Methanolic Extracts of Basella alba on Selected Microorganisms. Trade Science Inc.
- 35. Adhikari, R., Kumar, H.N. and Shruthi, S.D. (2012) Review Article a Review on Medicinal Importance of Basella alba Leaves. International Journal of Pharmaceutical Sciences and Drug Research, 4, 110-114.
- 36. Toyang, N.J., Ateh, E.N., Keiser, J., Vargas, M., Bach, H., Tane, P. and Verpoorte, R. (2012) Toxicity, Antimicrobial and Anthelmintic Activities of Vernonia guineensis Benth. (Asteraceae) Crude Extracts. Journal of Ethnopharmacology, 144, 700-704. https://doi.org/10.1016/j.jep.2012.10.016
- 37. Zomorodian, K., Saharkhiz, M.J. and Rahimi, M.J. (2013) Chemical Composition and Antimicrobial Activities of Essential Oil of Nepeta cataria Leaves against Common Causes of Oral Infections. Journal of Dentistry, 10, 329-337.
- 38. Devi, K.K., Mohanraj, R.S. and Dhanakkodi, B. (2013) Mosquitocidial Activities of Spathodea campanulata Methanolic Leaf Extract against the Dengue Vector Aedes aegypti. Asian Journal of Plant Science and Research, 3,138-149.
- 39. Ohikhena, F.U., Wintola, O.A. and Afolayan, A.J. (2016) Toxicity Assessment of Different Solvent Extracts of the Medicinal Plant, Phragmanthera capitata (Sprengel) Balle on Brine Shrimp (Artemia salina). International Journal of Pharmacology, 12, 701-710. https://doi.org/10.3923/ijp.2016.701.710
- 40. Nantia, E.A., Manfo, P.F.T., Beboy, N.E., Travert, C., Carreau, S., Monsees, T.K. and Moundipa, P.F. (2012) Effect of Methanol Extract of Basella alba Leaves (Basellaceae) on the Fecundity and Testosterone Level in Male Rats Exposed to Flutamide in Utero. Andrologia, 44, 38-45. https://doi.org/10.1111/j.1439-0272.2010.01104.x
- 41. Baskaran, G., Salvamani, S., Azlan, A., Ahmad, S.A., Yeap, S.K. and Shukor, M.Y. (2015) Hypocholesterolemic and Antiatherosclerotic Potential of Basella alba Leaf Extract in Hypercholesterolemia-Induced Rabbits. Evidence-Based Complementary and Alternative Medicine, 2015, Article ID: 751714.




