World Journal of Cardiovascular Diseases
Vol.4 No.5(2014), Article ID:45642,11 pages DOI:10.4236/wjcd.2014.45030
Radial Applanation Tonometry as an Adjuvant Tool in the Noninvasive Arterial Stiffness and Blood Pressure Assessment
Lucas José Sá da Fonseca1, Marco Antônio Mota-Gomes2, Luíza A. Rabelo1,3*
1Laboratório de Reatividade Cardiovascular, Setor de Fisiologia e Farmacologia, Instituto de Ciências Biológicas e da Saúde, Universidade Federal de Alagoas, Maceió, Brazil
2Centro de Pesquisas Clínicas do Hospital do Coração de Alagoas—HCOR-AL, Maceió, Brazil
3Max-Delbrück-Center for Molecular Medicine, Berlin, Germany
Email: *luizaa.rabelo@gmail.com, *luiza.rabelo@icbs.ufal.br
Copyright © 2014 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/


Received 12 March 2014; revised 14 April 2014; accepted 23 April 2014
Abstract
Since antiquity, the human arterial pulse represents an important parameter in the clinical assessment. Besides being routinely assessed in the medical practice, such pulse is not observed in its completeness yet, once many of the data obtained through it cannot be evaluated using conventional methods. Taking into account such methods, the measurement of arterial blood pressure using sphygmomanometry, although broadly widespread in the assessment and follow-up of patients who require accompaniment of their cardiovascular status, is not able to properly guide about parameters related to the central hemodynamic status, the latter most strongly associated with cardiovascular risk. Such incapability is due to the centrifugal augmentation of the pressures taken at different points of the arterial bed, based on the properties of the closed arterial system through which the blood flow travels. In this context, methodologies capable of assessing central parameters estimated using the pulse wave analysis, such as applanation tonometry, represent a promising adjuvant for evaluating patients with cardiovascular diseases, by providing detailed information concerning hemodynamic parameters otherwise inaccessible. In this scenario, the present review focuses on the applanation tonometry and its assessment on the radial artery, highlighting the importance of this method in the cardiovascular assessment, as well as its relevance in the clinical practice, when determining parameters peripherally obtained capable of estimating the central hemodynamic status.
Keywords:Arterial Pulse, Arterial Stiffness, Noninvasive Assessment, Radial Tonometry, Cardiovascular Risk

1. Introduction
“All we know is still infinitely less than all that remains unknown.”—William Harvey.
Historically, many civilizations associated the changes in the patterns of the arterial pulse with pathological conditions [1] . In this sense, the interpretation of such pulse represented an important propaedeutic tool for Chinese, Indian, Greek and Roman physicians, who used to explore the irregularity of the arterial pulse in the diagnostic assessment [1] [2] . The Greek physician Galen, for example, had already described 27 different varieties of pulse [2] , being the assessment of the human arterial pulse as old as the Egyptian papyri, with references to the pulse examination dating back to 1600 BC [3] , and the modern records being initiated in 1860, after the construction of the sphygmograph by Jules Marey [3] [4] (Figure 1).
In 1872, Frederick Akbar Mahomed, while describing the development of methods for recording the arterial pulse, highlighted that “Since the information which the pulse affords is of so great importance, and so often consulted, surely it must be to our advantage to appreciate fully all it tells us, and to draw from it every detail that it is capable of imparting” (apud O’Rourke et al., 2001 [5] ; O’Rourke & Adji, 2008 [6] ). More interestingly, despite the simplicity with which Marey and Mahomed registered the pulse waves, their records are surprisingly similar to those observed when using high technology devices currently available [2] .
In this scenario, increasing attention has been given to the importance of the arterial stiffness in the development of cardiovascular diseases, emphasizing hypertension, prediction of target organ damage and cardiovascular mortality [7] -[13] , with the development of different devices increasingly sophisticated for this purpose [4] [14] -[17] (Figure 2). By allowing the pulse wave analysis, such devices help to recognize the clinical relevance of the aforementioned stiffness [18] [19] . Instead of being considered innovations in the field of the vascular function assessment, such devices represent the reintroduction, with substantial upgrading, of the pulse wave analysis so broadly present in the clinical practice since last century [6] . Thus, the use of these methodologies affords the diagnosis of vascular impairment even before the onset of clinical manifestations of the related diseases [20] . In this context, the present review approaches some of the aspects related to the applanation tonometry, emphasizing the one performed in the radial artery, the meaning of its main parameters and its applicability in the clinical setting.
2. Applanation Tonometry: The Fundamentals
Among the different methods for assessing the vascular function, the applanation tonometry [“tonometry”—tono (from the Latin “tonus”): tension, stretch; metry (from the Greek, “métron”): measurement; “applanation”: flatten] is a noninvasive, reproducible and reliable technique [3] [21] [22] capable of providing estimated values concerning the central pressures. When considered the evaluation of hypertensive statuses, these parameters are presented, pathophysiologically and clinically, as more important variables [23] , once they constitute more accurate predictors of cardiovascular risk than peripheral pressures [3] [6] [24] . The reliability of this method is expressed by low intra and interobserver coefficients of variation for the measurement of the Augmentation In-
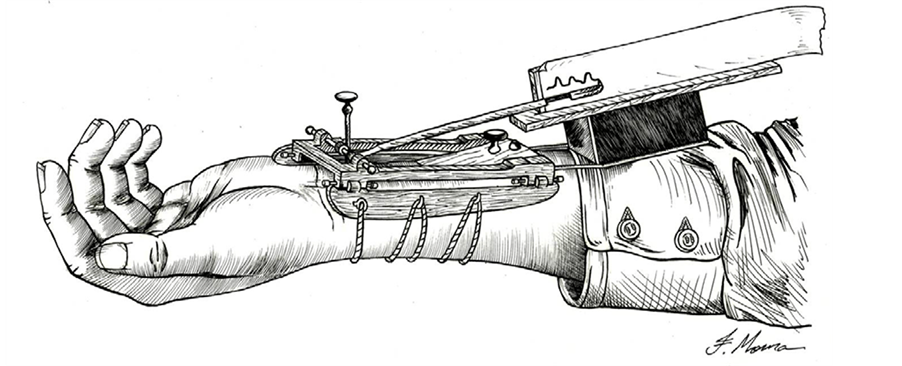
Figure 1. Sphygmograph developed by Etienne Jules Marey in 1860 (redesigned from Nelson et al., 2010).
