Advances in Infectious Diseases
Vol.4 No.2(2014), Article
ID:46628,6
pages
DOI:10.4236/aid.2014.42014
The Diagnostic Value of H Formula to Predict Mortality in Hospitalized Patients with Infectious Diseases
Ali Akbar Heydari, Khosro Mohammadi, Saied Akhlaghi, Arash Arianpoor
Research Center for Infection Control & Hand Hygiene, Mashhad University of Medical Sciences, Mashhad, Iran
Email: heydariaa@mums.ac.ir
Copyright © 2014 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/



Received 7 March 2014; revised 7 April 2014; accepted 17 April 2014
ABSTRACT
The ability to identify patients with risk of mortality in the initial stages allows us to introduce a more aggressive treatment in order to improve patients’ survival. In this study, we used systemic inflammatory response syndrome (SIRS) criteria, respiratory and heart rate per minute, and consciousness level [(Glasgow coma scale (GCS)] to develop a formula to predict death in patients admitted to the Infectious Diseases ward of Imam Reza hospital. Methods: This descriptive study was a cross sectional study done in the Infectious Diseases ward of Imam Reza hospital, Mashhad University of Medical Sciences, Iran. Alive and dead patients between the dates September 1, 2006 to September 1, 2007 were studied. In this study, data such as past medical history, prescribed drugs and their administration by nursing and medical staff was extracted from patients’ files. Also, the time of death, the first vital signs recorded in the hospital and the formula H = (PR + RR) − GCS (respiratory rate per minute plus heart rate per minute minus Glasgow coma scale (GCS)) was calculated for both alive and dead patients. Data was analyzed by SPSS software. Mann-Whitney test, Roc Curve, and logistic regression model were used for data analysis. Results: The total number of admitted patients was 1007 of whom 90 (10.82%) died. One patient was excluded from the study. Out of 90 dead patients, 51 (56.6%) were male and 39 (43.3%) were female. There was no significant difference between the two groups regarding the gender (P > 0.05). The mean age of the study group (deceased) was 59 ± 21 and the mean age of the control group (alive) was 58 ± 21. The Mann-Whitney test showed that the result of H Formula was significantly different between the two groups, (126 ± 26 for the study group and 111 ± 22 for the control group). The cutoff for H Formula was equal to 112.5. Negative and positive predictive values, specificity and sensitivity were 0.85, 0.35, 0.57, and 0.70 respectively. Logistic regression results show that the H index contents independently affected the mortality of infected patients. Conclusion: With regard to the importance of measuring vital signs in diagnosis and determining the mortality in patients with infectious disease, the H (Heydari) formula can be valuable for evaluation and determination of mortality risk and consequently, early intervention. Patients with severe tachycardia, severe tachypnea and altered mental status that cannot be properly and quickly improved within 2 hours after admission via hydration and other measures are at higher risk of mortality.
Keywords:Mortality, Prediction, Infectious Disease, H Formula, Vital Signs

1. Introduction
Infections are among the major determinants of prognosis and outcome of hospitalized patients, especially who are severely ill and need intensive care. Patients with prolonged stays in intensive care unit (ICU) and patients who have predisposing risk factors, such as diabetes, anemia, malignancies, leukopenia, cirrhosis or severe alcoholism are at higher risk of developing nosocomial infections [1] .
Early systemic responses to infection, such as tachycardia, tachypnea, leukocytosis and fever, are used to define a systemic inflammatory response syndrome (SIRS). To be precise SIRS is defined as the presence of at least two of the following: 1) Fever (temperature > 38˚C) or hypothermia (temperature < 36˚C), 2) Tachycardia (i.e. pulse rate > 90 beats/min), 3) Tachypnea (i.e. respiratory rate > 20 breaths/min) or PaCO2 < 32 torr and 4) Leukocytosis (White Blood Cell count > 12,000/mm3), leukopenia (WBC count < 4000/mm3) or bandemia (i.e. presence of greater than 10% immature band forms) [2] . Presentation of symptoms of SIRS along with confirmed or suspected infection in a patient is considered as sepsis [3] . It should be noted that the definition of sepsis would not unescapably imply the existence of hemodynamic comprise or a bacterial cause [4] .
