World Journal of Cardiovascular Surgery
Vol.4 No.3(2014), Article ID:43787,7 pages DOI:10.4236/wjcs.2014.43006
Heart Surgery Practice in Sub Saharan Africa: Single Nigerian Institutional Midterm Results and Challenges
Jonathan O. Nwiloh1, Mobolaji A. Oludara2, Philip A. Adebola3
1Department of Surgery, Atlanta Medical Center, Atlanta, USA
2Department of Surgery, Lagos State University Teaching Hospital, Lagos, Nigeria
3Department of Medicine, Lagos State University Teaching Hospital, Lagos, Nigeria
Email: Jnwiloh@gmail.com, boludara2011@gmail.com, adebolapmed@yahoo.com
Copyright © 2014 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/


Received 18 January 2014; revised 18 February 2014; accepted 26 February 2014
ABSTRACT
Background: The majority of prospective cardiac surgical patients in sub Saharan Africa lack access to open heart surgery. We reviewed our midterm results to identify the obstacles to growth and challenges with sustainability. Methods: Records of patients undergoing heart surgery at LASUTH from December 2004 to March 2006 were retrospectively reviewed for clinical and outcome data. Results: Twenty four patients age 10 - 50, mean 28.0 +/− 10.49 years and 13(54.2%) males underwent surgery.12(50.0%) patients had mechanical valve replacements, 11(45.8%) closure of septal defects and 1(4.2%) left atrial myxoma resection. Logistic euroscore for valve patients was 5.81 +/− 4.74 while observed mortality was 8.3% (1/12). Overall 30 days operative mortality was 8.3% (2/24) and major morbidity 4.2% (1/24). Patients with septal defects closure stopped clinic visits within a year. Valve patients follow up was complete in 90.1% with mean duration of 55.2 +/− 15.3 months. Late events occurred only in females with mitral valve replacements. The 5-year freedom from thromboembolism and bleeding was 74.0% and survival 82.0% in valve patients. Conclusion: Despite limited resources heart surgery can safely be performed with good outcomes by trained local personnel under supervision of visiting foreign teams until they are proficient to operate independently. Patients with less complex congenital defects have excellent postsurgical outcomes, while patients with rheumatic valve replacement are subject to ongoing valve related morbidity and mortality therefore require lifetime follow up. Choice of prosthetic valve for the mostly indigent and poorly educated population remains a challenge. We now prefer stented tissue valve despite its known limitations, in child bearing age females desirous of childbirth and others unlikely to comply with anticoagulation regimen. Barriers to sustainability include poor infrastructures, few skilled manpower, inadequate funding and restricted patient access due to inability to pay without third party insurance or government Medicaid.
Keywords:Open Heart Surgery; Prosthetic Valve Choice; Anticoagulation

1. Introduction
Cardiovascular diseases (CVDs) predominantly heart disease and stroke are the number one causes of death globally accounting for 17 million out of the 57 million annual deaths worldwide [1] . Majority of these deaths comes from low and middle income countries such as those found in sub Saharan Africa (SSA) with manpower and infrastructural limitations. Although communicable disease (CDs) especially AIDS presently account for the majority of deaths in Africa, the burden of CVDs is however on the increase with adoption of western lifestyles and is expected to become Africa’s number one killer by 2025. Nigeria the most populous country in Africa with 160 million citizens in 2004 had no active open heart surgery center after the closure of the only program at University of Nigeria Teaching Hospital, Enugu a few years earlier [2] [3] . Patients with heart disease requiring lifesaving surgery who could afford the costs therefore had to travel outside of the country for treatment. It was against this backdrop that Lagos State Government in partnership with an American based non-governmental organization, Global Eagle Foundation commenced heart surgery at Lagos State University Teaching Hospital (LASUTH).