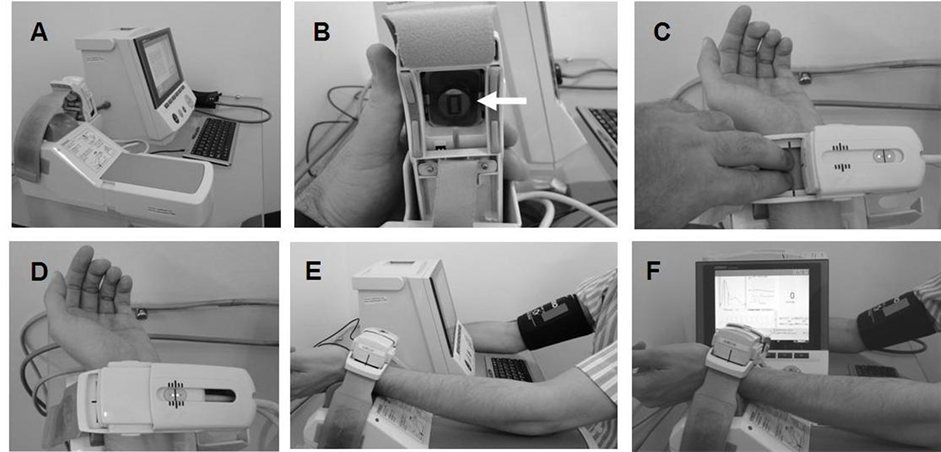
Figure 2. Representative sequence of the method of radial artery applanation tonometry. (A) Device for capturing the records; (B) microtransducer capable of identifying the pulse wave peripherally (arrow); (C) palpation of the left radial artery; (D) coupling of the tonometer on the radial anatomical correspondent; (E) positioning of the components in the upper limbs; (F) measurement of the pulse waves for determining the Augmentation Index (AI).
dex (AI), with values of 3.6% and 2.4%, respectively, ensuring its reproducibility [25] . The methodology of arterial applanation tonometry currently used is based on the technique of tonometry firstly applied in ophthalmology for measuring the intraocular pressure [26] , being the arteries flattened without the occurrence of vascular occlusion [27] .
The greater reliability provided by applanation tonometry comes from the fact that pressures obtained by assessing the brachial artery, using the conventional method of sphygmomanometry, are not effective in estimating the intraaortic pressure, particularly the central systolic pressure and the central pulse pressure [28] . Concerning this issue, the tonometry, in the evaluation of the anti-hypertensive response, is equally relevant. In fact, even though evoking similar reductions in blood pressure levels assessed by brachial artery, different associations of anti-hypertensive pharmaceuticals promote distinct reductions in blood pressure levels when evaluated the central pressures [2] [3] [28] [29] . Such observations reinforce the relevance of considering the central measures when it comes to the therapeutic response in the clinical management of hypertension [29] .
The principle of the applanation tonometry is based on the observation of the hemodynamic properties identified along the arterial tree [3] [23] . During the cardiac cycle, two waves are observed: the ejection wave, originated after systole, and the reflected wave, due to blood return through the peripheral vascular system at the end of systolic contraction (Figure 3). In this sense, the pressure registered at any point of the arterial system results from the sum of the ejection and reflected waves, depending on three factors: 1) the amplitude of ventricular ejection, 2) the duration of ventricular ejection, and 3) the velocity of the reflected wave from periphery [3] [30] . The pressure of the reflected wave represents an important evaluative parameter, as this pressure obtained by the assessment of the radial artery is associated with the aortic systolic blood pressure [2] .
Also, the increase in the central pressure may be quantified by the pressure added to the peak of systolic pressure based on the reflected wave, the so-called Augmentation Pressure (Figure 3). Equationally, the ratio between the reflected wave (P2) and the ejection wave (P1) is defined as the Augmentation Index (AI) [3] [20] [31] -[34] . The latter represents an indirect measure of systemic arterial stiffness [35] [36] (Figure 3), initially described as a parameter associated to the ventricular-vascular coupling [1] capable of providing complementary information while assessing the cardiovascular risk [37] . Considering that the reflected wave represents the numerator for calculating the AI (Figure 3), it is possible to conclude that increases in the Augmentation Pressure imply increases in the AI values, the latter expressed in percentage in relation to the pulse pressure. Thus, the greater the percentage values obtained, the greater the arterial stiffness and, consequently, the vascular impairment [7] [30] [36] [38] -[42] .
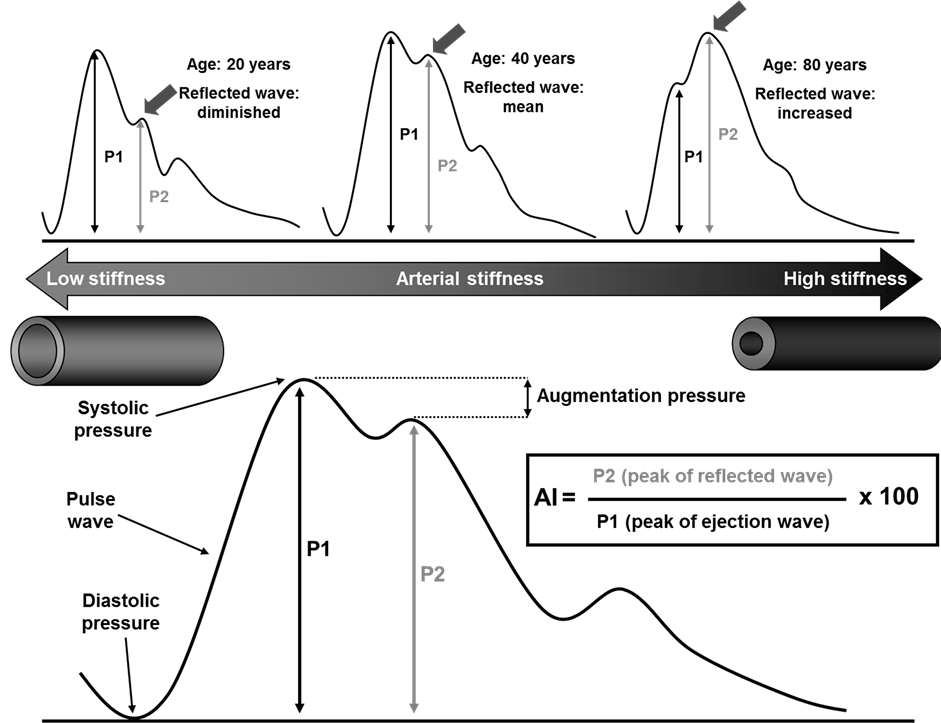
Figure 3 Representative scheme of the variables which determine the Augmentation Index (AI). With the advance of age, it is observed an increase in such index. Once the reflected wave (P2) is placed in the numerator of the ratio for calculating the AI, the greater the reflected wave, the higher the AI, ultimately leading to augmented arterial stiffness. Although it is expected the increase in the AI with ageing, this process of vascular ageing may be accelerated in the presence of cardiovascular risk factors. Adapted from Mota-Gomes et al., 2006.