Severe sepsis is another term which is defined by presence of sepsis along with organ dysfunctions that can be described as acute lung injury, coagulation abnormalities, thrombocytopenia, altered mental status, renal failure, cardiac failure, liver failure or hypoperfusion with lactic acidosis [5] . Septic shock, a more severe condition, is defined as the presence of sepsis together with unresponsive hypotension (systolic blood pressure < 90 mmHg, mean arterial pressure < 65 mmHg or a 40 mmHg drop in systolic BP compared to baseline) [4] .
Recognizing the historical, clinical and laboratory findings which are suggestive of infection, organ dysfunction and hypoxia is a necessity in order to diagnose severe sepsis and septic shock as early as possible. In that manner, both epidemiologic and patient risk for infection must be assessed. Many factors increase the risk of infection including the immunocompromising states and prosthetic devices such as intravenous lines, heart valves and urinary catheters. The hallmark of infection is fever and it should be noted that generally the elderly and patients who have myocardial dysfunction and shock tend to have lower temperatures than younger adults [4] .
As the sepsis and SIRS criteria, mentioned above, involve certain laboratory value abnormalities, various test are suggested when severe infection is suspected. These tests include a CBC count with the differential and standard chemistry panel (including bicarbonate, creatinine, liver enzymes, lactate and coagulation studies) [6] .
As mentioned before, severe sepsis and systemic inflammatory response syndrome (SIRS) are key causes of mortality in patients. Therefore, the ability to diagnose and treat the affected patients may decrease mortality rate [4] [7] -[11] . SIRS criteria and routine tests, such as the white blood cell (WBC) count are nonspecific and are not useful in septic patients. New sepsis biomarkers such as procalcitonin, are currently being evaluated [12] . In the present study, we calculated a new valuable formula to predict the risk of mortality in infectious patients.
2. Patients and Methods
2.1. Study Population
This cross-sectional descriptive study was performed during 2006-2007, in the Infections Disease ward of Imam Reza Hospital, Mashhad University of Medical Science. Information was extracted from patient files. Patient histories, prescribed drugs and their administration by the nursing and medical staff were studied.
2.2. Sampling and Sample Size
The study was performed on 1007 patients. Ninety (10.82%) of these patients had died during their hospital stay during September 1 2006 to September 1 2007. Two hundred and seventy of the patients, who were admitted to the Infectious Disease ward at the same time and discharged in good health, were assigned as our control group.
2.3. Calculation of H Formula
The H Formula consists of three components: 1) Pulse rate per minute (PR), 2) Respiratory rate per minute and 3) Glascow Coma Scale (GCS) and is calculated as follows:
H = (PR + RR) – GCS In this inquiry we calculated the H Formula for both study and control groups.
2.4. Statistical Analysis
Mean age (and standard deviation) were calculated for all study groups. P-value was calculated using the student t-test. We compared the P-value for H Formula between the study and control group using the Mann-Whitney test. After determining the cutoff point for H index, we drew the ROC curve model to predict mortality.
Two-sided P-values below 0.05 were considered as statistically significant. We used SPSS (version 11.5) software for all statistical analyses.
3. Results
Total patients who died after admission to the Infectious Diseases ward of Imam Reza hospital during our study period were studied. Of the 90 dead patients, 51 (56.6%) were male and 39 (43.3%) were female. According to the Mann-Whitney test, there was a significant difference between the calculated H Formula in the study (126 ± 26) and the control group (111 ± 22). The cutoff point for H Formula according to the ROC curve was 112.5.
Sensitivity, specificity and positive and negative predictive values were calculated (Table 1).
All of the variables that had a significant relation with mortality were entered into the logistic regression model and the result showed that H Formula is an independent predictive factor of mortality (odds ratio (OR) = 0.95 and 95% confidence interval (CI) = 0.19 − 0.981) (Figure 1).
Table 1. Value of H Formula to predict mortality in hospitalized infectious disease patients.
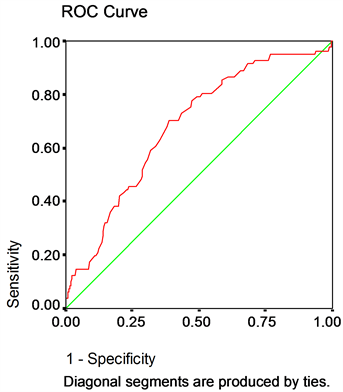
Figure 1. The Rock curve to determine the cutoff point of H Formula.