2. Material and Methods
The records of patients who underwent open heart surgery with aide of cardiopulmonary bypass (CPB) at LASUTH between December 2004 and March 2006 during three consecutive cardiac surgery missions were retrospectively reviewed. Patients undergoing non pump heart surgery were excluded from the study. The operated patients were selected from a pool of patients with known heart diseases followed at the Cardiology Clinic. Potential surgical candidates were screened prior to each planned cardiac surgery mission. Diagnoses were established non-invasively through clinical evaluation, electrocardiogram, chest x-ray and transthoracic echocardiogram (TTE). Transesophageal echocardiogram (TEE) and cardiac catheterization were not available at the hospital. Short listed patients were then screened for HIV/AIDS, Hepatitis B and C, and positive patients were excluded from surgery. Pediatric patients less than 10 years were also excluded for technical reasons. Highest priority was given to symptomatic patients with advanced stages of disease due to the limited resources. Patients with valvular heart disease all met the American College of Cardiology/American Heart Association (ACC/ AHA) class 1 indication for surgery. Preoperative risk assessment for valve patients was performed using the logistic Euroscore. All operations were elective and performed via standard median sternotomy with CPB through ascending aortic and bicaval cannulations, except in aortic valve replacements where a single venous cannula were used. Moderate systemic hypothermia at 30 ˚C was utilized and myocardial protection during the period of aortic cross clamping was with cold blood cardioplegia administered antegrade, retrograde or both. Swan Ganz catheter was reserved when available for sicker patients to facilitate hemodynamic management. Intraaortic balloon pump (IABP) was used when cardiogenic shock was refractory to inotropic support. All mitral valve replacements were performed with preservation of the subvalvular apparatus. There was no attempt at valve repair due to lack of intraoperative TEE to assess competency of repair, and also because of need for complete resolution of the pathology as the surgery offered the only one chance opportunity for cure in these mostly indigent patients. Intraoperative blood conservation techniques utilized included retrograde pump priming, cell saver and removal of patient’s blood for later reinfusion at completion of CPB and heparin reversal. Valve replacement patients were started on intravenous heparin 48 hours postoperatively if no bleeding problems and discontinued after prolongation of International normalized ratio (INR) within target range with Coumadin. Anticoagulation was continued after discharge with target INR between 2.0 - 3.0 and 2.5 - 3.5 for aortic and mitral mechanical valves respectively.
Data were entered into an excel spreadsheet and imported into Sigma Plot (Systat Software, Inc., San Jose, CA) for statistical analysis. Operative mortality was defined as death within 30 days of surgery. Categorical variables were reported using number and percent of observations, while continuous variables were reported as mean +/− standard deviation. Survival rates were calculated using the actuarial Kaplan Meier method. Post hospital discharge follow-up was through clinic visits and telephone calls. Follow up for this review was up to December 31, 2010.
3. Results
Twenty four patients comprising of 13(54.2%) males and 11(45.8%) females, age range 11 - 50, mean 28.0 +/− 10.49 years underwent open heart surgery during this time period. 12(50.0%) patients had valve surgery consisting of 8 mitral and 4 aortic valve replacements. Majority 75.5% (6/8) of mitral valve replacement patients were females, while majority 75.0% (3/4) of aortic valve patients were males. All valve replacements were with mechanical prosthesis, comprising 8 St. Jude Medical and 4 ATS valves. Chronic atrial fibrillation was present only in patients with mitral valve disease occurring in 62.5% (5/8) patients, one of who underwent concomitant left and right atrial radiofrequency ablation. 11(45.8%) patients underwent closure of intracardiac septal defects and 1(4.2%) patient had resection of a large left atrial myxoma. CPB time mean was 131.2 +/− 60.1 minutes (range 48 - 265) and aortic cross clamp mean was 79.6 +/− 39.3 minutes (range 20 - 132). Length of hospital stay mean was 13.7 +/− 5.4 days (range 7 - 27). One patient (4.2%) with chronic aortic insufficiency and severe LV dysfunction after aortic valve replacement developed hemodynamic instability in the ICU and required insertion of IABP. All patients were extubated within 24 hours. Major morbidity occurred only in one patient (4.2%) with mediastinal reexploration for post-operative bleeding. There were 2(8.4%) operative deaths. One male patient with severe left ventricular (LV) dysfunction and supra systemic pulmonary hypertension, died from cardiogenic shock following mitral valve replacement during our first surgical mission. The second death occurred in a female patient with undiagnosed 1 cm patent ductus arteriosus (PDA) on preoperative TTE that was inadvertently injured during surgery for ventricular septal defect (VSD) closure. Repair of the tear in the aortic arch required deep hypothermic circulatory arrest (DHCA), and patient died from coagulopathy and bleeding, Table 1. Follow up in valve patients was complete in 90.9%, with only one patient (9.1%) lost to follow up at 36 months after he relocated to the United States. Mean duration of follow up was 55.2 +/− 15.3 months, range 27 - 73 months. All valve patients preoperatively were either in NYHA Class III/IV and postoperatively were in Class I with the exception of one patient in Class II. There were 2 (18.2%) late deaths, both in two females with mitral valve replacements. One patient with ATS valve who was non-compliant with her Coumadin regimen died in hospital at 27 months from thromboembolic stroke. The second patient with a St. Jude valve who was on Coumadin and compliant with INR in target range died suddenly at home at 36 months. Late major morbidity occurred in one female patient with a St. Jude mitral valve who had bleeding and two recurrent spontaneous 1st trimester abortions and is yet to have a live baby. For valve patients, the 5-year survival was 82.0% and 5-year freedom from thromboembolism and bleeding 74.0%, Figures 1 and 2. Patients who underwent closure of atrial and ventricular septal defects were lost to follow up within one year of surgery.