3. Local Noninvasive Arterial Assessment, Its Systemic Significance, and Applicability as a Predictor of Cardiovascular Risk
The arterial mechanical properties play a relevant role in the maintenance of the arterial function, with innumerous variables capable of interfering in the vascular dynamics. Thus, the increase in the arterial stiffness, and consequently, the decreased vascular distensibility to the blood flow which comes with the ejection wave, augments the pulse wave. Such increase, in turn, promotes early return of the reflected wave [43] -[45] . This fact will imply an increment in the pulse pressure, augmentation pressure, ventricular afterload, with a reduction in diastolic pressure, ultimately leading to impairment in coronary perfusion, as in coronary circulation the arterial filling occurs in the diastole [43] .
The radial artery applanation tonometry allows to noninvasively and accurately assess the wave of central pulse pressure [3] [41] , by using transducers (micromanometers) (Figure 2(B), arrow) which continuously record the peripheral pulse waves [25] [46] , capturing changes of the intra-arterial pressure [26] . These tonometric sensors are able to detect the most pronounced pulse signals in the anatomy of the wrist, selecting the major amplitude among the recorded pulse waves [1] . Thus, these devices configure an important alternative for studying the arterial status [23] , once invasive procedures cannot be broadly used in the clinical setting [28] .
This noninvasive approach presents itself as more predictive for cardiovascular events related to hypertension than the peripheral blood pressure evaluated by the conventional method of sphygmomanometry [3] [47] . Such advantage comes from the fact that the AI derived from the radial artery presents a strong correlation with that identified in the aorta, with both indices bringing similar information [22] . Therefore, this observation allows to infer, by assessing peripheral data, about the condition in other vascular beds [48] [49] . Furthermore, the AI presents a positive correlation with coronary atherosclerosis and cardiovascular outcomes [50] . In this context, the index obtained from the radial artery may be used to identify patients with atherosclerotic disease [33] .
With regard to the vascular tonometry assessment, the anatomical location must be considered, once each vessel has a characteristic AI, being this one greater in the aorta than in the carotid arteries, and in these arteries, greater than in the radial arteries. Such capacity of a more refined evaluation, offered by the AI values, allows to obtain relevant data which cannot be assessed by using the conventional method of blood pressure measurement by sphygmomanometry in the brachial artery. According to this method, for example, it is not possible to distinguish between a normal pattern and a sustained pattern of vascular stress by the influence of the waves generated along the cardiac cycle, so that the data obtained by tonometry reflects both the degree of arterial damage and, consequently, a possible damage to cardiac function [15] .
Besides allowing the indirect assessment related to the atherosclerotic vascular impairment, the data obtained from tonometry enable to evaluate disturbances associated with the endothelial function [41] , because the AI is also described as an indicator of endothelial function [51] . This observation is of particular importance, once endothelial cells can, via release of specific molecules—among which the nitric oxide (–NO), the main vasorelaxing factor derived from the endothelium [52] , and vasoconstrictor factors, such as endothelin-1 [53] and prostaglandins [54] —modulate the arterial tone [55] [56] .
In reference to the evaluation of specific vascular beds, the applanation tonometry in the radial artery is anatomically easier, thanks to the fact that this artery rests on bone tissue [7] [46] . Technically, the segment of the anterior artery wall is easily flattened between the device and the distal part of the radius [6] [57] . Thus, this tonometric modality shows great advantage when compared to that used for the carotid assessment, mainly because in the latter, discomfort and difficulties may be observed while performing the procedure [25] . Furthermore, this vascular bed, for being located more internally in the neck, and circled by connective tissue, cannot be easily flattened [25] [58] . Moreover, for performing the carotid tonometry, it is also necessary to consider the interference of respiratory movements during the signal capture [25] , besides representing an exam which requires a highly trained professional for its execution [6] [22] [46] [58] [59] .
Still regarding the carotid arteries, risks exist during its applanation, once the procedure may induce bradycardia or even instability of atheromatous plaques [58] . The fact of not using the brachial artery tonometry, in turn, is based on the observation that this vessel is not firmly located in its anatomical territory, the reason why it could not be properly flattened because of its uncertain path along the humerus and the presence of the brachial aponeurosis, both of them representing direct interfering factors in the signal capture by the sensor [6] [58] .
For the graph representation of the arterial pulse, literature describes the existence of three distinct patterns of behavior: A, B and C [60] . The first one is characterized by an oscillatory pulse, and its main characteristic is the accentuated pulse wave reflection, as indicated in Figure 3 (superior graph, right side, representing the pulse wave of an 80-year-old individual). For the C pattern, it is observed a less oscillatory, more regular presentation, with minor and more diffuse reflection, according to the superior graph, left side in Figure 3 (record of a pulse wave in a 20-year-old individual). Finally, type B pattern for the pulse wave represents an intermediated point between the above mentioned extremes (Figure 3, graph from a 40-year-old individual) [60] .
Considering that the AI and the central pressure values represent indirect measures of the arterial stiffness [35] [36] , it is of note to highlight that they actually constitute auxiliary data in the vascular assessment, as the pulse wave velocity (PWV) is recognized as the gold standard for evaluating the arterial stiffness [18] [44] . Thus, the AI values and the PWV values are not interchangeable, so that the ones obtained from the AI should not be taken as identical surrogates for the PWV, but as adjuvant data in the pulse wave analysis instead [4] [21] . In this regard, in line with the description of a strong correlation between the AI and the PWV [21] , and the fact that some studies have shown central measures to be stronger predictors of cardiovascular risk than values peripherally obtained [3] [6] [24] , Vlachopoulos and colleagues (2010) [61] , in a meta-analysis studying the predictive role of central hemodynamics, did find that central hemodynamic values independently predict cardiovascular outcomes. In such study, however, the investigators observed that the AI is capable of predicting clinical events irrespective of peripheral pressures, with the central pulse pressure showing a marginally but not significantly predictive ability in comparison to the peripheral pulse pressure values. Finally, the authors reinforce the importance of conducting large-scale studies in order to better clarify the participation of these markers in the classification of cardiovascular disease risk.