4. Discussion
Several studies have found that abnormalities in heart rate characteristics that were measured using spectral analysis, precede (in neonates) or coincide with (in adults) [13] [14] the onset of septic shock, and these abnormalities may predict in-hospital mortality in some settings [15] [16] . They may reflect an uncoupling of biologic oscillations in heart rate, blood pressure, respiration, and other functions that are normally connected through neural networks [17] [18] . Hyperventilation with respiratory alkalosis can be one of the earliest manifestations of sepsis. Similarly, pulmonary dysfunction typically occurs early in the course of severe sepsis. In a study conducted by Rangel-Frausto, 71% of the patients developed severe sepsis, sepsis, or SIRS [19] . Severe sepsis and septic shock is associated with case-fatality rate of approximately 30% and 50%. As initially noted by McCable, and Jackson [20] , the outcome is significantly (and most profoundly) influenced by the patient’s underlying diseases [21] [22] . Confusion and other alterations in higher cerebral function are often early manifestations of severe sepsis, particularly in older adults, and it should be noted that the severity of these changes has been found to correlate with the overall severity of illness [23] . Prognostic scores based on bedside evaluations such as the APACHE II, Simplified Acute Physiology Score (SAPS II), and the sequential organ failure assessments (SOFA) are more appropriate measurements in the usual ICU setting, although their mortality predictions differ substantially [24] [25] . The early systemic responses to infection, such as tachycardia, fever, tachypnea, leukocytosis or leucopenia can be used to define SIRS. When SIRS occurs in a patient with proven or suspected infection it is called sepsis.
Early diagnosis and treatment of patients with sepsis is important for saving their lives (8). There is also considerable inter-individual and time-dependent variability in the expression of the body’s response to infection, so it is not possible to provide a diagnostically useful “profile” of laboratory tests [11] . In 2003, Shapiro et al. predicted a 28-day mortality rate in hospitalized patients, considering determinants such as terminal disease, hypoxemia (PaO2/FIO2 < 300), tachypnea, septic shock, a platelet count <150,000 mm3, band cell > 5%, age > 65 years, pneumonia, being a long care facility resident and altered mental status [26] . In 2010, Jabalameli et al. evaluated the correlation of SIRS with mortality and morbidity in critically ill obstetric patients in the ICU and reported that higher incidence of SIRS in these patients is associated with increasing morbidity [27] . In another inquiry which we performed in 2007, the sensitivity of SIRS in predicting the mortality of patients with infectious disease was 41% [28] .
One of the limitations in our study is that due to high workload in our emergency department, the initial vital signs of patients at the time of admission may not be accurately recorded. In spite of this disadvantage, the H Formula calculated based on these vital signs showed good sensitivity and specificity.
5. Conclusion
According to our experience in infectious diseases department, patients with tachycardia, severe tachypnea and altered mental status, which are not properly and quickly (within 2 hours after admission) curable by hydration and other measures, are at higher risk of mortality. We obtained a valuable formula (H = (PR+ RR) – GCS) for the evaluation and determination of death risk.
Acknowledgements
This research was financially supported by a grant provided by the chancellor for research of the Mashhad University of Medical Science, Mashhad, Iran.
We would like to thank Mr. Emran Askari for his time in commenting on our paper and the personnel of Medical Archives of Imam Reza Hospital.
