World Journal of Cardiovascular Surgery
Vol. 3 No. 2 (2013) , Article ID: 32776 , 3 pages DOI:10.4236/wjcs.2013.32006
Surgical Experience of a Partial Atrioventricular Septal Defect in an Elderly Patient: A Case Report
1Department of Cardiovascular Surgery, Fuji Heavy Industries Health Insurance Society Ota Memorial Hospital, Ota, Japan
2Department of Cardiovascular Surgery, Kameda Medical Center, Chiba, Japan
Email: *sugiharu0204@gmail.com
Copyright © 2013 Yukiharu Sugimura et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received April 16, 2013; revised May 16, 2013; accepted May 22, 2013
Keywords: Partial Atrioventricular Septal Defect; Incomplete Endocardial Cushion Defect; Mitral Regurgitation; Elderly Patient; Repair
ABSTRACT
The following paper describes patch closure (bovine pericardial sheet) of an ostium primum atrial septal defect and mitral valve repair (sutured mitral valve cleft + autologous pericardial annuloplasty + Alfieri’s method) in a 50-year-old man. He had been perfectly well until he was brought to the emergency room because of acute heart failure. Chest radiography revealed right-side heart enlargement. Electrocardiography indicated atrial flutter. Echocardiography revealed a large ostium primum atrial septal defect and moderate mitral regurgitation. The pulmonary-to-systemic blood flow ratio was 3.24. First, cardiologists performed catheter ablation of the cavotricuspid isthmus for atrial flutter. We performed patch closure of an ostium primum atrial septal defect and mitral valve repair after the patient’s heart failure was under control. The patient was discharged 13 days postoperatively in a satisfactory condition without any critical complications.
1. Introduction
Partial atrioventricular (AV) septal defect is a congenital heart disease that is seldom observed in adult patients. The aim of this report is to share our clinical experience of the surgical treatment for a partial AV septal defect, particularly mitral regurgitation, for which various techniques were used.
2. Case
We report the case of a patient whose first clinical symptom was dyspnea. The patient was a normal 50-year-old obese man with no medical history of cardiac disorders. He had undergone routine annual medical check-ups but not pointed out anything except that he gained 26 kg in the last 2 years. He arrived at the emergency room in a severely affected condition. At admission, his oxygen saturation was 91% on room air. Physical examination revealed rapid pulse rate and fixed splitting of the second heart sound; no murmur was audible. Chest radiography showed infiltrations in both the lower lung zones, which suggested right-side heart enlargement (Figure 1). Electrocardiography (ECG) indicated atrial flutter (AFL) with 2:1 AV conduction. Transthoracic echocardiography (TTE) and transesophageal echocardiography (TEE) showed a dilated right ventricle, paradoxical movement of the interventricular septum, and a left-to-right shunt due to a large ostium primum atrial septal defect (ASD) (Figure 2). Moderate mitral regurgitation (MR) was found, but mitral valve cleft was not evident in TTE and TEE. Coronary angiography revealed normal coronary arteries. Cardiac catheterization revealed a pulmonary-to-systemic blood flow ratio (Qp/Qs) of 3.24, with pulmonary arterial pressure of 29/18 mmHg (mean: 23 mmHg). The patient was therefore diagnosed with acute heart failure because of a congenital abnormality of endocardial cushions and AFL. After treatment for acute heart failure, cardiologists performed catheter ablation of the cavotricuspid isthmus for AFL, and his sinus rhythm was maintained. Furthermore, surgical repair was planned for partial AV septal defect with MR.
The ascending aorta was cannulated, and bicaval cannulation was performed. A left ventricular vent was placed through the right superior pulmonary vein. The aorta was

Figure 1. Chest radiography showing infiltrations in both the lower lung zones, suggesting right-side heart enlargement.