Besides the advantages described, some limitations concerning the use of radial artery tonometry deserve to be pointed. Among them, appears the limited number of studies using this noninvasive method, compared to the greater number of clinical studies based on the use of blood pressure measurements in the brachial artery, as well as well as the lack of knowledge about this technique by health professionals [3] . Moreover, the use of methodologies for peripheral analysis, to further estimate central pressures, may require the application of transfer functions for properly converting and estimating values [23] [25] [28] . Such necessity arises from the greater stiffness in peripheral arteries when compared to the central ones, resulting in a process of centrifugal amplification even in healthy individuals, putting this assessment at risk of mistaken analysis [3] [7] [58] [62] . In this context, the evaluation of these transfer functions represents a relevant aspect to be considered while using the applanation tonometry.
4. Are Transfer Functions Imperative for Validating the Applanation Tonometry?
The arterial tonometry has become a useful means for noninvasively assessing the arterial properties by the use of transfer functions, the latter applied to estimate the central pressure by using variables obtained peripherally [63] . Based on mathematical methods, these functions represent specific algorithms in the programming of the devices used, enabling the indirect study of central parameters via analysis of different arterial beds, such as the radial, brachial or carotid arteries [64] . However, the applicability of these functions in the tonometric assessment has been questioned [25] , due to their validation in selected groups of patients [2] [7] [65] . In this context, after comparing the invasive and noninvasive evaluations in patients undergoing diagnostic angiography, Munir and colleagues (2008) [63] demonstrated that such functions are not necessarily required to estimate the systolic central pressure, once it is possible to perform this estimation by using the peripheral pulse wave. The results obtained by the authors suggest that the pressure of the late systolic shoulder of the peripheral arterial wave (a representation of the reflected wave from the periphery, with centripetal direction) is capable of estimating the central systolic blood pressure in a similar way to that observed during the use of transfer functions. However, the authors highlight that such estimation could only be reliably performed if the values obtained by the device were calibrated taking as reference invasive records.
Concerning the aforesaid calibration, many devices commercially available use transfer functions based on values obtained in patients who underwent invasive procedures (catheterization), ensuring the reproducibility and applicability of these methods [3] [28] , enabling, thus, to estimate central pressures by the use of peripheral noninvasive records [46] . Exemplifying this validation, in a study with a tonometric device, Takazawa and colleagues (2007) [25] compared values obtained by invasive assessments with those recorded in radial arteries. Interestingly, the authors demonstrated that the pressure of the reflected wave, noninvasively recorded by radial artery applanation tonometry, allows to assess the aortic central pressure as precisely as when using validated transfer functions. Furthermore, in the same study, it was evidenced a significant correlation between the aortic AI and the radial AI.
Methodologically, for the acquisition of more reliable values for the AI, it is important to consider the heart rate as one of the major influencing factors in the ventricular filling and, consequently, in the ejection wave [66] , being recommended the percentage values obtained to be normalized for a uniform heart rate of 75 beats per minute [1] [3] [5] [67] , as the augmentation increases with the reduction of heart rate, due to the increase in the period of ventricular ejection [5] .
Besides the heart rate, other parameters may influence the determination of the AI [67] . Physiologically, the reflected wave depends on the route developed by the blood flow, and in taller individuals, the arterial tree is bigger, so that the reflected wave appears later [38] . Thus, at any age and at any arterial segment considered, the augmentation is higher in individuals of short stature [5] . For this reason, it is also important to consider this anthropometric parameter during the acquisition of tonometric data. In this regard, some devices automatically include this variable in the vascular assessment by the use of processing algorithms obtained with linear equations, this way enabling such adaptation, with the possibility of designing, with graphical representations, the arterial status of an individual [59] [68] .
Still regarding the interference of others factors, literature also describes the direct relation between increases in the AI and ageing [5] [15] [37] (Figure 3), mainly due to histological changes in arterial components, with a marked reduction in elastin content in the media and its replacement by collagen, besides the increase in calcium deposition in the arterial wall [3] [47] . In this sense, unpublished data from our group based on the use of radial artery tonometry, point to the directly proportional relation between the advance of age and the increase in the AI values. Furthermore, different cardiometabolic disturbances, among which hypertension and diabetes [7] , importantly contribute to this negative profile, with the AI generally being negative in young individuals [1] .
5. From Theory to Practical Application: The Applanation Tonometry Protocol
The noninvasive assessment of the arterial function can be performed by applanation tonometry of the left radial artery (Figure 2), according to the protocol described by Mota-Gomes and colleagues (2006) [37] , using a validated device for this purpose [17] [25] .
Initially, the same care required for measuring the blood pressure is taken, in accordance with the VI Brazilian Guidelines for Hypertension (VI Diretrizes Brasileiras de Hipertensão, 2010) [69] , with the patient in sitting position, without being bent, free from previous intake of alcohol or coffee, resting for at least 5 minutes before measurement, the arm aligned with the thorax at heart level and free from clothes, and the elbow slightly flexed (Figure 2(E)). The cuff is then placed approximately 3 cm above the antecubital fossa, with the patient not being in the immediate postprandial period, and not presenting urinary content. Also, the legs should be kept uncrossed and, before measurement, the patient should be warned not to talk during the procedure.
Blood pressure levels are initially recorded by an oscillometric method in the right arm (Figure 2(E)). Before the measures for obtaining the AI could be performed, two blood pressure measurements are taken as reference, so that the sequence for evaluating the AI could only be done in the presence of pressure stability, the latter characterized by a difference of no more than 10 mmHg or no more than 5 mmHg for systolic and diastolic blood pressure, respectively. Once identified this stability, three consecutive measures are taken by the device, those that will enable the assessment of other tonometric parameters, among which the AI [37] .