4. Discussion
Open heart surgery is now widely practiced worldwide since the first successful human closure of congenital heart defect with the heart lung machine in 1953 by John Gibbon. However, over half a century later, only very few hospitals in SSA have the capacity to perform heart surgery for a myriad of reasons. To put it in perspective
Table 1. Operations, morbidity, mortality.
Legend: ASD—Atrial Septal Defect; VSD—Ventricular Septal Defect; MVR—Mitral Valve Replacement; AVR—Aortic Valve Replacement; LA— Left Atrium.
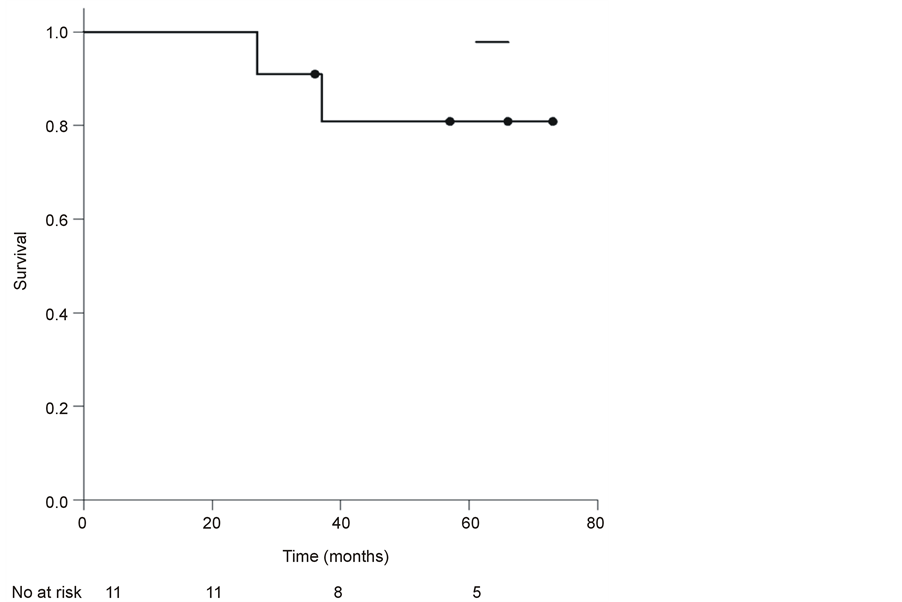
Figure 1. Kaplan-Meier survival analysis for valve patients.