References
- Zarei, M.-R., Dianat, S., Eslami, V., Harirchi, I., Boddouhi, N., Zandieh, A., et al. (2011) Factors Associated with Mortality in Adult Hospitalized Burn Patients in Tehran. Ulus Travma Acil Cerrahi Derg, 17, 61-65. http://dx.doi.org/10.5505/tjtes.2011.22129 Bone R.C., Balk, R.A., Cerra, F.B., Dellinger, R.P., Fein, A.M., Knaus, W.A., et al. (1992) Definitions for Sepsis and Organ Failure and Guidelines for the Use of Innovative Therapies in Sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest Journal, 101, 1644-1655. http://dx.doi.org/10.1378/chest.101.6.1644 Morrell M.R., Micek, S.T. and Kollef, M.H. (2009) The Management of Severe Sepsis and Septic Shock. Infectious Disease Clinics of North America, 23, 485-501. http://dx.doi.org/10.1016/j.idc.2009.04.002 Nguyen H.B., Rivers, E.P., Abrahamian, F.M., Moran, G.J., Abraham, E., Trzeciak, S., et al. (2006) Severe Sepsis and Septic Shock: Review of the Literature and Emergency Department Management Guidelines. Annals of Emergency Medicine, 48, 54. Levy M.M., Fink, M.P., Marshall, J.C., Abraham, E., Angus, D., Cook, D., et al. (2003) 2001 SCCM/ESICM/ACCP/ ATS/SIS International Sepsis Definitions Conference. Intensive Care Medicine, 29, 530-538. http://dx.doi.org/10.1007/s00134-003-1662-x Cornbleet P.J. (2002) Clinical Utility of the Band Count. Clinics in Laboratory Medicine, 22, 101-136. http://dx.doi.org/10.1016/S0272-2712(03)00069-6 Sankoff J.D., Goyal, M., Gaieski, D.F., Deitch, K., Davis, C.B., Sabel, A.L., et al. (2008) Validation of the Mortality in Emergency Department Sepsis (MEDS) Score in Patients with the Systemic Inflammatory Response Syndrome (SIRS). Critical Care Medicine, 36, 421-426. http://dx.doi.org/10.1097/01.CCM.0B013E3181611F6A0
- Rivers E., Nguyen, B., Havstad, S., Ressler, J., Muzzin, A., Knoblich, B., et al. (2001) Early Goal-Directed Therapy in the Treatment of Severe Sepsis and Septic Shock. New England Journal of Medicine, 345, 1368-1377. http://dx.doi.org/10.1056/NEJMoa010307
- Annane D., Sébille, V., Charpentier, C., Bollaert, P.-E., François, B., Korach, J.-M., et al. (2002) Effect of Treatment with Low Doses of Hydrocortisone and Fludrocortisone on Mortality in Patients with Septic Shock. JAMA, 288, 862-871. http://dx.doi.org/10.1001/jama.288.7.862
- Van Den Berghe G., Wouters, P., Weekers, F., Verwaest, C., Bruyninckx, F., Schetz, M., et al. (2001) Intensive Insulin Therapy in Critically Ill Patients. New England Journal of Medicine, 345, 1359-1367. http://dx.doi.org/10.1056/NEJMoa011300 Bernard G.R., Vincent, J.-L., Laterre, P.-F., LaRosa, S.P., Dhainaut, J.-F., Lopez-Rodriguez, A., et al. (2001) Efficacy and Safety of Recombinant Human Activated Protein C for Severe Sepsis. New England Journal of Medicine, 344, 699-709. http://dx.doi.org/10.1056/NEJM200103083441001 Talan D.A., Moran, G.J. and Abrahamian, F.M. (2008) Severe Sepsis and Septic Shock in the Emergency Department. Infectious Disease Clinics of North America, 22, 1-31. http://dx.doi.org/10.1016/j.idc.2007.09.005 Griffin M.P. and Moorman, J.R. (2001) Toward the Early Diagnosis of Neonatal Sepsis and Sepsis-Like Illness Using Novel Heart Rate Analysis. Pediatrics, 107, 97-104. http://dx.doi.org/10.1016/j.idc.2007.09.005 Griffin M.P., O’Shea, T.M., Bissonette, E.A., Harrell, F.E., Lake, D.E. and Moorman, J.R. (2003) Abnormal Heart Rate Characteristics Preceding Neonatal Sepsis and Sepsis-Like Illness. Pediatric Research, 53, 920-926. http://dx.doi.org/10.1203/01.PDR.0000064904.05313.D2 Annane