For the analysis of the AI, the left arm is positioned on the support for the wrist, with the palpation of the left radial artery (Figure 2(C)). After its identification, the sensor is placed on its anatomical correspondent in the anterior side of the left wrist (Figure 2(D) and Figure 2(E)). For each patient, three measurements of the AI are taken (Figure 2(F)), and the standard deviation should not be greater than 10%, as higher values compromise the quality of the data obtained. For this parameter, as previously stated, increased percentage values are associated with low arterial elasticity [2] [4] [37] [52] . Besides the data concerning the AI, the device also informs about systolic blood pressure, diastolic blood pressure, pulse pressure, the pressure of the ejection wave and the pressure of the reflected wave [17] , allowing a detailed assessment of these cardiovascular parameters.
6. Conclusions
The criteria for noninvasively assessing cardiovascular variables using different methodologies, among which the radial artery applanation tonometry, have brought the notion that peripheral pressures, evaluated in the brachial artery, may not properly reflect the behavior of parameters related to the central pressures.
Indeed, based on the improvement of hemodynamic knowledge applied to the clinical assessment, current evidences show that alternative methodologies have become available, with a high degree of reliability. These approaches enable to early diagnose the vascular damage, also making possible a more accurate evaluation concerning the efficacy of the anti-hypertensive treatment. Finally, despite the fact that these proposals are not recent, it is possible to recognize the need to introduce these methods in the clinical setting, with major dissemination of its applicability, as a means for assessing useful parameters in the cardiovascular study and which are unavailable while using conventional evaluation methods.
Acknowledgements
The authors thank the physician Flávio Moura Rezende Filho (Scientific Initiation at the Laboratório de Reatividade Cardiovascular), for the elaboration of figure 1 of this manuscript, and the physiotherapist MSc. Glauber Schettino-Silva (Laboratório de Reatividade Cardiovascular, ICBS-UFAL), for helping with the images used to elaborate figure 2 of this manuscript.
Sources of Funding
This work was supported by grants from the Brazilian Ministry of Health/CNPq/SESAU-AL/FAPEAL (PPSUS- 2009 60030-695/2009), CNPq-Universal (483049/2009-3) and PROCAD-NF/CAPES (PROCAD-NF 2450/ 2008). Lucas José Sá da Fonseca received a Masters scholarship from CAPES (Programa de Pós-Graduação em Ciências da Saúde, ICBS-UFAL).
Conflict(s) of Interest/Disclosure(s)
None.
References
- Avolio, A.P., Butlin, M. and Walsh, A. (2010) Arterial Blood Pressure Measurement and Pulse Wave Analysis—Their Role in Enhancing Cardiovascular Assessment. Physiological Measurement, 31, R1-R47. http://dx.doi.org/10.1088/0967-3334/31/1/R01
- Palatini, P., Casiglia, E., Gasowski, J., Gluszek, J., Jankowski, P., Narkiewicz, K., Saladini, F., Stolarz-Skrzypek, K., Tikhonoff, V., Bortel, L., Wojciechowska, W. and Kawecka-Jaszcz, K. (2011) Arterial Stiffness, Central Hemodynamics, and Cardiovascular Risk in Hypertension. Vascular Health and Risk Management, 7, 725-739. http://dx.doi.org/10.2147/VHRM.S25270
- Nelson, M.R., Stepanek, J., Cevette, M., Cocalciuc, M., Hurst, R.T. and Tajik, A.J. (2010) Noninvasive Measurement of Central Vascular Pressures with Arterial Tonometry: Clinical Revival of the Pulse Pressure Waveform? Mayo Clinic Proceedings, 85, 460-472. http://dx.doi.org/10.4065/mcp.2009.0336
- Davies, J.I. and Struthers, A.D. (2003) Pulse Wave Analysis and Pulse Wave Velocity: A Critical Review of Their Strengths and Weaknesses. Journal of Hypertension, 21, 463-472. http://dx.doi.org/10.1097/00004872-200303000-00004
- O’Rourke, M.F., Pauca, A. and Jiang, X.-J. (2001) Pulse Wave Analysis. British Journal of Clinical Pharmacology, 51, 507-522. http://dx.doi.org/10.1046/j.0306-5251.2001.01400.x
- O’Rourke, M.F. and Adji, A. (2008) Basis for Use of Central Blood Pressure Measurement in Office Clinical Practice. Journal of the American Society of Hypertension, 2, 28-38. http://dx.doi.org/10.1016/j.jash.2007.08.006
- Laurent, S., Cockcroft, J., Bortel, L.V., Boutouyrie, P., Giannattasio, C., Hayroz, D., Pannier, B., Vlachopoulos, C., Wilkinson, I. and Struijker-Boudier, H., on the Behalf of the European Network for Non-invasive Investigation of Large Arteries (2006) Expert Consensus Document on Arterial Stiffness: Methodological Issues and Clinical Applications. European Heart Journal, 27, 2588-2605. http://dx.doi.org/10.1093/eurheartj/ehl254
- Qasem, A. and Avolio, A. (2008) Determination of Aortic Pulse Wave Velocity from Waveform Decomposition of the Central Aortic Pressure Pulse. Hypertension, 51, 188-195. http://dx.doi.org/10.1161/HYPERTENSIONAHA.107.092676
- Chen, W., Srinivasan, S.R. and Berenson, G.S. (2008) Differential Impact of Heart Rate on Arterial Wall Stiffness and Thickness in Young Adults: The Bogalusa Heart Study. Journal of the American Society of Hypertension, 2, 152-157. http://dx.doi.org/10.1016/j.jash.2007.10.008
- Grassi, G. and Borghi, C. (2008) Central Blood Pressure as Estimate of Cardiovascular Risk: Potentials and Limitations. Journal of Hypertension, 26, 16-17. http://dx.doi.org/10.1097/HJH.0b013e3282f465e3
- Schnabel, R., Larson, M.G., Dupuis, J., Lunetta, K.L., Lipinska, I., Meigs, J.B., Yin, X., Rong, J., Vita, J.A., NewtonCheh, C., Levy, D., Keany Jr., J.F., Vasan, R.S., Mitchell, G.F. and Benjamin, E.J. (2008) Relations of Inflammatory Biomarkers and Common Genetic Variants With Arterial Stiffness and Wave Reflection. Hypertension, 51, 1651-1657. http://dx.doi.org/10.1161/HYPERTENSIONAHA.107.105668
- Dengo, A.L., Dennis, E.A., Orr, J.S., Marinik, E.L., Ehrlich, E., Davy, B.M. and Davy, K.P. (2010) Arterial Destiffening with Weight Loss in Overweight and Obese Middle-Aged and Other Adults. Hypertension, 55, 855-861. http://dx.doi.org/10.1161/HYPERTENSIONAHA.109.147850
- Duprez, D.A. (2010) Arterial Stiffness and Endothelial Function: Key Players in Vascular Health. Hypertension, 55, 612-613. http://dx.doi.org/10.1161/HYPERTENSIONAHA.109.144725
- Cunha, R.S. (2004) Rigidez Arterial: Conceito e Implicações Metodológicas. Revista Brasileira de Hipertensão, 11, 152-156.