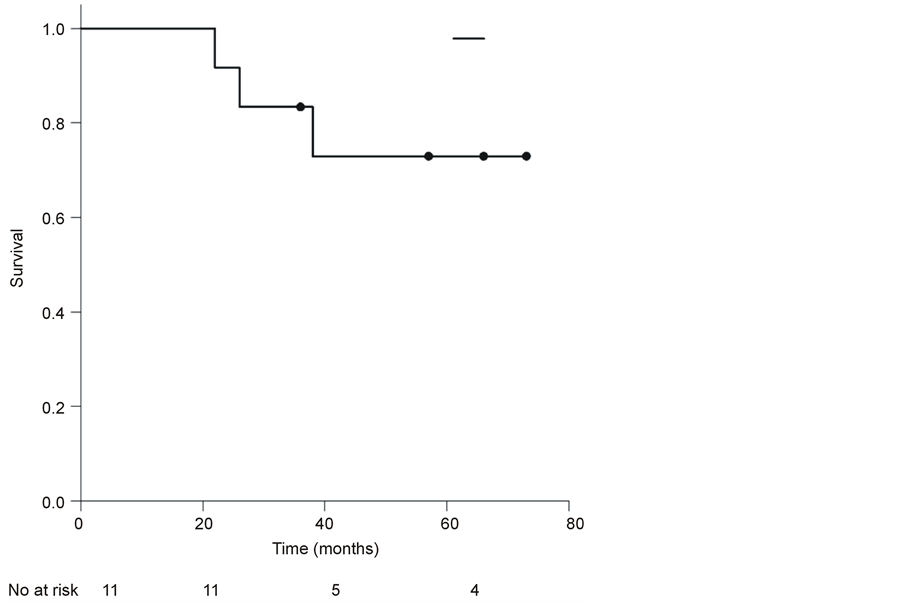
Figure 2. Freedom from bleeding & thromboembolism for valve patients.
there are 1222 open heart surgeries per million population in North America compared to 18 per million in Africa [1] . Majority of the heart surgery programs in Africa are concentrated mainly in Egypt and South Africa, with only a scattered few in West, East and Central Africa [4] [5] . In SSA as in other developing parts of the world, the challenges associated with commencing open heart surgery are multifactorial and often seems insurmountable. Limited government funding for public hospitals and manpower shortage are two obvious major impediments. A 2008 WHO report [6] states that Africa bears 25% of the global burden of disease with only 2% of the workforce. MacGowan [7] in his worldwide review of surgical manpower estimates that Africa may have less than 1% of the number of surgeons in the U.S. despite having three times the population. Similarly Turino [8] in a 2002 review of worldwide distribution of cardiothoracic surgeons per million population shows North America with 26.7, Western Europe 27.8, Europe 8.9, South America 2.6, Asia 0.99 and Africa 0.26. Africa comes a distant last with <1% the number of cardiothoracic surgeons in North America. In a more recent unpublished 2012 survey by the Pan Africa Society of Cardiovascular Surgeons (PASCATS) there were only 933 cardiothoracic surgeons registered with the cardiothoracic surgery network from Africa which has a population of 1.1 billion. Of these, 668 (71.6%) were in North Africa with a surgeon ratio of 3:1 million and the remaining 256 (28.4%) in SSA with a ratio of 0.3:1 million. Nigeria the most populous country in Africa with 160 million had only 35 cardiothoracic surgeons giving a ratio of 0.00000021 per million, and with vast majority practicing non cardiac thoracic surgery. Other mitigating factors include inadequate infrastructures and inability of patients to afford the expense associated with heart surgery in the absence of third party insurance payers or government Medicaid assistance for the poor. The infrastructural limitations are evident right from the onset of illness when challenges are often encountered in establishing the correct diagnosis in most hospitals [9] . While a simple diagnostic tool such as transthoracic echocardiography is widely available in the developed World, in SSA countries such as Nigeria, this tool remains a luxury in majority of the hospitals. The diagnostic challenges are further compounded because there are few trained and experienced echocardiographers and physicians that can accurately perform and interpret the results respectively. Complementary diagnostic modalities such as TEE, Cardiac MRI and cardiac catheterization are rare to non-existent in Nigeria as in most SSA Countries. Determining patient’s operability could therefore on occasions be quite challenging in the absence of a cardiac catheterization. Pulmonary artery pressures estimated by TTE were sometimes misleading. With unavailability of swan ganz catheter for most cases, correct pulmonary artery pressures could only be accurately determined by direct measurement after sternotomy. Oxygen saturations were measured intraoperatively at different levels to calculate step up to confirm diagnosis and also adequacy of shunt closure. Fortunately with the young age of operated patients been predominantly less than 40 years, there were no concerns for possible occult coronary artery disease (CAD). The vast majority of patients in SSA including Nigeria requiring heart surgery have either congenital or acquired rheumatic valvular heart disease. Most of these are found in pediatric, adolescence and young adult population. Because of the hitherto unavailability of open heart surgery in Nigeria, many succumb early to their disease and do not survive to adulthood. CAD is relatively rare although there is however now compelling evidence that there is an increasing incidence of CAD with the recent private hospital opening of a cardiac catheterrization laboratory in Lagos performing percutaneous coronary intervention and the referral of patients for coronary artery bypass surgery. CAD therefore appears to have been previously under diagnosed due to lack of definitive diagnostic tools. In the present series though, we were able to achieve a high diagnostic accuracy of most pathologies with only TTE due to the expertise of the local cardiologist. One patient had an undiagnosed large PDA that was inadvertently injured at surgery and required DHCA for repair. Patient subsequently died from bleeding secondary to coagulopathy. Contributory factors were also the