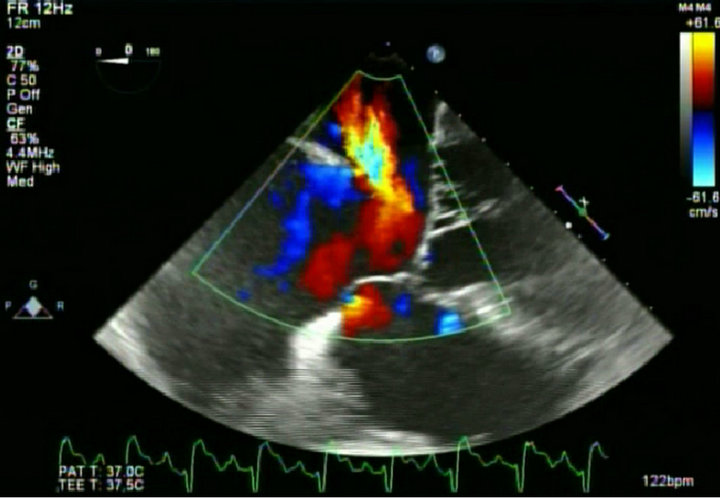
Figure 2. Transesophageal echocardiography showing a large ostium primum atrial septal defect.
cross-clamped, and only antegrade cardioplegia was administered throughout the operation. The patient’s body was cooled to 32˚C. Oblique right atriotomy was performed. A large mitral valve cleft was identified through a large ostium primum ASD. However, no ventricular septal defect was identified. Initial water test showed central MR and central tricuspid regurgitation. Mitral cleft was carefully and evenly closed with multiple 5 - 0 Ticron interrupted sutures. Central regurgitation remained after cleft closure. To reduce chordal tension, posterior annuloplasty was performed with 2 - 0 Ticron plication sutures reinforced with an autologous pericardial strip (Figure 3). A mild central regurgitation remained, however. Finally, Alfieri’s technique was used with 4 - 0 pledgeted monofilament sutures in the middle of the leaflet. Final water test showed no regurgitation. Then, a large piece of bovine pericardial sheet was cut in the form of a square. The initial suture was started in the middle of the ventricular septal crest between the left and right AV valve with 4 - 0 monofilament, and suturing was continued toward the surgeon’s right. Special care was needed to avoid picking up the conduction pathway and tricuspid septal valve leaflet. Suturing was continued leaving the coronary sinus ostium in the natural anatomical side (i.e., right atrial side). The lateral side of the septal defect was quickly sutured. Water test showed no regurgitation of the tricuspid valve. The right atrium was closed with a 4-0 monofilament suture. A de-airing maneuver was carefully conducted. The aorta was then declamped. Cardiopulmonary bypass was quickly weaned off, and a normal hemodynamic state was slowly restored. No blood transfusion was needed during the procedure.
The patient was extubated 7 h after the operation and required inotropic support for a further 3 days. AFL and atrial fibrillation were detected on postoperative day 2, but sinus rhythm spontaneously returned on postoperative day 4. He was discharged 13 days postoperatively without any other complications. At 6 months after surgery, he remains in good health, free from any major cardiac event, trivial MR, and no mitral stenosis (MS) on TTE (Figures 4(a) and (b)). His sinus rhythm remains stable.
3. Discussion
Partial AV septal defect is an extremely rare condition. It is widely recognized as a prognostic factor in the progress of arrhythmias, such as atrial fibrillation, complete AV block, sick sinus syndrome, and ventricular tachycardia, which are the most common causes of deterioration and frequently occur with increasing age [1]. Conditions for long-term survival include 1) mild valve dysfunction; 2) maintenance of sinus rhythm and absence of arrhythmias; 3) mild cardiac dysfunction, including late onset of heart failure; and 4) none or other simple car-

Figure 3. Operative findings. Sutured mitral valve cleft (arrow), tricuspid valve (arrowhead).