- Takazawa, K. (2005) Augmentation Index in Heart Disease. AJH, 18, 15S-18S.
- Wassertheurer, S., Mayer, C. and Breitenecker, F. (2008) Modeling Arterial and Left Ventricular Coupling for NonInvasive Measurements. Simulation Modelling Practice and Theory, 16, 988-997. http://dx.doi.org/10.1016/j.simpat.2008.04.016
- (2011) Omron Healthcare Europe B.V. http://www.omron-healthcare.com.sg/products_medicalprofessional_hem9000ai.htm
- Sugawara, J., Hayashi, K., Yokoi, T. and Tanaka, H. (2010) Carotid-Femoral Pulse Wave Velocity: Impact of Different Arterial Path Length Measurements. Artery Research, 4, 27-31. http://dx.doi.org/10.1016/j.artres.2009.11.001
- Vermeersch, S.J., Rietzschel, E.R., De Buyzere, M.L., Van Bortel, L.M., Gillebert, T.C., Verdonck, P.R., Laurent, S., Segers, P. and Boutouyrie, P. (2009) Distance Measurements for the Assessment of Carotid to Femoral Pulse Wave Velocity. Journal of Hypertension, 27, 2377-2385.http://dx.doi.org/10.1097/HJH.0b013e3283313a8a
- Malachias, M.V.B. (2004) A Rigidez Arterial como Marcador de Lesão no Presente e Preditor de Risco no Futuro. Revista Brasileira de Hipertensão, 11, 157-160.
- Yasmin and Brown, M.J. (1999) Similarities and Differences between Augmentation Index and Pulse Wave Velocity in the Assessment of Arterial Stiffness. QJM: An International Journal of Medicine, 92, 595-600. http://dx.doi.org/10.1093/qjmed/92.10.595
- Millasseau, S.C., Patel, S.J., Redwood, S.R., Ritter, J.M. and Chowienczyk, P.J. (2003) Pressure Wave Reflection Assessed from the Peripheral Pulse. Is a Transfer Function Necessary? Hypertension, 41, 1016-1020. http://dx.doi.org/10.1161/01.HYP.0000057574.64076.A5
- Crilly, M., Coch, C., Bruce, M., Clark, H. and Williams, D. (2007) Repeatability of Central Aortic Blood Pressures Measured Non-Invasively Using Radial Applanation Tonometry and Peripheral Pulse Wave Analysis. Blood Pressure, 16, 262-269. http://dx.doi.org/10.1080/08037050701464385
- Wohlfahrt, P., Wichterle, D., Seidlerová, J., Filipovský, J., Bruthans, J., Adámková, V. and Cífková, R. (2012) Relation of Central and Brachial Blood Pressure to Left Ventricular Hypertrophy. The Czech Post-MONICA Study. Journal of Human Hypertension, 26, 14-19. http://dx.doi.org/10.1038/jhh.2011.78
- Takazawa, K., Kobayashi, H., Shindo, N., Tanaka, N. and Yamashina, A. (2007) Relationship between Radial and Central Arterial Pulse Wave and Evaluation of Central Aortic Pressure Using the Radial Arterial Pulse Wave. Hypertension Research, 30, 219-228. http://dx.doi.org/10.1291/hypres.30.219
- Hayward, C.S., Kraidly, M., Webb, C.M. and Collins, P. (2002) Assessment of Endothelial Function Using Peripheral Waveform Analysis: A Clinical Application. Journal of the American College of Cardiology, 40, 521-528. http://dx.doi.org/10.1016/S0735-1097(02)01991-5
- Crilly, M., Coch, C., Bruce, M., Clark, H. and Williams, D. (2007) Indices of Cardiovascular Function Derived from Peripheral Pulse Wave Analysis Using Applanation Tonometry: A Measurement Repeatability Study. Vascular Medicine, 12, 189-197. http://dx.doi.org/10.1177/1358863X07081134
- Smulyan, H., Siddiqui, D.S., Carlson, R.J., London, G.M. and Safar, M.E. (2003) Clinical Utility of Aortic Pulses and Pressures Calculated From Applanated Radial-Artery Pulses. Hypertension, 42, 150-155. http://dx.doi.org/10.1161/01.HYP.0000084051.34269.A9
- Williams, B., Lacy, P.S., Thom, S.M., Cruickshank, K., Stanton, A., Collier, D., Hughes, A.D. and Thurston, H. (2006) Differential Impact of Blood Pressure-Lowering Drugs on Central Aortic Pressure and Clinical Outcomes. Principal Results of the Conduit Artery Function Evaluation (CAFE) Study. Circulation, 113, 1213-1225.
- Safar, M. (2004) Fatores Mecânicos Preditores do Risco Cardiovascular. Revista Brasileira de Hipertensão, 11, 175- 179.
- Pizzi, O., Brandão, A.A., Magalhães, M.E.C., Pozzan, R. and Brandão, A.P. (2006) Velocidade de Onda de Pulso—O Método e suas Implicações Prognósticas na Hipertensão Arterial. Revista Brasileira de Hipertensão, 13, 59-62.