lack of component blood therapy. Many blood banks in Nigeria can only transfuse whole blood and lack capacity to separate different blood components. This practice can potentially result in transfusion of large blood volumes in patients with post cardiotomy bleeding that might otherwise require only platelets, fresh frozen plasma or cryoprecipitate for hemostasis. Many of our patients because of their young age had few co morbidities other than malnutrition from cardiac cachexia secondary to long standing heart disease. Valvular patients especially those with mitral disease and large left atrium also frequently had associated chronic atrial fibrillation. The observed 30 days mortality of 8.3% in the valve surgery subgroup was within the range predicted by the logistic euroscore. The foreign team nurses working with the local nursing staff were able to provide excellent postoperative care in less than ideal circumstances which also contributed to the good clinical outcome of the surgeries. The use of mechanical valve in all patients was based on the rationale that these patients were unlikely to have a second opportunity should another surgery be required for early failure of a repair or premature structural deterioration with bioprosthetic valve. However the trade-off was the anticoagulant related problems of bleeding and thromboembolism associated with mechanical valves. 5 year freedom from thromboembolism or bleeding was 74.0%. Although patients with chronic atrial fibrillation regardless of implanted valve type may still require anticoagulation, they could at least potentially stop with bioprosthetic valve with less risk of disastrous consequences compared to mechanical valves. Atrial radiofrequency ablation which has a high rate of conversion to sinus rhythm in most patients would be of great help with these patients in avoiding long term anticoagulation except in those with mechanical valves. The available atricure machine was damaged with electrical power surge during the first usage and therefore was not available for our subsequent patients with chronic atrial fibrillation. The one patient who had ablation has remained in sinus rhythm for 5 years post surgery. The 82% 5 year survivalin our mechanical valve cases is within the range reported in a similar demographic population from South Africa [10] and definitely superior to medical management as was the case prior to onset of the open heart program. There were no reoperations during the study period but there were two late deaths, one valve related and the second sudden and also likely valve related. One female patient on Coumadin for prosthetic valve has had trouble keeping pregnancies due to bleeding. Because of these experiences over the years with anticoagulation especially in young females desiring children, compliance issues and questionable accuracy of INR results from different laboratories, we have been compelled to reconsider our preference for mechanical valve despite the advantage of longer durability. With an unregulated local laboratories and largely indigent illiterate population afflicted with rheumatic heart disease, we now prefer a stented tissue valve when repair is not feasible especially in child bearing age females and other patients unlikely to comply with required lifelong anticoagulation and monitoring. Most patients and their families when fully informed in terms they can comprehend of these various local limitations and the long term pros and cons of biological versus mechanical valve, now tend to prefer the risks associated with biological valves. Most patients with uncomplicated isolated atrial and ventricular septal defects who survived surgery all did well and stopped clinic follow up within one year, as they no longer felt the need to see a physician in the absence of any further problems. The valve patients however require a lifetime of follow up and most continued with clinic visits during the study period. Study limitations include been retrospective, small number of patients and therefore limited statistical power. It however represents a significant progress in the most populous country in Africa, and has provided us an insight to the prevalent local problems in establishing a sustainable heart surgery program and how to surmount the challenges. There is need when working under less than ideal conditions prevalent in most of SSA, to be flexible and innovative in other to manage and maximize the limited resources for the maximum number of patients. This includes recycling of disposable consumables when it can be done safely, although these would be totally unacceptable by Western standards. However, with many