D., Trabold, F., Sharshar, T., Jarrin, I., Blanc, A.S., Raphael, J.C., et al. (1999) Inappropriate Sympathetic Activation at Onset of Septic Shock: A Spectral Analysis Approach. American Journal of Respiratory and Critical Care Medicine, 160, 458-465. http://dx.doi.org/10.1164/ajrccm.160.2.9810073 Chen W.L., Chen, J.H., Huang, C.C., Kuo, C.D., Huang, C.I. and Lee, L.S. (2008) Heart Rate Variability Measures as Predictors of In-Hospital Mortality in ED Patients with Sepsis. The American Journal of Emergency Medicine, 26, 395-401. http://dx.doi.org/10.1016/j.ajem.2007.06.016 Seely A.J. and Christou, N.V. (2000) Multiple Organ Dysfunction Syndrome: Exploring the Paradigm of Complex Nonlinear Systems. Critical Care Medicine, 28, 2193-2200. http://dx.doi.org/10.1097/00003246-200007000-00003 Godin P.J. and Buchman, T.G. (1996) Uncoupling of Biological Oscillators: A Complementary Hypothesis Concerning the Pathogenesis of Multiple Organ Dysfunction Syndrome. Critical Care Medicine, 24, 1107-1116. http://dx.doi.org/10.1097/00003246-199607000-00008 Rangel-Frausto M.S., Pittet, D., Costigan, M., Hwang, T., Davis, C.S. and Wenzel, R.P. (1995) The Natural History of the Systemic Inflammatory Response Syndrome (SIRS): A Prospective Study. JAMA, 273, 117-123. http://dx.doi.org/10.1001/jama.1995.03520260039030 McCabe W.R. and Jackson, G.G. (1962) Gram-Negative Bacteremia: I. Etiology and Ecology. JAMA Internal Medicine, 110, 847-855. http://dx.doi.org/10.1001/archinte.1962.03620240029006 Bates D.W., Pruess, K.E. and Lee, T.H. (1995) How Bad Are Bacteremia and Sepsis? Outcomes in a Cohort with Suspected Bacteremia. JAMA Internal Medicine, 155, 593-598. http://dx.doi.org/10.1001/archinte.1995.00430060050006 Perl T.M., Dvorak, L., Hwang, T. and Wenzel, R.P. (1995) Long-Term Survival and Function after Suspected GramNegative Sepsis. JAMA, 274, 338-345. http://dx.doi.org/10.1001/jama.1995.03530040066043 Sharshar T., Hopkinson, N.S., Orlikowski, D. and Annane, D. (2005) Science Review: The Brain in Sepsis-Culprit and Victim. Critical Care, 9, 37-44. http://dx.doi.org/10.1186/cc2951 Friedland J.S., Porter, J.C., Daryanani, S., Bland, J.M., Screaton, N.J., Vesely, M.J., et al. (1996) Plasma Proinflammatory Cytokine Concentrations, Acute Physiology and Chronic Health Evaluation (APACHE) III Scores and Survival in Patients in an Intensive Care Unit. Critical Care Medicine, 24, 1775-1781. http://dx.doi.org/10.1097/00003246-199611000-00003 Vincent J.L., De Mendonça, A., Cantraine, F., Moreno, R., Takala, J., Suter, P.M., Sprung, C.L., Colardyn, F. and Blecher, S. (1998) Use of the SOFA Score to Assess the Incidence of Organ Dysfunction/Failure in Intensive Care Units: Results of a Multicenter, Prospective Study. Critical Care Medicine, 26, 1793-1800. http://dx.doi.org/10.1097/00003246-199811000-00016 Shapiro N.I., Wolfe, R.E., Moore, R.B., Smith, E., Burdick, E. and Bates, D.W. (2003) Mortality in Emergency Department Sepsis (MEDS) Score: A Prospectively Derived and Validated Clinical Prediction Rule. Critical Care Medicine, 31, 670-675. http://dx.doi.org/10.1097/01.CCM.0000054867.01688.D1 Jabalameli M. (2012) Evaluating the Correlation of Systemic Inflammatory Response Syndrome with Mortality and Morbidity in Critically Ill Obstetric Patients in ICU. Qom University of Medical Sciences Journal, 4, 37-41. Heydari A. and Ghabouli, M. (2007) The Relationship between Severity of the Systemic Inflammatory Response Syndrome (SIRS) and Its Etiology and Outcome. Medical Journal of Mashhad University of Medical Sciences, 50, 321- 326.