- Najjar, S.S., Scuteri, A., Shetty, V., Wright, J.G., Muller, D.C., Fleg, J.L., Spurgeon, H.P., Ferrucci, L. and Lakatta, E.G. (2008) Pulse Wave Velocity Is an Independent Predictor of the Longitudinal Increase in Systolic Blood Pressure and of Incident Hypertension in the Baltimore Longitudinal Study of Aging. Journal of the American College of Cardiology, 51, 1377-1383. http://dx.doi.org/10.1016/j.jacc.2007.10.065
- Fischer-Rasokat, U., Brenck, F., Zeiher, A.M. and Spyridopoulos, I. (2009) Radial Augmentation Index Unmasks Premature Coronary Artery Disease in Younger Males. Blood Pressure Monitoring, 14, 59-67. http://dx.doi.org/10.1097/MBP.0b013e32832941ce
- Korhonen, P.E., Syvänen, K.T., Vesalainen, R.K., Kantola, I.M., Kautiainen, H., Järvenpää, S. and Aarnio, P.T. (2009) Ankle-Brachial Index Is Lower in Hypertensive than in Normotensive Individuals in a Cardiovascular Risk Population. Journal of Hypertension, 27, 2036-2043. http://dx.doi.org/10.1097/HJH.0b013e32832f4f54
- Wilkinson, I.B., Hall, I.R., Maccallum, H., Mackenzie, I.S., McEniery, C.M., Van der Arend, B.J., Shu, Y.E., Mackay, L.S., Webb, D.J. and Cockcroft, J.R. (2002) Pulse Wave Analysis. Clinical Evaluation of a Noninvasive, Widely Applicable Method for Assessing Endothelial Function. Arteriosclerosis, Thrombosis, and Vascular Biology, 22, 147-152. http://dx.doi.org/10.1161/hq0102.101770
- Fantin, F., Mattocks, A., Bulpitt, C.J., Bayana, W. and Rajkumar, C. (2007) Is Augmentation Index a Good Measure of Vascular Stiffness in the Elderly? Age and Ageing, 36, 43-48. http://dx.doi.org/10.1093/ageing/afl115
- Mota-Gomes, M.A., Feitosa, A.M., Brandão, M.C.B. and Chaves, H. (2006) Augmentation Index—Novo Preditor de Risco Cardiovascular. Revista Brasileira de Hipertensão, 13, 63-64.
- Gatzka, C.D., Kingwell, B.A., Cameron, J.D., Berry, K.L., Liang, Y.L., Dewar, E.M., Reid, C.M., Jennings, G.L., Dart, A.M. and the ANBP2 Investigators (2001) Gender Differences in the Timing of Arterial Wave Reflection beyond Differences in Body Height. Journal of Hypertension, 19, 2197-2203. http://dx.doi.org/10.1097/00004872-200112000-00013
- Sutton-Tyrrell, K., Najjar, S.S., Boudreau, R.M., Venkitachalam, L., Kupelian, V., Simonsick, E.M., Havlik, R., Lakatta, E.G., Spurgeon, H., Kritchevsky, S., Pahor, M., Bauer, D. and Newman, A., for the Health ABC Study (2005) Elevated Aortic Pulse Wave Velocity, a Marker of Arterial Stiffness, Predicts Cardiovascular Events in Well-Functioning Older Adults. Circulation, 111, 3384-3390. http://dx.doi.org/10.1161/CIRCULATIONAHA.104.483628
- Brewer, G.J. (2010) Epigenetic Oxidative Redox Shift (EORS) Theory of Aging Unifies the Free Radical and Insulin Signaling Theories. Experimental Gerontology, 45, 173-179. http://dx.doi.org/10.1016/j.exger.2009.11.007
- Giollo Jr., L.T., Mota-Gomes, M.A. and Martin, J.F.V. (2010) A Avaliação da Resposta Anti-hipertensiva com Tonometria de Aplanação. Revista Brasileira de Hipertensão, 17, 189-190.
- Kotsis, V., Stabouli, S., Karafillis, I. and Nilsson, P. (2011) Early Vascular Aging and the Role of Central Blood Pressure. Journal of Hypertension, 29, 1847-1853. http://dx.doi.org/10.1097/HJH.0b013e32834a4d9f
- Bellien, J., Favre, J., Iacob, M., Gao, J., Thuillez, C., Richard, V. and Joannidès, R. (2010) Arterial Stiffness Is Regulated by Nitric Oxide and Endothelium-Derived Hyperpolarizing Factor during Changes in Blood Flow in Humans. Hypertension, 55, 674-680. http://dx.doi.org/10.1161/HYPERTENSIONAHA.109.142190
- Weber, T., Ammer, M., Rammer, M., Adji, A., O’Rourke, M.F., Wassertheurer, S., Rosenkranz, S. and Eber, B. (2009) Noninvasive Determination of Carotid-Femoral Pulse Wave Velocity Depends Critically on Assessment of Travel Distance: A Comparison with Invasive Measurement. Journal of Hypertension, 27, 1624-1630. http://dx.doi.org/10.1097/HJH.0b013e32832cb04e
- Kovaite, M., Petrulioniene, Z., Ryliskyte, L., Badariene, J., Dzenkeviciute, V., Cypiene, A., Laucevicius, A., Polena, S. and Gintautas, J. (2007) Systemic Assessment of Arterial Wall Structure and Function in Metabolic Syndrome. Proceedings of the Western Pharmacology Society, 50, 123-130.