competing interests for the limited healthcare budget, and a large pool of cardiac patients awaiting surgery, reusing supplies extends the services to more patients than might otherwise be possible. The surgical missions represented a paradigm shift in healthcare delivery at LASUTH, as the experience gained by the local physicians and nursing personnel in management of cardiac patients, in combination with improvements in the intensive care unit and blood bank services were subsequently deployed for treatment of other critically ill non cardiac patients with resultant improvement in quality of care for the healthcare system overall. The surgical mission model no doubt is temporal, but it helps presently fill a void and provides hands on practical experience for the local team, while building local capacity as a long term strategy. To develop and sustain new open heart programs in SSA therefore will require clearly defined attainable goals, especially boosting surgeon ratio by increasing the number of trainees in thoracic surgery residencies easily supported by the large pool of patients needing heart surgery. There is also need for a more comprehensive cardiovascular healthcare policy by the respective SSA governments, including policies encouraging private sector participation in establishing more heart surgery programs and residency training. Most African Governments have tended to emphasize and devote most of their healthcare budget to primary care and often consider surgery a luxury. However others such as Ozgediz et al. [11] argue that surgery has long been neglected within global public health despite increasing evidence of cost effective surgical cure or palliation for many diseases in low and middle income countries as found in SSA. There is need therefore for governments to increase the percentage of the health budget allocated to tertiary care and strive to increase third party insurance coverage to more of the population, while offering subsidized medical assistance to the poor needing access to specialized surgical care such as open heart surgery.
In conclusion, the pioneering collaborative effort between LASUTH and Global Eagle Foundation, USA demonstrated the feasibility of performing heart surgery in a resource limited SSA Country like Nigeria with acceptable morbidity and mortality. These encouraging initial results have served as an impetus for the Lagos State government to construct a cardiac and renal center, and undertake human capacity building to improve the cardiac surgical workforce. It is hoped that over time with continued support and close supervision the local personnel will eventually be proficient to practice independently and sustain the heart surgery program which now serves as a beacon of hope to patients with ravages of heart diseases requiring surgical treatment.
References
- Pezella, A. (2002) International Cardiac Surgery: A Global Perspective. Seminars in Thoracic and Cardiovascular Surgery, 14, 298-320. http://dx.doi.org/10.1053/stcs.2002.0140298
- Anyanwu, C., Ihenacho, H., Okoroma, E., et al. (1982) Initial Experience with Open Heart Surgery in Nigeria. Tropical Cardiology, 8, 123-127.
- Eze, J. and Ezemba, N. (2007) Open Heart Surgery in Nigeria: Indication and Challenges. Texas Heart Institute Journal, 34, 8-10.
- Metras, D., Ouezzin-Coulibaly, A., Ouattara, K., et al. (1983) Open Heart Surgery in Tropical Africa-Results and Peculiar Problems of the 1st 300 Cases of Extracorporeal Circulation Performed in Abidjan. La Presse Médicale, 12, 621-624.
- Edwin, F., Sereboe, L., Tettey, M., et al. (2010) Experience from a Single Centre Concerning the Surgical Spectrum and Outcome of Adolescents and Adults with Congenitally Malformed Hearts in West Africa. Cardiology in the Young, 20, 159-164. http://dx.doi.org/10.1017/S1047951109990679
- WHO (2006) World Health Report: Working Together for Health. http://www.who.int/whr/2006/whr06en.pdf
- MacGowan, W. (1987) Surgical Manpower Worldwide. Bulletin of the American College of Surgeons, 72, 5-7, 9.
- Turino, M. (2002) EACTS: Carrying the Torch. European Journal Cardio-Thoracic Surgery, 22, 857-869.
- Edwin, F., Tettey, M., Aniteye, E., et al. (2011) The Development of Cardiac Surgery in West Africa—The Case of Ghana. The Pan African Medical Journal, 9, 15.
- Williams, M.A. and Van Riet, S. (2006) The On-X Heart Valve: Mid-Term Results in a Poorly Anticoagulated Population. The Journal of Heart Valve Disease, 15, 80-86.
- Ozgediz, D., Jamison, D., Cherian, M. and McQueen, K. (2008) The Burden of Surgical Conditions and Access to Surgical Care in Low and Middle Income Countries. Bulletin of World Health Organization, 86, 846-847.