 (a)
(a) (b)
(b)
Figure 4. Transthoracic echocardiography showing (a) no ventricular septal defect and mitral stenosis and (b) no left-to-right shunt at the right atrium, at 1 week after the operation.
diac anomaly. Furthermore, the survival rate of complete AV septal defect patients over 50 years of age in their natural histories is only 1.8% - 3.6%, and 18.5% for partial AV septal defect [2]. In recent years, low surgical mortality has been reported even in elderly patients [3-6]. Thus, we suggest that partial AV septal defect is an operation indication when its diagnosis is established regardless of the presence of arrhythmias or heart failure.
It is well known that partial AV septal defect has concomitant valve dysfunction, usually MR due to mitral valve cleft. Most surgeons probably attempt mitral valve repair first for MR. The objective is to create an adequate coaptation zone by suturing the cleft to reduce the regurgitation orifice and mitral annular plication where strut chordae are close together [2]. In the case of mitral valve cleft, however, the distance of both papillary muscles is relatively closer than in a normal mitral valve [7]. Surgeons must not insist on mitral valve repair to reduce residual MR to lower than moderate level because it is most important to not cause postoperative MS. Hence, we took meticulous care during mitral valve repair although we added Alfieri’s method to reduce residual MR. Postoperative TTE showed trivial MR, and deceleration time (DT) was 220 msec, with an estimated mitral valve area (MVA) of 3.45 cm2 (Formula; MVA = 759/DT). The patient does not currently exhibit MS, but we must continuously follow up on his mitral valve function.
Successful repair of partial AV septal defect demands understanding for accurate location and course of the AV conduction. A previous study reported that the AV node is displaced posteroinferiorly from the apex of the traingle of Koch [7]. In the present case, the initial suture was started in the middle of the ventricular septal crest between the left and right AV valves. Suturing was continued to the edge of the coronary sinus ostium in the natural anatomical side (i.e., right atrial side) to avoid conduction injury. The AV block was not detected postoperatively. Hence, we believe that this suture was appropriate in this case.
4. Conclusion
This report describes a very rare case of successful repair of a partial AV septal defect combined with MR in an adult. We suggest that an anatomical understanding described here is essential to achieving a good result in this type of operation.
REFERENCES
- S. Asano, H. Murayama, Y. Okada, T. Sezaki, Y. Nakagawa and K. Tatsuno, “Successful Surgical Correction for an Incomplete Endocardial Cushion Defect in an Elderly Patient,” The Japanese Association for Thoracic Surgery, Vol. 46, No. 11, 1998, pp. 1172-1176.
- A. Takazawa, A. Shiikawa, S. Aomi, H. Nishida, M. Endo and H. Koyanagi, “Successful Surgical Correction of Endocardial Cushion Defect in a 63-Year-Old Female Patient,” The Japanese Association for Thoracic Surgery, Vol. 39, 1991, pp. 1960-1965.
- K. H. John, J. T. Abdul, B. S. James and C. M. Dwight, “Partial Atrioventricular Canal Defect in Elderly Patients (Aged 60 Years or Older),” The American Journal of Cardiology, Vol. 50, No. 8, 1982, pp. 59-62. doi:10.1016/0002-9149(82)90009-1
- K. H. John, J. T. Abdul, B. S. James, F. Valentin, G. R. Donald, O. B. Robert, et al., “Partial Atrioventricular Canal Defect in Adults,” Circulation, Vol. 66, No. 2, 1982, pp. 284-287. doi:10.1161/01.CIR.66.2.284
- L. Laszio, S. Gyorgy, K. Imre and L. Maria, “Late Results after Repair of Partial Atrioventricular Septal Defect in Adolescents and Adults,” Texas Heart Institute Journal, Vol. 19, No. 4, 1992, pp. 265-269.
- A. G. Michael, H. G. Sloane and G. W. William, “Surgery for Partial Atrioventricular Septal Defect in the Adult,” The Annals of Thoracic Surgery, Vol. 67, 1999, pp. 504-510. doi:10.1016/S0003-4975(98)01137-0
NOTES
*Corresponding author.