- Chen, C.H., Nevo, E., Fetics, B., Pak, P.H., Yin, F.C.P., Maughan, W.L. and Kass, D.A. (1997) Estimation of Central Aortic Pressure Waveform by Mathematical Transformation of Radial Tonometry Pressure. Circulation, 95, 1827- 1836. http://dx.doi.org/10.1161/01.CIR.95.7.1827
- Nichols, W.W. (2005) Clinical Measurement of Arterial Stiffness Obtained from Noninvasive Pressure Waveforms. American Journal of Hypertension, 18, 3S-10S. http://dx.doi.org/10.1016/j.amjhyper.2004.10.009
- Kohara, K., Tabara, Y., Oshiumi, A., Miyawaki, Y., Kobayashi, T. and Miki, T. (2005) Radial Augmentation Index: A Useful and Easily Obtainable Parameter for Vascular Aging. American Journal of Hypertension, 18, 11S-14S. http://dx.doi.org/10.1016/j.amjhyper.2004.10.010
- Shinohata, R., Nakatsu, T., Yuki, Y., Nishitani, A., Mashima, K., Toyonaga, S., Ogawa, H., Hirohata, S., Usui, S., Kitawaki, T. and Kusachi, S. (2008) Association of Augmentation Index of Radial Pressure Wave Form with Diurnal Variation Pattern of Blood Pressure in Untreated Patients with Essential Hypertension. Journal of Hypertension, 26, 535-543. http://dx.doi.org/10.1097/HJH.0b013e3282f2fdb6
- Khalegui, M. and Kullo, I.J. (2007) Aortic Augmentation Index Is Associated with Ankle-Brachial Index: A Community-Based Study. Atherosclerosis, 195, 248-253. http://dx.doi.org/10.1016/j.atherosclerosis.2006.12.017
- Crilly, M., Coch, C., Clark, H., Bruce, M. and Williams, D. (2007) Repeatability of the Measurement of Augmentation Index in the Clinical Assessment of Arterial Stiffness Using Radial Applanation Tonometry. Scandinavian Journal of Clinical & Laboratory Investigation, 67, 413-422. http://dx.doi.org/10.1080/00365510601131946
- Michel, T. and Vanhoutte, P.M. (2010) Cellular Signaling and NO Production. European Journal of Physiology, 459, 807-816. http://dx.doi.org/10.1007/s00424-009-0765-9
- Vanhoutte, P.M., Shimokawa, H., Tang, E.H.C. and Feletou, M. (2009) Endothelial Dysfunction and Vascular Disease. Acta Physiologica, 196, 193-222. http://dx.doi.org/10.1111/j.1748-1716.2009.01964.x
- Vanhoutte, P.M. and Tang, E.H.C. (2008) Endothelium-Dependent Contractions: When a Good Guy Turns Bad! Journal of Physiology, 586, 5295-5304. http://dx.doi.org/10.1113/jphysiol.2008.161430
- Furchgott, R.F. and Zawadzki, J.V. (1980) The Obligatory Role of Endothelial Cells in the Relaxation of Arterial Smooth Muscle by Acetylcholine. Nature, 288, 373-376. http://dx.doi.org/10.1038/288373a0
- Najjar, S.S., Scuteri, A. and Lakatta, E.G. (2005) Arterial Aging: Is It an Immutable Cardiovascular Risk Factor? Hypertension, 46, 454-462. http://dx.doi.org/10.1161/01.HYP.0000177474.06749.98
- Hope, S.A., Tay, D.B., Meredith, I.T. and Cameron, J.D. (2002) Comparison of Generalized and Gender-Specific Transfer Functions for the Derivation of Aortic Waveform. American Journal of Physiology. Heart and Circulatory Physiology, 283, H1150-H1156.
- O’Rourke, M.F. and Adji, A. (2010) Clinical Use of Applanation Tonometry: Hope Remains in Pandora’s Box. Journal of Hypertension, 28, 229-233. http://dx.doi.org/10.1097/HJH.0b013e328334cb2a
- Kips, J.G., Schutte, A.E., Vermeersch, S.J., Huisman, H.W., Van Rooyen, J.M., Glyn, M.C., Fourie, C.M., Malan, L., Schutte, R., Van Bortel, L.M. and Segers, P. (2011) Comparison of Central Pressure Estimates Obtained from SphygmoCor, Omron HEM-9000AI and Carotid Applanation Tonometry. Journal of Hypertension, 29, 1115-1120. http://dx.doi.org/10.1097/HJH.0b013e328346a3bc
- Murgo, J.P., Westerhof, N., Giolma, J.P. and Altobelli, S.A. (1980) Aortic Input Impedance in Normal Man: Relationship to Pressure Wave Forms. Circulation, 62, 105-116. http://dx.doi.org/10.1161/01.CIR.62.1.105
- Vlachopoulos, C., Aznaouridis, K., O’Rourke, M.F., Safar, M.E., Baou, K. and Stefanidis, C. (2010) Prediction of Cardiovascular Events and All-Cause Mortality with Central Haemodynamics: A Systematic Review and Meta-Analysis. European Heart Journal, 31, 1865-1871. http://dx.doi.org/10.1093/eurheartj/ehq024
- Safar, M.E., Blacher, J., Protogerou, A. and Achimastos, A. (2008) Arterial Stiffness and Central Hemodynamics in Treated Hypertensive Subjects According to Brachial Blood Pressure Classification. Journal of Hypertension, 26, 130- 137. http://dx.doi.org/10.1097/HJH.0b013e3282f16a9c
- Munir, S., Guilcher, A., Kamalesh, T., Clapp, B., Redwood, S., Marber, M. and Chowienczyk, P. (2008) Peripheral Augmentation Index Defines the Relationship between Central and Peripheral Pulse Pressure. Hypertension, 51, 112- 118. http://dx.doi.org/10.1161/HYPERTENSIONAHA.107.096016
- Miyashita, H. (2012) Clinical Assessment of Central Blood Pressure. Current Hypertension Reviews, 8, 80-90. http://dx.doi.org/10.2174/157340212800840708
- Cameron, J.D., McGrath, B.P. and Dart, A.M. (1998) Use of Radial Artery Applanation Tonometry and a Generalized Transfer Function to Determine Aortic Pressure Augmentation in Subjects with Treated Hypertension. Journal of the American College of Cardiology, 32, 1214-1220. http://dx.doi.org/10.1016/S0735-1097(98)00411-2
- Wilkinson, I.B., MacCallum, H., Flint, L., Cockcroft, J.R., Newby, D.E. and Webb, D.J. (2000) The Influence of Heart Rate on Augmentation Index and Central Arterial Pressure in Humans. Journal of Physiology, 1, 263-270. http://dx.doi.org/10.1111/j.1469-7793.2000.t01-1-00263.x
- Gedikli, O., Ozturk, S., Yilmaz, H., Baykan, M., Kiris, A., Durmus, I., Karaman, K., Karahan, C. and Celik, S. (2009) Low Total Antioxidative Capacity Levels Are Associated with Augmentation Index but Not Pulse-Wave Velocity. Heart and Vessels, 24, 366-370. http://dx.doi.org/10.1007/s00380-008-1129-7
- Boutouyrie, P. and Vermeersch, S.J. (2010) Determinants of Pulse Wave Velocity in Healthy People and in the Presence of Cardiovascular Risk Factors: “Establishing Normal and Reference Values”. The Reference Values for Arterial Stiffness’ Collaboration. European Heart Journal, 31, 2338-2350.
- Sociedade Brasileira de Cardiologia/Sociedade Brasileira de Hipertensão/Sociedade Brasileira de Nefrologia (2010) VI Diretrizes Brasileiras de Hipertensão. Arquivos Brasileiros de Cardiologia, 91, 1-51.
Acronyms
AI: augmentation index P1: ejection wave P2: reflected wave NO: nitric oxide
NOTES

*Corresponding author.

